Acromegaly is a pathology that manifests itself in an increase in the size of certain parts of the body; it is associated with increased production of growth hormone (somatotropin), which occurs as a result of tumor damage to the pituitary gland.
This phenomenon occurs in adult patients, its features are growth of the lower jaw, lips, ears, nose, growth of hands, feet, pain in the joints and head, interruptions in reproduction in females and males.
Elevated hormonal levels provoke premature death from heart, vascular, pulmonary and cancer diseases. Progression of acromegaly occurs after overall growth of the body stops. Little by little, over a long period of time, an increase in symptoms occurs, which is accompanied by changes in appearance. On average, the disease is diagnosed 7 years after its actual onset. Acromegaly can be found equally in both men and women; the age of patients is predominantly 40-60 years.
Causes and symptoms of acromegaly
Pituitary adenoma:
- Monoclonal tumor (somatotropinoma).
- Mixed adenoma - in addition to GH, prolactin, TSH, ACTH, LH, FSH can be produced.
- Ectopic tumor from cells of the APUD system, producing GH or somatoliberin:
- tumors with an endocranial location (in the pharyngeal or sphenoidal sinus);
- tumors with extracranial location (in the lungs, mediastinum, gonads, intestines).
Iatrogenic factors. Genetically determined endocrinopathies:
- MEN-1 syndrome (multiple endocrine neoplasia) - primary hyperparathyroidism, islet cell tumors, adenohypophysis tumors. Carcinoid tumors of the digestive tract, multiple facial angiofibromas, collagenomas, subcutaneous and visceral lipomatosis, melanomas, leiomyomas of the esophagus, lungs, rectum, uterus;
- McCune-Albright syndrome - osteofibrous dysplasia, local dermopathy (appearance of café-au-lait spots on the skin), pituitary tumor;
- Carney complex - mixed (GH-prolactin-secreting) tumors, cardiac myxoma, patchy skin pigmentation, nodular adrenal dysplasia, schwannomas, etc.;
- isolated familial acromegaly - registered when 2 or more cases of acromegaly (gigantism) are detected in a family in the absence of signs of MEN 1 or Carney complex. It is distinguished by the early onset of the disease, more frequent development in men and rapid growth of adenomas.
Somatotropic hormone (somatotropin, somatropin, growth hormone)
A peptide hormone secreted by adenohypophysis cells. The main function is to stimulate the growth and development of the body. Has an anabolic effect, enhancing protein synthesis; participates in the regulation of carbohydrate metabolism, being an insulin antagonist, etc. Most of the effects of GH are mediated by the participation of insulin-like growth factors, mainly IGF-1, synthesized in the liver and to a lesser extent in target organs. The hypothalamic releasing factor somatoliberin has a stimulating effect on the production of growth hormone, and the hypothalamic hormone somatostatin suppresses the production of growth hormone.
Clinical manifestations associated with endocrine and metabolic disorders
- Diffuse or nodular enlargement of the thyroid gland associated with excess GH and increased renal clearance of iodine. Secondary hypothyroidism may develop;
- Secondary hypogonadism due to a lack of gonadotropin production or concomitant hyperprolactinemia: women - menstrual irregularities such as oligo- and amenorrhea, galactorrhea, infertility; men - gynecomastia, decreased libido, erectile dysfunction;
- Development of insulin resistance and compensatory hyperinsulinemia, direct lipolytic effect of growth hormone, impaired glucose tolerance or diabetes mellitus;
- Pathology of phosphorus-calcium metabolism - hypercalciuria (nephrolithiasis), increased levels of inorganic phosphorus in the blood serum.
The loss of calcium in the urine is compensated by the acceleration of its absorption through the gastrointestinal tract due to increased PTH production. Acromegaly can be combined with hyperparathyroidism and parathyroid adenomas.
Clinical manifestations of the musculoskeletal system, skeletal muscles
- Disproportional enlargement of the hands and feet (pasty hands and feet), thickening of the fingers (cigar fingers);
- Pain and decreased mobility in the joints due to the development of secondary osteoarthropathy (bone growth, joint deformation);
- Spinal deformation of the kyphoscoliosis type with the formation of osteophytes and the development of radicular pain;
- Osteoporosis and osteopenia;
- Muscle weakness. Primary hypertrophy of muscle tissue is gradually replaced by proximal myopathy; patients are concerned about muscle weakness and decreased tolerance to physical activity.
