Pediatrician
Sayfulina
Maryam Zakareevna
32 years of experience
Pediatrician of the highest category, member of the Union of Pediatricians of Russia
Make an appointment
Hemophilia is a hereditary pathology of homeostasis, manifested in a violation of blood clotting against the background of reduced synthesis of necessary substances by the patient’s body (factors VII, IX, XI). Persons suffering from the disease regularly find hematomas on their bodies or encounter hemarthrosis, internal bleeding due to injuries or surgical interventions. Treatment of hemophilia in children is based on replacement therapy, which must be received throughout life.
Reasons for the development of pathology
The mechanism and type of inheritance of hemophilia have been studied in sufficient detail. Genes that provoke insufficient production of blood clotting factors are linked to the X chromosome. The pathology is inherited recessively through the female line. Hereditary pathology occurs exclusively in boys.
The sons of a healthy man and a woman who is a carrier of the pathological gene are equally likely to be born without signs of hemophilia or with them. A man suffering from bleeding disorders will be able to conceive healthy children with a woman who is not a carrier of the altered gene.
Medicine knows of isolated cases of hemophilia in women. Their mothers were carriers of a mutated gene, and their fathers suffered from insufficient production of blood clotting factors. The cause of hemophilia in such cases is a combination of recessive and dominant genes.
GYNECOLOGICAL COMPLICATIONS IN WOMEN WITH INCREASED BLEEDING
Rice. 2.
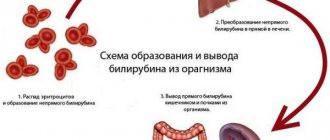
Blood clot formation
Fibrin clot formation
At this stage, a network-like covering of the blood clot is formed - a fibrin clot (blood clot), formed through the interaction of 13 plasma clotting factors, numbered in Roman numerals from I to XIII (Fig. 3).
Deficiency of any of these proteins can result in delayed or incomplete clot formation and subsequent resumption of bleeding when the clot forms temporarily, requiring reinforcement with a fibrin clot. Rice.
3. Fibrin clot formation
Problems with increased bleeding in women
Bleeding problems can be inherited or acquired during a woman's life. Acquired increased bleeding can be caused by certain types of medications, treatments, malignant diseases and autoimmune disorders. Let us dwell on hereditary problems, which most often cause bleeding problems in women.
von Willebrand disease
Von Willebrand disease (VWD) is reported to be the most common cause of excessive bleeding in humans.
Rice.
4. Inheritance of von Willebrand disease
The presence of von Willebrand disease (VWD) is caused by a gene passed from parent to child. The abnormal von Willebrand disease gene is located on one of the regular chromosomes, not on the sex chromosome (like hemophilia), and therefore VWD occurs with equal intensity in both men and women. Often, an accurate family history can help a doctor diagnose the condition. Sometimes an abnormal gene may manifest itself for the first time in a patient when neither of the parents possessed it. This is called a new "mutation", and the disease can then be passed on to successive children in the usual way. A specific test for the von Willebrand factor gene (DNA test) is now available for some forms of von Willebrand disease. It is sometimes possible to trace von Willebrand disease over several generations. The figure above shows the usual pattern of dominant inheritance. Although the genetic defect is inherited in an autosomal manner, it does not follow the classical pattern of autosomal dominant or autosomal recessive inheritance. Moderate VWD and some forms of the disease (type 2A or 2B) appear as a consequence of the autosomal dominant model; severe VWD, with von Willebrand factor, occurs only when two genes are defective.
