The incidence of acute respiratory diseases (ARI) and their high prevalence in children are a serious problem for healthcare in Russia [1]. The pathological process during acute respiratory infection can involve both the upper and lower respiratory tracts. Etiological factors represent a polyetiological group of infections, among which in children the proportion of viruses is 65-90% [2-4]. The most common bacterial pathogens detected in acute respiratory infections in children are Str. pneumoniae, H. influenzae, Str. pyogenes, Staph, aureus, M. catarrhalis
[5]. The role of bacterial flora in the development of complications and recurrent respiratory diseases in frequently ill children is especially high [6].
In children, a complicated course of acute respiratory diseases is much more often recorded in the form of inflammatory diseases of the nasal cavity, pharynx, larynx, trachea, which have a recurrent course. Currently, the treatment of these diseases is effective when using, first of all, antiseptic agents in combination with symptomatic drugs [7, 8] and physical factors [9-11].
One of the pressing problems of modern physiotherapy is the development of technologies that allow the administration of drugs using hardware physiotherapy methods [12].
An effective method for treating diseases of the upper respiratory tract is aerosol therapy in the form of inhalation of medicinal substances that have higher chemical and physical activity than conventional liquid drugs due to an increase in the total surface of the dispersed phase.
In recent years, a new generation antiseptic, Miramistin, has been widely used, which has pronounced activity against a number of microbes - viruses, bacteria, fungi.
The purpose of the study was to scientifically substantiate the possibility of using Miramistin solution in children with acute respiratory diseases using physiotherapy technologies and increasing the effectiveness of complex treatment.
About medications in gynecology
Miramistin in gynecology how to use. Miramistin is a drug with antiseptic properties, used in the form of a solution and as an ointment. As a rule, a cotton swab is taken and soaked in the drug, after which it is inserted into the vaginal cavity.
This antiseptic drug has a special property; it acts extremely selectively, that is, it has a negative effect on the skin or mucous membrane. At the same time, it has an effect on pathogenic microorganisms and does not cause an allergic reaction in the patient.
Sometimes there is a slight burning sensation at the site of use of this product, but it goes away on its own in a short period of time and is absolutely safe, so the drug can be used in the future. Miramistin has a number of useful properties such as: increasing local immunity, anti-inflammatory effect and accelerated cell regeneration.
Like any antiseptic, Miramistin kills germs.
Miramistin solution 0.01% 50 ml with gynecological attachment in Lipetsk
Locally. The drug is ready for use. Instructions for using packaging with spray nozzle.
- Remove the cap from the bottle; Also remove the urological applicator from the 50 ml bottle.
- Remove the supplied spray nozzle from its protective packaging.
- Attach the spray nozzle to the bottle.
- Activate the spray nozzle by pressing again.
Surgery, traumatology, combustiology. For preventive and therapeutic purposes, the surface of wounds and burns is irrigated, wounds and fistula tracts are loosely tamponed, gauze swabs soaked in the drug are fixed. The treatment procedure is repeated 2–3 times a day for 3–5 days. A highly effective method of active drainage of wounds and cavities with a daily consumption of up to 1 liter of the drug.
Obstetrics, gynecology. In order to prevent postpartum infection, it is used in the form of vaginal irrigation before childbirth (5–7 days), during childbirth after each vaginal examination and in the postpartum period, 50 ml of the drug in the form of a tampon with an exposure of 2 hours for 5 days. For the convenience of vaginal irrigation, it is recommended to use the gynecological nozzle included in the kit. When women give birth by cesarean section, the vagina is treated immediately before the operation, the uterine cavity and the incision on it are treated during the operation, and in the postoperative period, tampons soaked in the drug are inserted into the vagina with an exposure of 2 hours for 7 days. Treatment of inflammatory diseases is carried out over a course of 2 weeks by intravaginal administration of tampons with the drug, as well as by the method of medicinal electrophoresis.
Venereology. For the prevention of sexually transmitted diseases, the drug is effective if it is used no later than 2 hours after sexual intercourse. Using a urological applicator, insert the contents of the bottle into the urethra for 2-3 minutes: for men - 2-3 ml, for women - 1-2 ml and in the vagina - 5-10 ml. For convenience, the use of a gynecological attachment is recommended. Treat the skin of the inner thighs, pubis, and genitals. After the procedure, it is recommended not to urinate for 2 hours.
