Home | About us | Delivery | Advertisers | Login | Registration
Delivery on Sundays and holidays does not work!
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2022 Pharmacy 84.
Among the drugs that affect gastric secretion, proton pump inhibitors (PPIs) have firmly taken a leading position in the treatment of acid-dependent diseases (ADDs) of the gastrointestinal tract (GIT), almost completely replacing H2-histamine receptor blockers (H2-blockers) and significantly by reducing the frequency of patients taking antacids [1]. Over 30 years of use, PPIs have shown high effectiveness in the treatment of patients suffering from various diseases: gastroesophageal reflux disease, duodenal and gastric ulcers (DU), erosive and ulcerative lesions of the gastric and duodenal mucosa (DU) caused by taking acetylsalicylic acid (ASA) and non-steroidal anti-inflammatory drugs (NSAIDs), chronic gastritis associated with Helicobacter pylori
, as well as functional disorders of the upper gastrointestinal tract, the clinical symptoms of which are caused by hypersecretion of gastrocytes. Russian and international standards, as well as clinical recommendations for the diagnosis and treatment of CDZ, based on the vast accumulated evidence-based medicine, contain clear indications for the use and regimens for the use of PPIs, assigning the most important role to drugs in this group [1, 2].
However, quite often, practitioners recommend the use of antacids and/or H2 blockers. About 30-50% of pregnant women take antacids during pregnancy to treat heartburn. These drugs are divided into absorbable (sodium bicarbonate) and non-absorbable (magnesium hydroxide, calcium carbonate, aluminum phosphate, etc.). Despite the ability of sodium bicarbonate to quickly relieve heartburn, its effect is short-lived and heartburn soon returns. In addition, sodium absorbed in the intestines can lead to edema, which is undesirable for pregnant women. Non-absorbable antacids, which are highly effective and have mild side effects, can be prescribed during pregnancy. To date, most of them are considered safe and approved for use in average therapeutic doses, but you should always remember that antacids can adsorb other medications taken during pregnancy. First of all, we are talking about iron supplements, which are necessary for the treatment and prevention of anemia during gestation.
The absence of teratogenic effects of ranitidine (H2-blocker) in experimental conditions and clinical practice proves their safety during pregnancy. The number of studies on the safety of famotidine and nizatidine to date is too small to draw clear conclusions. The duration of the clinical effect of H2 blockers is much shorter, which requires an increase in the frequency and dose of their use, leading to the development of undesirable reactions - dry mouth, changes in appetite, stool disturbances, etc. However, in everyday clinical practice, to relieve the symptoms of chronic diseases: heartburn , belching, a sour taste in the mouth, pain or a burning sensation in the epigastrium, nausea, etc., obstetricians and pregnant women themselves use PPIs (usually omeprazole).
Acid-induced symptoms during pregnancy are either the result of an exacerbation of pre-existing chronic diseases in patients, or develop against the background of a number of processes characteristic of the gestation period. In particular, it has been shown that, due to hormonal changes, there is a disturbance in the tone of the smooth muscles of the gastrointestinal tract, a decrease in the sensitivity of receptors, and with an increase in the uterus and total body weight, an increase in intra-abdominal and intragastric pressure and a violation of motor-evacuation contractions are observed [3].
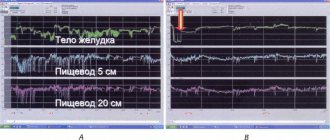
Data from a manometric study of the esophagus and stomach in 12 pregnant women, conducted by E. Bainbridge et al., showed a decrease in the tone and motor activity of the upper gastrointestinal tract, as well as the pressure of the lower esophageal sphincter (LES), while increasing the frequency of antiperistaltic contractions of the esophagus. These phenomena, according to the authors, contribute to the development of gastroesophageal reflux during pregnancy [4].