Clinical manifestations of internal organs
- Splanchnomegaly (increase in the mass of all internal organs). As the disease progresses, functionally active connective tissue is replaced with the development of multi-organ sclerotic changes and organ failure;
- Changes in the cardiovascular system:
- angiopathy associated with sclerotic changes;
- cardiosclerosis;
- acromegalic cardiomyopathy - concentric hypertrophy is replaced by dilated cardiomyodystrophy with the development of progressive heart failure;
- rhythm and conduction disturbances, valvular disorders due to ventricular hypertrophy;
- arterial hypertension caused by sodium and water retention, decreased production of atrial natriuretic peptide, insulin resistance, increased vascular tone;
- Changes in the respiratory system:
- macroglossia. Often the development of obstructive sleep apnea, as a consequence, chronic hypoxia. Thickening of the vocal cords and the appearance of a characteristic low, rough voice;
- pneumosclerosis;
- emphysema;
- development of pulmonary heart failure;
Clinical changes in the nervous system
- Loss of pain and tactile sensitivity of the fingers of the extremities, the appearance of paresthesia due to compression of the median nerve in the deformed carpal canal, as well as segmental demyelination of peripheral nerves;
- Headache;
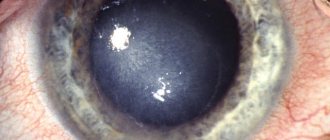
- Narrowing of visual fields, swelling and atrophy of the optic discs;
- Anosmia;
- Diencephalic epilepsy;
- Hydrocephalus;
- Hypopituitarism;
- Hypothalamic disorders - fever, eating disorders, changes in sleep/wake patterns;
- Diabetes insipidus;
- Damage to the III-VI pair of cranial nerves with the development of ptosis, diplopia, pupillary dysfunction, ophthalmoplegia, facial analgesia, pain along the trigeminal nerve, and hearing loss.
Other manifestations
- A characteristic change in facial features due to enlargement of the brow ridges, cheek bones, lower jaw, hypertrophy of soft tissues (nose, lips, ears);
- Hardening and thickening of the skin, hyperpigmentation, most often in the area of skin folds. Often - hypertrichosis, hirsutism, oily seborrhea, acne vulgaris, acanthosis nigricans (acanthosis nigricans, a type of papillary pigmentary dystrophy of the skin), increased humidity (overproduction of the sebaceous and sweat glands);
- The proliferative and antiapoptotic effects of GH and IGF-1 lead to an increased risk of developing benign and malignant neoplasms. Thus, the prevalence of thyroid cancer, breast cancer and colorectal cancer is significantly higher than similar indicators in the general population.
Stages
There are 4 stages of acromegaly:
- preacromegaly;
- hypertrophic;
- tumor;
- cachectic.
The first stage is diagnosed extremely rarely due to the mild severity of the symptoms characteristic of acromegaly.
At the hypertrophic stage, acromegaly can be recognized by the enlargement of individual organs, changes in facial contours and protrusion of the lower jaw. Characteristic features at this stage include deepening of the voice, increased body weight, and visual impairment. There are frequent cases of increased sweating due to the fact that the sweat glands also increase in size. General weakness and headaches are also included in the clinical picture of hypertrophic acromegaly.
At the tumor stage, the patient develops increased intracranial pressure. The consequence of this may be severe headaches, decreased hearing and vision. The tumor stage of acromegaly is often accompanied by muscle atrophy and weakness.
The outcome of the disease is considered to be the cachectic stage. This is complete exhaustion that develops in the absence of therapy.
Severity of acromegaly
- Mild - tolerance to normal physical activity remains, but there may be restrictions in performing heavy physical activity. Hospitalization is not required;
- Average - maintaining the ability to self-service, the inability to perform any work. Activity - 50% of waking time;
- Severe - restrictions on self-care and any other activities. The patient remains in bed or sits (inactive) more than 50% of the time he is awake.
Folk remedies
Acromegaly is caused by a tumor that changes the level of hormones in the body. Folk remedies cannot affect the development, progression and activity of the tumor, so they are not used in practice. Attempts to refuse the help of official medicine and treat pituitary adenoma using traditional recipes can lead to a deterioration in the patient’s condition and the development of serious complications.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
SEARCH FOR TREATMENT AROUND THE WORLD WITH YELLMED
Treatment of acromegaly
Surgical treatment (first-line therapy):
Removal of a pituitary tumor through a transnasal-transsphenoidal approach using endoscopic techniques. In the presence of giant tumors with massive invasion into the cavity and structure of the base of the skull, a two-stage intervention is possible: transcranial removal of the intracranial part, after 2-3 months - transnasal resection of the remainder of the adenoma.