Urology. In the complex treatment of urethritis and urethroprostatitis, 2-3 ml of the drug is injected into the urethra 1-2 times a day, the course is 10 days.
Otorhinolaryngology. For purulent sinusitis, during puncture the maxillary sinus is washed with a sufficient amount of the drug. Tonsillitis, pharyngitis and laryngitis are treated by gargling and/or irrigation using a spray nozzle, pressing 3-4 times 3-4 times a day. The amount of drug per rinse is 10–15 ml.
Children. In case of acute pharyngitis and/or exacerbation of chronic tonsillitis, the pharynx is irrigated using a spray nozzle. At the age of 3-6 years - 3-5 ml per irrigation (press the head of the spray nozzle once) 3-4 times a day; 7–14 years — 5–7 ml per irrigation (press twice) 3–4 times a day; over 14 years old - 10-15 ml per irrigation (3-4 times pressing) 3-4 times a day. The duration of therapy ranges from 4 to 10 days, depending on the timing of remission.
Dentistry. For stomatitis, gingivitis, and periodontitis, it is recommended to rinse the mouth with 10–15 ml of the drug 3–4 times a day.
About Medar
Now we will talk about our medical institution. Our medical center Medar has long been known both in Kazakhstan and abroad. We chose our beloved capital, Astana, as our location. How are we different from others, and what type of services do we provide? On our website you can find many articles on various medical topics.
We bring knowledge and health to people. From our articles you can learn about how various types of ultrasound scanning are done, what products are used to treat ailments in various fields of medicine. We are talking not only about well-known and widely used pharmacology, but also about less common folk methods.
Our doctors have received many awards and prizes, which is why Medar has outstanding treatment methods.
The prices in our clinic will pleasantly surprise you.
Results and discussion
Before the start of the study, 45 (78.3%) children complained of poor health and malaise. In 24 (40.0%) children, rhinitis was complicated by symptoms of catarrhal sinusitis: difficulty nasal breathing, heaviness and pain in the head, in the projections of the sinuses. During rhinoscopy, 17 (28%) children had mucopurulent discharge from the nose in the middle and lower nasal passages, 43 (72.0%) had mucous discharge, 29 (48.0%) patients had hyperemia and swelling of the nasal mucosa . During pharyngoscopy, redness of the pharyngeal mucosa and mucus flowing down the back wall of the pharynx were observed in 48.1% of cases. In children, along with a runny nose, there were signs of acute pharyngitis and laryngotracheitis (24.0%), which was accompanied by a sore throat and dry cough; in 55% of cases the cough was paroxysmal in nature. In 40% of cases, complaints were made of chest pain when coughing. In 26.7% of children with symptoms of tracheitis, the cough was accompanied by the separation of viscous mucous sputum.
The presence of acute inflammatory process activity in 41.7% of children with acute respiratory diseases was evidenced by leukocytosis up to 11.08±1.4·109/l in 62.5% of them and an increase in ESR on average to 16.2±1.45 mm/h in 79.2%.
When using inhaled miramistin solution in children with symptoms of nasopharyngitis, the cough became milder, less frequent after the 2nd day of treatment, in 75% of patients it completely disappeared by the end of the course; sputum discharge improved, nasal congestion decreased, and the amount of discharge from the nasal passages decreased.
In 40% of children with symptoms of laryngotracheitis, cough complaints decreased significantly after the 4th day of inhalation. Against the background of a decrease in the number of coughing episodes in children in the main group, a change in the nature of sputum was recorded - the viscosity decreased, and the discharge acquired a mucous character. The cough became moist, more productive, its intensity decreased, which was accompanied by a significant decrease in sore throat and pain in the chest during coughing attacks. In 25% of children, the cough stopped completely after the 5th day of treatment, in half (45%) of the children - after the 7th day, in the remaining patients - after the 10th day of inhalation.
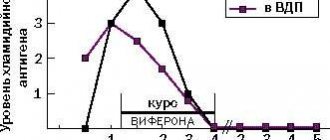
In the control group, the positive dynamics of clinical symptoms were less pronounced and occurred 3-4 days later ( Fig. 1
).