Functional disorders of the contractility of the gastrointestinal tract during gestation (hypomotility, antiperistalsis), as a rule, disappear after resolution of pregnancy and do not bother the woman in later life [3]. Increased energy consumption in the body of a pregnant woman entails an increase in the amount of food consumed and, as a consequence, an increase in the functional activity of the digestive organs [5]. Such common phenomena during pregnancy as nausea, constipation, hypersalivation, changes in taste preferences associated with changes in the secretory and motor functions of the digestive system (decrease in the speed and amplitude of waves of esophageal peristalsis, which disrupts its clearance and slows down gastric evacuation) do not prevent adequate intake food into the body [6, 7].
According to many epidemiological studies, more than 60% of pregnant women experience acid-induced symptoms more than 2 times a week in various trimesters of pregnancy. The most common symptom of CVD in pregnant women is heartburn [8, 9]. The manifestation of heartburn only during gestation in the absence of a chronic recurrent disease is defined as heartburn of pregnant women. Heartburn is the leading clinical symptom and the main diagnostic criterion for GERD. Long-term exposure to refluxate on the mucous membrane of the esophagus when gastric contents and/or DC are thrown into it weakens the protective mechanisms of the mucous membrane and triggers inflammation processes: oxidative stress, activation and degranulation of mast cells, release of inflammatory mediators and free radicals, potentiating the cytotoxic effect [10]. In addition, a decrease in pH in the esophageal cavity to less than 4.0 leads to intracellular acidosis with subsequent possible destruction and development of necrosis of esophageal epithelial cells with the formation of erosions and/or ulcers of its mucous membrane [11, 12].
According to the results of a study of the clinical manifestations of GERD in 166 pregnant women published in 2015, the prevalence of GERD symptoms in the first trimester of pregnancy was 16.9%, in the second - 25.3% and in the third - 51.2%. At the same time, extraesophageal manifestations of the disease (cough, bronchial asthma) during gestation were much less common than in the general population of patients with GERD [13].
Symptoms of CPZ, reducing appetite, lead to refusal or reduction in the frequency of meals, lengthening the intervals between meals, which provokes an increase in functional disorders of the digestive organs, exacerbation of chronic gastrointestinal diseases, and helps to reduce the body weight of a pregnant woman in the first trimester. The high prevalence of symptoms induced by exposure to hydrochloric acid on the mucous membrane of the upper gastrointestinal tract during gestation requires timely and effective measures to relieve them. This will ensure a complete balanced diet, improve the mother’s digestive processes and embryo trophism, and also improve the quality of life of the expectant mother [8].
The presence of heartburn, sour belching and other symptoms caused by the negative impact of gastric contents on the mucous membrane of the esophagus requires timely diagnosis with determination of the severity of the disease and the risk of recurrence of clinical manifestations after delivery in order to select optimal therapy, which includes modification of lifestyle and a course of drug treatment, the choice of which An important place should be given to patient compliance [12].
The results of studying the safety of PPI use in pregnant women are presented in a meta-analysis by S. Gill et al., performed on the basis of 60 studies (134,940 patients) [14]. It has been shown that there is no relationship between PPI use and the risk of fetal pathology, spontaneous abortion or premature birth. This allowed us to conclude that this group of drugs is safe and recommend them to women who have acid-induced symptoms as a result of functional disorders or exacerbations of CVD during pregnancy. Experts from the US Food and Drug Administration (FDA - Food and Drug Administration) assigned drugs in this group safety category B.
The safety of omeprazole has been primarily studied in animal studies (rats and rabbits). At the same time, a dose-dependent probability of fetal death was established, although teratogenic effects were not identified [15]. In addition, the FDA received information about 12 cases of congenital malformations in children whose mothers took the drug after the 13th week of pregnancy (5 cases of anencephaly and 1 case of hydrocephalus) [16].
On the other hand, the literature describes a large number of observations indicating the safety of omeprazole. M. Harper et al. observed a woman suffering from Zollinger-Ellison syndrome who was prescribed omeprazole during two pregnancies. She first received the drug at a dose of 120 mg per day starting at week 11 and gave birth to a live, full-term baby. During the second pregnancy, she took 180 mg of omeprazole and 450 mg of cimetidine per day and also gave birth to a healthy full-term baby [17].
