The symptoms and treatment of mastitis are inextricably linked. Timely identification of signs will allow you to quickly identify and eliminate the inflammatory disease occurring in the breast tissue. In case of late consultation with a doctor and improper therapy, purulent mastitis may develop, requiring surgical intervention. Therefore, it is important to know the first signs and symptoms of the disease, the causes of its occurrence, in order to prevent serious consequences.
Causes of mastitis
In most cases, mastitis in women is provoked by a staphylococcal infection, which enters the ducts of the mammary glands and actively develops there. The most common causes of mastitis are the following:
- of chronic diseases in the body , including infections of the respiratory tract, reproductive system, etc.;
- Acute intestinal infections , when the stick enters the mammary glands through the circulatory system;
- Cracked nipples . Even microscopic lesions are vulnerable to infection;
- Lactostasis . Stagnation of milk in the gland encourages the proliferation of pathogenic organisms;
- Weakened immunity caused by recent childbirth or the presence of concomitant diseases;
- Failure to comply with basic hygiene rules.
If you have one of the listed factors, you need to pay special attention to your health and conduct regular breast examinations. To reduce the likelihood of mastitis, you should exclude its possible causes.
Mastitis in nursing women
Most often, breastfeeding women suffer from mastitis. Refusal to breastfeed or irregular pumping causes stagnation of milk in the glands. As a result, a favorable environment for the proliferation of microorganisms is created.
The first signs of mastitis may appear as early as the second week of breastfeeding or during weaning. However, mastitis in a nursing woman also occurs at other stages. Milk is rich in nutrients, making the infection develop very quickly. Even short-term disruptions in feeding the baby and expressing milk can cause mastitis.
Read more: Symptoms of mastitis in a nursing mother.
Mechanism of disease development
Pathogenic microorganisms enter the woman’s mammary gland through blood or microcracks in the nipples. After this, the pathogens begin to actively multiply and secrete waste products that have a detrimental effect on the human body. As a result, the first symptoms of mastitis appear in the form of fever and general malaise.
The immune system responds to the inflammatory process by producing white blood cells designed to suppress the source of infection. This is accompanied by dilation of blood vessels and the appearance of characteristic signs of mastitis.
How does the disease begin?
Mastitis develops after infection enters through the nipple opening. As a result of infection, pathogenic microorganisms settle on the wall of the duct. When milk stagnates, favorable conditions are created for the reproduction and growth of colonies, which gradually causes the death of gland cells.
The disease goes through three stages:
- Serous-infiltrative – acute mastitis begins with it. The affected tissues swell, and there is an accumulation of leukocytes - protective cells for destroying microbes. All pathological processes at this stage are still reversible.
- Stage of phlegmon - if the pathogen is not destroyed, the colonies infect new tissues, causing the death of entire areas. There is limited accumulation of pus.
- Gangrene develops if left untreated. It is characterized by blockage of large vessels with blood clots or their compression by growing purulent foci. Due to poor circulation, most of the gland dies.
Stages
Mastitis is divided into several stages, which are characterized by certain symptoms and signs. The main classification of mastitis is as follows:
- Serous is the initial stage of the disease, which responds well to treatment. At this stage, it is important to recognize the first symptoms: a slight inflammation forms, without visible changes on the skin. In this case, there is an enlargement of the mammary gland, pain and an increase in temperature.
- Infiltrative - occurs two days after the lack of proper treatment for serous mastitis. The area of inflammation increases, and upon palpation you can feel a pronounced compaction (infiltrate).
- Purulent - at this stage, purulent formations appear, causing a significant increase in temperature to 40 degrees and a sharp deterioration in well-being. The breasts become swollen, and the skin in the area of the mammary gland changes color.
- Chronic – occurs due to improper treatment or lack thereof. In most cases, this is untreated mastitis of the mammary gland, which subsequently responds poorly to therapy.
In addition to those described, there are also several other classifications of mastitis:
- Abscess – characterized by the presence of a purulent formation that is localized in a certain area and does not extend beyond its limits.
- Phlegmonous is one of the advanced forms of purulent mastitis, when inflammation spreads throughout the mammary gland.
- Gangrenous – a severe stage at which tissue necrosis occurs. The woman feels a sharp deterioration in her health, and her body temperature can rise above forty degrees. These symptoms require immediate hospitalization.
It is worth noting that mastitis in a nursing mother develops very intensively. In just a few hours, the disease can progress to the next stage. Therefore, when the first symptoms appear, you need to contact a clinic where professional help will be provided.
How to prevent it?