Under the influence of inhalation of Miramistin solution, favorable dynamics of the auscultatory picture were observed in the form of a decrease or disappearance of wheezing in the lungs after the 6th day of treatment in 65% of children with laryngotracheitis, in the remaining children - after the 8th day of inhalation. In the control group, the disappearance of wheezing was observed at a later date: in only 20% of children, wheezing disappeared by the end of the treatment course.
To assess the dynamics of subjective complaints, SAS was used. SAS data showed that by the end of the course of treatment, children of all groups had improved well-being and motor activity.
In children with symptoms of nasopharyngitis, nasal congestion, according to the SAS, decreased from 8.49±0.137 to 2.00±0 points, discharge from the nasal passages - from 9.25±0.155 to 2.00±0.10 points ( Fig. 2
).
In the control group, the dynamics of the severity of nasal congestion and nasal discharge decreased from 7.99±0.207 to 4.00±0.100 points and from 8.89±0.266 to 4.92±0.140 points, respectively ( Fig. 3
).
According to SAS data, after the first inhalation of miramistin solution in children with symptoms of laryngotracheitis, the intensity of cough decreased (from 9.30±0.179 to 7.70±0.193 points), weakness significantly decreased and performance increased. A significant decrease in subjective symptoms in children with symptoms of laryngotracheitis in the main group was noted after the 4th day of inhalation. In 2 children who received treatment for 10 days, by the end of treatment the severity of subjective symptoms decreased to 1 point ( Fig. 4
).
In the control group, the severity of subjective symptoms decreased gradually and by the end of the observation remained at an average level of 5.7 points.
Based on the studies conducted, a positive effect of inhalation of miramistin solution on peripheral blood parameters in children with acute respiratory infections who had initially reduced hemogram values was established, characterized by normalization of the leukocyte count and ESR in all children, which indicates an anti-inflammatory effect.
Analysis of the flow-volume curve data showed that at the beginning of the study, 70% of patients with complicated tracheitis had an average decrease in respiratory function below the age norm (POS - 69.24±0.23% D, FEV1 - 75.45± 0.67%D).
Under the influence of inhalation of miramistin solution, a tendency towards an increase in reduced indicators was noted (POS up to 73.02±0.34%D and FEV1 up to 82.36±0.41%D), but no significant dynamics were identified.
In children of the control group who received miramistin in the form of a spray, indicators of external respiration function remained at the same level.
During the study, daily monitoring of peak expiratory flow (PEF) was carried out in children with symptoms of tracheitis, which made it possible to monitor the state of external respiration and evaluate the effectiveness of the therapy. The initial PEF values in 25% of these children were below the age norm. In the course of the study, under the influence of inhalation of miramistin solution, a tendency was noted to increase the average PEF values after the 5th inhalation in almost half (45%) of children (from 66.79±0.76 to 74.22±0.62%D) , by the end of the course there was a significant increase in indicators to 78.35±0.89%D ( p
<0.05).
In children who received miramistin in the form of a spray, similar dynamics of PEF indicators were not recorded, which indicated a more pronounced positive effect of inhalations ( Fig. 5
).
Analysis of the initial level of physical fitness of school-age children with acute respiratory infections revealed a decrease in the degree of development of speed-strength capabilities in 70% of children, and a decrease in the level of development of strength capabilities in 80%.
Data from a repeated study of the functional state of the muscular system in all children after recovery indicated positive dynamics in speed-strength indicators of physical fitness (standing long jump, dynamometry).
A comprehensive assessment of the effectiveness showed a significantly higher therapeutic effectiveness of inhalation of Miramistin solution (87.5%) than when using Miramistin in the form of a spray (75.0%, p
<0.05), due to an increase in the pharmacotherapeutic activity of the drug due to an increase in the total volume of the drug suspension and the contact surface of the aerosol obtained using a nebulizer.
Douching with an antiseptic
An antiseptic can also be used for douching. Is it worth doing this procedure before you visit a gynecologist? Definitely not. In this case, the doctor will not be able to conduct a full examination if you clean the vagina of bacteria.
In this case, making a correct diagnosis will be extremely difficult. For douching you will need a douche bulb, or an ordinary Esmarch mug. Rubber tubes or a syringe must be thoroughly disinfected with alcohol, and then rinsed with boiled water.
The tips of the Esmarch mug are usually boiled. You must be sure that the medical instruments are completely sterile.
This procedure must be carried out extremely carefully.