In a study by G. Brunner et al. 9 women took from 20 to 60 mg of omeprazole during pregnancy, 4 of them in the first trimester. No pregnancy complications, developmental anomalies or congenital deformities were noted in newborns, and the duration of observation of the children was 12 years [18].
There are also several prospective studies confirming the safety of PPIs and, in particular, omeprazole in pregnant women. According to the Swedish Medical Birth Registry, an analysis was conducted of the condition of 262 newborns whose mothers took omeprazole throughout pregnancy [19]. Among them, 8 birth defects were recorded (3.1%). At the same time, the prevalence of congenital anomalies in the general population according to the same Register was 3.9%. Another prospective cohort study compared the pregnancy outcomes of three groups of women: the first included 113 people taking omeprazole; in the second - 113 patients taking H2 blockers; and the third - 113 women who did not take any antisecretory drugs (control group) [20]. There were no significant differences in pregnancy outcomes between the three groups of patients (number of live births, spontaneous miscarriages, premature births, cesarean sections, birth weight) [20]. The incidence of major congenital malformations in newborns whose mothers took omeprazole in the first trimester was 5.1% (4 out of 78); and in the second and third groups - 3.1% (3 out of 98) and 3% (2 out of 66), respectively. The risk of developing congenital deformities was 0.9 for omeprazole, and 1.3 and 1.5 for cimetidine and ranitidine, respectively. There are other observations, the results of which confirm the safety of omeprazole during the gestational period. Thus, according to observations in the UK and Italy, 134 women taking omeprazole gave birth to 139 live newborns (in 11 cases premature births occurred), 5 (3.7%) had congenital deformities, of which 2 were heart defects ( ventricular septal defect) [21].
A cohort study was conducted in Denmark to determine the association between PPI use and the risk of major birth defects. We compared the incidence of fetal pathology in women who took PPIs 4 weeks before conception and during 12 weeks of gestation (first trimester), as well as those who took PPIs only during the first trimester of pregnancy. Developmental defects of all live-born children were detected during the 1st year of their life. It was found that among 840,968 women examined (childbirth resulted in a live birth), 5,100 took PPIs 4 weeks before conception and throughout the entire first trimester of pregnancy (group 1), 3,651 pregnant women took PPIs only during the first trimester (group 2 ). In children of women from group 1, 174 (3.4%) serious congenital malformations were identified, while in the group who did not take PPIs, 21,811 (2.6%) malformations were identified. In group 2, out of 3651 subjects, 118 (3.2%) major birth defects were identified. In a secondary analysis of the effect of individual PPIs on the risk of developing congenital pathologies, no significantly significant differences were identified (insufficient data were obtained for rabeprazole). In conclusion, we can say that taking PPIs 4 weeks before conception and during the first trimester of pregnancy does not significantly increase the risk of developing birth defects [22].
Thus, we can agree with the conclusion of J. Richter that omeprazole is safe when prescribed to pregnant women [4].
Omez (omeprazole) is approved for use during pregnancy and lactation. The drug is listed in the US Food and Drug Administration (FDA) Orange Book as a PPI with proven therapeutic equivalence category A.
According to a report received by the Federal Service for Surveillance in Healthcare on the results of drug safety monitoring, omez is characterized by a high safety profile. No serious adverse events have been reported with the use of the drug. Omez (omeprazole) is approved by 16 regulatory authorities worldwide [23].
The choice of antisecretory therapy increases the doctor's responsibility regarding the development of possible side effects from the drug, which often leads the doctor to choose less effective therapy. However, it cannot be excluded that the presence of acid-induced symptoms and the risk of developing complications of CDZ, especially bleeding from the upper gastrointestinal tract, in the absence of adequate assistance, can lead to a violation of the quality of life, refusal of pregnancy and its premature resolution due to the severe course of CDZ.
The generalized results of world research have made it possible to authorize the use of omeprazole drugs during pregnancy, provided that the instructions for use of the drug indicate that omeprazole in the specified dose and duration of administration does not have side effects on the health of pregnant women and the development of the fetus.
Conflict of interest:
The materials in the article are advisory in nature and do not address conflicts of interest.