The exact prevalence is unknown, but some estimates suggest it is present in 1% of the world's population. BV occurs throughout the world among people of all socioeconomic and ethnic groups. This is an autosomal disease (that is, it affects both men and women equally) (Fig. 4). There are three main types of VWD depending on whether the VWF defect is quantitative or qualitative. In VWD type 1, there is a deficiency of von Willebrand factor (vW). Type 2 VWD, which has four subtypes, occurs when there is a qualitative defect in vWF (the factor does not function properly). In type 3, vWF is almost or completely absent. Most types are inherited in an autosomal dominant manner. Type 3 and 2N are inherited in a recessive manner. It is important to know which type of BV each individual patient has because treatment for different types of disease is different. If there is a significant decrease in vWF, as in type 3, or a problem with vWF associated with factor VIII, as in type 2N, then a significant decrease in factor VIII relative to normal may also occur. Sometimes people with type 3 or 2N BV are misdiagnosed as having hemophilia due to significantly reduced factor VIII. To prevent such misdiagnosis, it is necessary to check the level of factors VIII and von Willebrand when determining a blood coagulation disorder in a patient.
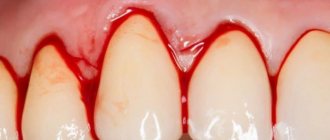
Signs of BV are expressed in the body's inability to form a blood clot. Bleeding mainly occurs from the mucous membrane and (or) skin. The most common signs are the presence of a large number of bruises on the body, frequent or prolonged nosebleeds, heavy or prolonged menstrual bleeding (menorrhagia) and prolonged bleeding from wounds, surgery, tooth extraction and in women in labor during childbirth. Gastrointestinal bleeding may also occur. Joint bleeding in BV is less common than in hemophilia and usually occurs in patients with low levels of factor VIII in the blood.
Hemophilia
Since the inheritance principle of hemophilia A (factor VIII deficiency) and hemophilia B (factor IX deficiency) is a sex-linked recessive trait, women extremely rarely suffer from these diseases. It is more possible, but unproven, that bleeding occurs in female carriers of hemophilia A or B. A symptomatic carrier with low levels of factor VIII or IX may experience increased bleeding in the same way as a patient with mild hemophilia during surgery or trauma. In women, however, abnormal periods may be the only symptom. Irregular, heavy or prolonged menstrual periods are the most common symptoms among carriers of the hemophilia A and B genes. Excessive bleeding associated with pregnancy and childbirth can also occur in cases where factor levels are below 30%. Female carriers whose factor level allows them to be classified as having a mild form of hemophilia require the same treatment for bleeding as men with a mild form of hemophilia. Clinically there is no difference.
Mixed diseases
Deficiency of any of the blood clotting proteins (factors) may indicate signs of varying degrees of severity as well as quantitative and qualitative platelet defects. Most symptoms of such defects will resemble those of von Willebrand disease. Some diseases associated with deficiency of blood clotting factors are quite mild (for example, factor XII deficiency). Others, such as hypofibrinogenemia (deficiency of the clotting factor fibrinogen) are particularly problematic. Many of these diseases are inherited autosomalally by women and men equally.
Gynecological symptoms observed in women with increased bleeding
Menorrhagia/metrorrhagia
Prolonged and heavy menstrual bleeding is the most common hemorrhagic symptom observed in women with bleeding problems. Some suffer from excessive bleeding during the menstrual cycle (menorrhagia); others experience similar problems immediately after the end of the menstrual cycle (metrorrhagia). The uterus is a highly vascular organ capable of losing large amounts of blood over a short period of time. Prolonged bleeding can cause iron deficiency anemia. Therapeutic interventions such as dilatation and curettage of the walls of the uterine cavity usually only worsen the situation, since the alignment of the lining tissues of the uterus prevents the formation of a fibrin clot, the uterine cavity remains unprotected and the resumption of hemostasis is complicated.
Dysmenorrhea and mid-cycle pain
Another common complaint among women with excessive bleeding is pain during menstrual periods and mid-cycle pain. One can only speculate about their reasons, since no reliable scientific data on this issue exists. Some women may experience pain as a result of heavy bleeding and incomplete formation of clots in the uterus. In other cases, there is pain in the pelvis or abdomen, which occurs with endometriosis. Endometriosis is an abnormal condition in which the growth of endometrial tissue occurs in the abdominal cavity outside the uterus. When any woman is on her menstrual period, the intrauterine tissue - wherever it is - will bleed. If a woman has a bleeding disorder and endometriosis, tissue outside the uterus may bleed, causing peritoneal irritation (irritation of the peritoneum) and pain.