The main task of prevention is to ensure the natural drainage function of the mammary gland - this will prevent stagnation of milk and create a favorable emotional background. We list the basic rules that must be followed to prevent the development of mastitis:
- Immediately after birth you need to breastfeed - it is advisable to do this in the first 30 minutes. In the future, feeding should be continued, strictly observing the daily routine.
- Always express the remaining milk - place your fingers around the periphery of the areola, do not pull on the breast or pinch the skin. Alternate these movements with a light massage.
- Wear only a loose bra made from natural fabrics - the seams should not dig into the skin. If there is discharge from their nipple, use special wipes.
- Do a light breast massage every day - gently, in a circular motion. The procedure should last 5-10 minutes.
- If sores appear on the nipple, you should immediately consult a doctor. The doctor will prescribe medications for healing and special creams.
The best prevention is timely attendance at antenatal clinics and breast care. If you adhere to all of the above rules, the likelihood of developing pathology is very low. When symptoms of mastitis appear, urgent conservative therapy is required.
Symptoms of mastitis
Unlike many diseases, mastitis is characterized by the appearance of pronounced symptoms even at an early stage. This allows you to consult a doctor in a timely manner and undergo a course of therapy to prevent further development of the infection. Among the main symptoms are:
- pain in the affected area;
- increase in breast size;
- breast lump;
- malaise and weakness;
- headache;
- increased body temperature;
- change in skin color in the breast area;
- deterioration of milk flow;
- swelling of the skin of the breast;
Each stage of the disease is characterized by certain signs of mastitis. At the initial stage, thickening of the mammary gland and an increase in body temperature appear. These symptoms are enough to suspect the disease and undergo a professional examination to make an accurate diagnosis.
Types and forms of mastitis
There are acute and chronic forms of the disease. The first includes lactation or postpartum mastitis with pronounced symptoms. An example of the second is a non-lactation type of pathology, which is not associated with the period of breastfeeding and is not clearly linked to gender and age.
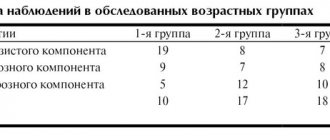
On a note! According to statistics, lactation mastitis occurs on average in 5% of lactating women. In unfavorable regions, this figure can rise to 15%. Moreover, 85% of all cases of the disease occur in first-time mothers. Non-lactation mastitis is less common (no more than 10% of the total number of all manifestations of mastitis) and can affect women of different ages, men, and children.
There are 3 clinical forms of the disease:
- Acute postpartum – develops against the background of congestion in nursing women.
- Plasma cell - more typical for multiparous women in the period after the end of lactation, as well as during hormonal changes during menopause. The disease occurs in a moderately acute form, with mild symptoms, which makes it similar to tumor pathologies of the mammary gland
- Neonatal mastitis – observed in infants of both sexes as a result of residual effects of maternal hormones (is a complication of physiological mastopathy in newborns).
On a note! Separately, it is worth mentioning cases of mastitis in men, which are considered a direct consequence of chronic endocrine diseases and hormone imbalance. The pathology manifests itself in the presence of diabetes mellitus, gynecomastia, tumors of the genital organs, as well as with long-term use of steroids in bodybuilders.
Depending on the nature of the inflammation, there are several types of mastitis:
- serous;
- infiltration;
- purulent.
Together they form 3 successive stages of development of the inflammatory process - from the appearance of the first symptoms in the form of serous exudate to active suppuration of the area of inflammation with the discharge of pus. Based on the type of localization of purulent structures, two more forms can be distinguished:
- phlegmonous - with the spread of pus throughout the entire volume of the affected tissue;
- abscess - with clear localization and delimitation of purulent contents from adjacent tissues.
In advanced cases, a gangrenous form may develop with tissue necrosis and septic complications, which poses a high risk to the patient’s life. The only way out in this situation is complete removal of the mammary gland and adjacent lymph nodes.
Diagnostics
Diagnostics plays an important role, since timely identification of the problem will allow for effective therapy and quickly eliminate the inflammatory process. The patient must carry out the initial diagnosis independently. This will allow you to identify the first symptoms of mastitis, suspect the presence of the disease and seek help from specialists.
When visiting a doctor, an examination is carried out and complaints are identified. The specialist palpates the breast, which allows you to make a diagnosis and determine a list of further examinations to determine effective treatment tactics.
Depending on the situation, the patient may be prescribed the following tests:
- general blood analysis;
- discharge from the nipples, to identify the causative agent of infection and sensitivity to antibiotics;
- examination of milk for the presence of bacteria and leukocyte levels.
To accurately determine the location of inflammation, as well as its extent, an ultrasound examination is performed. If the clinical picture is questionable, a biopsy is prescribed to rule out the possibility of cancer. The list of studies may vary and depend on factors such as the presence of concomitant diseases, the stage of mastitis, and so on.