Drug treatment
Somatostatin analogues:
- octreotide - administered subcutaneously 3 times a day. Single dose 100-200 mcg;
- Extended release octreotide - administered deep intramuscularly at an initial dosage of 20 mg every 28 days. If necessary, the dose is increased by 10 mg (up to 30-40 mg) with the same frequency of administration;
- Lanreotide is prescribed at an initial dose of 30 mg every 14 days deep intramuscularly. The dosage is increased by decreasing the intervals between drug administrations (every 7-10 days).
Dopamine agonists - currently, preference is given to selective long-acting agonists of type 2 dopamine receptors:
- cabergoline -1.0-3.5 mg/week;
- quinagolide - 0.3 mg/day.
GH receptor inhibitor (pegvisomant, not registered in the Russian Federation) is a genetically engineered analogue of endogenous IGF with amino acid substitutions, preventing the peripheral effects of GH overproduction.
Radiation therapy
Fractionated radiotherapy and stereotactic radiosurgery are currently used. After irradiation, normalization of GH and IGF levels occurs after 5-10 years or more. Due to the delayed effect of remission and the high risk of complications, radiation therapy is used only if surgical and/or drug treatment is ineffective.
Recommendations for further patient management
Annual clinical, instrumental (CD-graphy of the lungs, MRI of the pituitary gland, ultrasound of the thyroid gland, EchoCG, etc.) and laboratory (GH level, IGF-1) examination to assess the production of GH, the severity of somatic changes and the need for correction of therapy.
Characteristics of the main drugs for the treatment of acromegaly
| Somatostatin analogues | Dopamine agonists | GH receptor inhibitors | |
| Indications | Primary therapy for contraindications to surgical treatment. Secondary therapy for non-radical adenomectomy. The need for preoperative preparation to improve somatic status and reduce the risk of complications. Component of combination therapy. | ||
| Monitoring and correction of therapy | Every 3 months, control the levels of growth hormone and IGF. If there is clinical improvement within 3 months, the content of growth hormone and/or IGF has decreased by more than 30% of the initial level, treatment is considered effective and is continued. Otherwise, the patient is considered refractory to treatment with somatostatin analogues and other therapies are considered. Dose adjustment: Clinical improvement STH -1-2.5 ng/ml, IGF - within reference values - the dose remains the same; STH>2.5 ng/ml, IGF - outside the reference values - increase the dose of the drug; STH <1.0 ng/ml, IGF - within reference values - dose reduction. | ||
| Selection conditions | In combination with surgical treatment (pre and/or postoperative stage) Primary therapy in the absence of direct indications for surgical intervention (absence of chiasmatic or diaphragmatic syndrome), in the presence of contraindications to neurosurgical intervention, in the event of the patient’s refusal to undergo surgery. | Mixed pituitary adenomas producing GH and prolactin (somatoprolactinomas, mammosomatotropinomas). They are most effective in patients with a slight increase in GH levels and an increase in IGF-1 levels less than 2 times the upper limit of normal. | Lack of effect or intolerance to somatostatin analogues after non-radical selective adenomectomy. |
Criteria for monitoring the course of acromegaly
| Controlled disease | Active disease |
|
|
Diagnostics
Photo: krasnayakrov.ru
Diagnosing acromegaly is quite simple, especially in the later stages, since its external manifestations are specific. However, there is a certain category of diseases whose symptoms are in many ways similar to those of acromegaly. To carry out differential diagnosis and confirm (or exclude) the presence of acromegaly, a consultation with an endocrinologist is prescribed, as well as visual, laboratory and instrumental methods for diagnosing acromegaly.
Visual examination of the patient
Before prescribing the necessary diagnostic procedures and proper treatment, the doctor collects anamnesis, determines the hereditary predisposition to the development of this disease, and also conducts an objective examination - palpation, percussion, auscultation. Based on the results of the initial examination, the necessary diagnostic procedures are prescribed.
Laboratory diagnostic methods
To diagnose acromegaly, traditional laboratory research methods are used: blood and urine tests. However, the most informative and therefore frequently used of them are considered to be the determination of hormones in the blood for acromegaly: STH - somatotropic growth hormone, and insulin-like growth factor - IGF-1.
Determination of the level of growth hormone
Confirmation of the development of gigantism or acromegaly is an increased level of somatotropin in the blood - growth hormone, which is produced by the anterior lobe of the pituitary gland. A distinctive feature of the production of growth hormone is its cyclical nature, therefore, to conduct a test to determine its level, multiple blood sampling is practiced:
- in the first case, three samples are taken with an interval of 20 minutes, after which the serum is mixed and the average level of growth hormone is determined;
- in the second case, blood is drawn five times with an interval of 2.5 hours, but the level is determined after each portion of blood is received. The final indicator is obtained by averaging all values.