I have spoken with women who experience excessive bleeding during ovulation and experience severe pelvic pain. When the egg is released from the ovary, healthy women experience very little bleeding. But in women with bleeding disorders, this can be a significant problem. I once met a woman with von Willebrand disease type 3 whose bleeding during ovulation was so intense that she had to take birth control pills for the rest of her life to avoid ovulation.
Conception/fertility problems
Many women with bleeding problems use birth control pills or other hormone therapy. Obviously, this affects a woman's ability to conceive. The long-term effect of such long-term hormonal therapy is not known. It is also unknown whether von Willebrand factor deficiency has any effect on the ability of a fertilized egg to attach to the uterine wall, which in turn may affect the ability to carry a fetus to term. It seems casuistic that there is a higher likelihood of miscarriage in women with BV than in the general case. This may be simply because when a miscarriage occurs, the subsequent excessive bleeding forces the woman to seek medical attention and her diagnosis is noted. At the same time, a miscarriage that occurs in the early stages of pregnancy in an ordinary woman may not even be perceived as such. The bleeding that follows spontaneous termination of pregnancy can be quite significant, since the high level of clotting factors naturally maintained in the blood during pregnancy decreases sharply after the loss of the fetus. Postpartum bleeding can be a problem for women with bleeding disorders. Depending on the disease, problems may be small or very minor because hormones that rise during pregnancy cause clotting factors to increase. This is especially true for factors VIII and von Willebrand. However, even if there are no complications immediately after birth, postpartum hemorrhage may occur a few days later, when hormone levels and levels of clotting factors begin to decline. Patients with von Willebrand disease have a greater number of primary (immediate) and secondary (delayed) postpartum hemorrhages. In women who breastfeed, hormone levels remain high, but it is not known whether this protects against postpartum hemorrhage. Pregnancy does not provide any protection to women with VWD type 2, since hormonal increases and increases in von Willebrand factor do not alter the functional impairment of vWF. Factor IX levels do not increase during pregnancy.
Diagnosis of hereditary diseases that cause increased bleeding
For non-hematology physicians, including obstetricians-gynecologists and family physicians, diagnosing a bleeding disorder can be challenging at best. First responders typically rely on prothrombin time (PT) and activated partial thromboplastin time (aPTT) tests and, to a lesser extent, clotting-bleeding time to make a diagnosis. The difficulty with this is that the most common bleeding disorder in women, von Willebrand disease, cannot be detected using these tests.
In von Willebrand disease, there are no changes in PT, and the aPTT is only occasionally prolonged. Increased PT occurs only with a deficiency of factors X, VII, V, II, I, or with certain liver diseases. The aPTT is prolonged only when the patient has a deficiency of factors XII, XI, X, IX, VIII, V, II or I. The aPTT in von Willebrand disease is prolonged only if the level of factor VIII is below 40%. For patients with qualitative type 2 VWD (except 2N), the aPTT will usually be normal. Bleeding time can be normal or prolonged. Bleeding time testing is not very accurate. This is a superficial test to assess platelet function and can be affected by various external factors, such as a cold. VWF testing should include a ristocytin cofactor test, which assesses the function of VWF, the antigen to VWF, which measures vWF levels and factor VIII levels. Many doctors also use the test to evaluate the binding capacity of vWF collagen. Additional tests, such as the vWF multimer assay, are used to study protein structure, which is especially useful in studying the different subtypes of von Willebrand disease type 2. There is no perfect test for diagnosing VWD.