Treatment of mastitis
Treatment methods depend entirely on the stage of mastitis and the woman’s health condition. It is worth noting that mastitis progresses very quickly and requires qualified treatment. Trying to cope with the disease on your own can lead to serious consequences.
The initial stage of the disease allows you to achieve high results using conservative treatment methods. These include taking anti-inflammatory medications and regularly expressing breast milk (in the case of lactation mastitis). In case of weakened immunity, the doctor prescribes antibiotics. During this period, it is recommended to stop breastfeeding, as taking medications can affect the composition of milk.
To minimize the likelihood of relapse, during the treatment period it is necessary to eliminate the factors that led to the development of mastitis. For example, ensure regular expression of milk.
Treatment of mastitis in women should be carried out under the supervision of specialists. In the absence of a positive result and the formation of suppuration, surgical intervention will be required. Removal of an abscess can be carried out by puncture or opening with subsequent drainage.
After the operation, a course of antibacterial therapy and painkillers is prescribed. If the disease occurred during lactation, then breastfeeding can be resumed only after stopping the medication and complete recovery. To ensure the effectiveness of the therapy, the patient is scheduled to undergo repeated tests.
Read more: Treatment of mastitis in a nursing mother.
How to treat?
Treatment for mastitis requires mandatory cessation of breastfeeding, since Staphylococcus aureus can cause dangerous diseases in the child. You also need to remember that any medicine penetrates the glandular tissue, and then into the milk.
At the initial stages, conservative therapy is prescribed. It includes:
- Drugs to reduce lactation (Dostinex, Bromocriptine) are prescribed by a doctor to relieve the strain on the mammary gland. When taking them, breastfeeding is strictly prohibited.
- Expressing breast milk - done 4-5 times a day, the procedure begins with the sore breast. For severe pain, a novocaine blockade is first done.
- Analgesics (Nise, Ibuprofen) or antispasmodics (Papaverine, No-Shpa) are prescribed for severe local symptoms. Medicines help cope with the manifestations of pathology.
- Antibiotics for mastitis (Clarithromycin, Erythromycin) are prescribed by a doctor when Staphylococcus aureus is detected. Taken in courses along with painkillers.
In case of phlegmonous form or in the presence of an abscess, surgery is prescribed. During surgery, purulent foci are opened, drainage of the contents is performed, followed by disinfection. In case of gangrene, the entire gland must be removed. After the intervention, a course of antibiotics is indicated.
Recommendations
Breast mastitis requires immediate action and adequate treatment. To achieve a speedy recovery and not harm your health, you need to adhere to the following recommendations:
- Treatment of mastitis should be trusted only to qualified specialists. Independent actions can lead to negative consequences and the transition of the disease to a more complex stage.
- To achieve effective results, you cannot ignore the recommendations of your doctor.
- When identifying the first signs of mastitis, you need to refrain from thermal procedures and regularly express milk.
Only professional treatment of mastitis will help get rid of the inflammatory process and avoid its reappearance.
Prevention
It is almost impossible to completely exclude the possibility of the disease. However, you can reduce it to a minimum. To do this, it is enough to carry out a number of preventive measures:
- It is necessary to breastfeed regularly, as well as express the remaining milk after each procedure.
- When feeding, you need to properly attach the baby to the breast. The baby should be able to grasp the entire areola. This prevents damage to the delicate skin of the nipples.
- Timely treatment of inflammatory processes occurring in the body also reduces the chances of mastitis.
- Before and after each feeding, you need to prepare your breasts. The nipples are washed with warm water and then gently wiped with a clean towel.
Preventive measures also include self-examination of the mammary glands and regular visits to a specialist.
Is it possible to continue breastfeeding with mastitis?
With mastitis, the infection does not get into the milk, and it cannot harm the baby. And although breastfeeding with mastitis can be painful for mom, try not to stop breastfeeding. The more often the baby suckles at the breast where congestion has occurred, the faster it will be eliminated. You also need to continue feeding to strengthen the baby’s immunity, since breast milk has antibacterial properties.
Rarely, but sometimes breastfeeding with lactation mastitis can be too painful. Then try placing your baby on the healthy breast, and place a cloth or small towel under the breast with mastitis to absorb the dripping milk. Perhaps, after the sore breast is partially emptied, the pressure will decrease and feeding from it will not be so painful. You can also try expressing milk and feeding your baby or saving it for the future.
The discomfort of mastitis can be frustrating and discourage breastfeeding. But with timely treatment, the symptoms of mastitis quickly disappear, and mother and baby can again enjoy the benefits and process of breastfeeding.