Confirmation of the diagnosis of acromegaly is possible when the hormone level exceeds 10 ng/ml. The disease can be excluded if the average value does not exceed 2.5 ng/ml.
Determination of IGF-1 level
Another informative screening test is to determine the level of the hormone IGF-1. It has high sensitivity and specificity, since it does not depend on daily fluctuations, like somatotropin. If the level of IGF-1 in the blood is higher than normal, the doctor may diagnose acromegaly. However, this test should be carried out in conjunction with other studies, since the IGF-1 value may change under the influence of certain factors:
- be reduced in case of liver dysfunction, hypothyroidism, excess estrogen, fasting;
- be increased as a result of hormone replacement therapy, as well as with an increase in insulin levels in the blood.
Glucose tolerance test
In case of doubtful results, a test for determining GH using glucose is performed to clarify the diagnosis. To carry it out, the basal level of somatotropin is measured, after which the patient is offered to take a glucose solution. In the absence of acromegaly, a glucose test shows a decrease in GH secretion, and with the development of the disease, on the contrary, its increase.
Instrumental diagnostic methods
To clarify the diagnosis of acromegaly and identify the nature of its origin, the doctor often resorts to instrumental diagnostic methods.
CT or MRI
The main and highly informative diagnostic method is CT or MRI, which allows you to identify the pituitary adenoma, as well as the degree of its spread to regional organs and tissues. The procedure is carried out using a contrast agent, which accumulates in the changed tissues, which simplifies the research procedure and allows one to determine characteristic changes in the pituitary gland or hypothalamus.
During the diagnostic process, many patients are interested in how often an MRI should be done for acromegaly. This procedure is usually carried out at the stage of hypertrophy of individual parts of the body, full-blown clinical manifestations, and later, at the tumor stage, when the patient complains of increased fatigue, headaches, muscle and joint pain, as well as other accompanying manifestations.
X-ray of the skull
This procedure is performed in order to identify characteristic radiological manifestations of acromegaly, as well as signs of the development of pituitary adenoma:
- increasing the size of the sella turcica;
- development of osteoporosis;
- increased pneumotization of the sinuses;
- double-circuit walls.
During radiography in the early stages of the disease, these signs may be absent, so other, often auxiliary, diagnostic methods are prescribed:
- radiography of the feet, which allows you to determine the thickness of the soft tissues in this area;
- Examination by an ophthalmologist to detect swelling, stasis and atrophy of the optic nerves, which often leads to blindness.
If necessary, the patient is prescribed an examination to identify complications: diabetes mellitus, intestinal polyposis, nodular goiter, adrenal hyperplasia, etc.
Forecast
Acromegaly in the absence of therapy is characterized by a progressive course with the development of organ disorders, early disability and premature death (mortality compared to the general population indicator is 2-2.5 times higher; without treatment, patients die 10 years earlier than healthy people). The younger the patient is at the time of the onset of the disease, the more aggressive growth the tumor is characterized by and the higher its functional activity. When it debuts at the age of over 50 years, the tumor grows more slowly and has less hormone-producing activity.
Danger of disease
If acromegaly is not treated promptly, it can lead to severe complications and death. Approximately half of patients die before the age of 50 years. Moreover, the overwhelming number of deaths with acromegaly (60%) are associated with cardiovascular complications. Another quarter consists of pulmonary-respiratory complications and 15% - the development of oncological processes, most often of the digestive system.
The danger of acromegaly is that it often goes unrecognized. The rarity of this disease, as well as the gradual development of changes in appearance over a long period, do not cause suspicion in the patient. Delayed diagnosis and treatment of acromegaly increases the risk of complications. With timely consultation with a doctor, on the contrary, it is possible to significantly reduce the external manifestations of pathology and side effects.
Surgery
Surgical treatment consists of removing the pituitary adenoma. Currently in clinical practice there are two approaches to neurosurgical treatment of pituitary tumors: transcranial and transsphenoidal. The choice of access is made by a neurosurgeon.
The goal of surgical treatment of this pathology is complete removal of the tumor in the case of microadenoma and maximum removal of part of the tumor in case of macroadenoma. Surgical treatment provides quick results and is highly effective in relieving headaches and eliminating compression of the optic nerve.
At the moment, the transsphenoidal access method is the most effective method for removing microadenomas. This surgical intervention is performed under endoscopic control, this helps to carry out the operation as successfully as possible. For 50% of patients with a large pituitary tumor, surgical treatment is ineffective, because after surgery the level of somatotropin remains the same.