Laboratory tests to determine the presence of BV are often negative or inconclusive and may require repeat testing for confirmation. People with BV may have cyclical variations in their levels, making diagnosis difficult, especially in its milder forms. The timing of the test is important. It is better to test a woman during her menstrual cycle, when hormonal and factor norms are at their lowest. When performing a coagulation test, it is important for the examiner to consider any environmental factors or medications that may affect the accuracy of the test. Hormonal therapy such as oral contraceptives, due to their stimulating effect on vWF and factor VIII, should be interrupted before testing. The use of certain drugs that have contraindications that affect platelet function should also be discontinued. This is aspirin and most non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, diclofenac, Voltaren, Celebrex, etc. Because of a number of reasons that can affect the accuracy of the result and normal fluctuations in factor levels, it is necessary to repeat tests in women with a history of bleeding, even if the test results are normal at the time. It is also necessary to refer the woman to hematologists with experience in treating bleeding disorders.
These hematologists are typically affiliated with treatment centers throughout the United States and around the world. Special tests necessary to establish a diagnosis usually require the use of specialized equipment, reagents and technology. Laboratory errors in the assessment of coagulation problems are common among non-specialized laboratories. Very few of the women I interviewed were diagnosed without repeated testing. This is a huge waste of time and money.
Treatment of gynecological complications in women with increased bleeding
The various treatments described below have been successful in the women I interviewed. This list is not final. You should consult your doctor to determine the appropriate method for your particular case.
Hormone therapy
Oral contraceptives (OCs) are very effective in increasing levels of factors II, VIII, and von Willebrand factor. For this reason, they are especially useful in treating heavy menstrual periods as well as other bleeding in women. Women often report that during their menstrual period and taking placebo pills (pacifiers), they also have an increase in the number of strokes and nosebleeds, which decrease once they take the contraceptives again. For symptomatic carriers (factor VIII), OC may be the only possible treatment option. For women with qualitative VWF defects, the effectiveness of oral contraceptives is reduced because the hormones increase VWF levels but do not correct the inherent structural defects. For these women, OCs probably have some success in helping regulate their menstrual periods and reduce bleeding, but other treatments may also be necessary. For bleeding not sensitive to OCs, the use of pure progestin components, such as Norulat and Provera, can be very useful because they cause thickening of the lining uterine tissue (secretory myometrium) and stop bleeding. Question: How long can you stop menstruating? Some doctors prefer the use of progesterone components such as Depo-Provera for intramuscular administration, although the results, according to surveys of women, vary. Progesterone components when deposited intramuscularly are unsafe for a number of reasons:
1. They require an intramuscular injection, which is not recommended for people with bleeding problems. 2. If side effects occur in some patients during administration, they may last for several months, whereas the half-life for oral contraceptives is much shorter. 3. Dosage can be better managed with the assistance of a specialist. Strictly speaking, in case of life-threatening bleeding, the use of intravenous combined estrogens (Premarin) is very effective.
Desmopressin acetate
This medication is usually administered by injection (intravenously or subcutaneously - DDAVP) and intranasally (nasal drops - Stimate). It is chemically related to antidiuretic hormone (vasopressin). When used, DDAVP causes a dramatic increase in circulating plasma factor VIII and von Willebrand factor, stimulating the production of these proteins from blood vessel walls. This drug is very effective in treating bleeding in women with type 1 BV and symptomatic carriers of hemophilia A with factor VIII deficiency. It is less effective for women with type 2 VWD because it does not correct the molecular defects in von Willebrand factor. The drug is ineffective in VWD type 3, where little or no VWF is produced, and should not be used in type 2B due to excessive platelet binding and subsequent thrombocytopenia. (Thrombocytopenia is a condition characterized by a decrease in the number of platelets and, accordingly, an increase in bleeding). Unfortunately, DDAVP does not provide any benefit to female symptomatic carriers of hemophilia B because it has no effect on factor IX. When a "strong" spray (Stimate) is prescribed, doctors do so because there is a less concentrated formulation of intranasal desmopressin called DDAVP used to treat nocturnal enuresis. This less concentrated form of the drug is correspondingly ineffective for patients with increased bleeding.
Plasma preparations
Women with increased bleeding who are not sensitive to desmopressin or active hormonal therapy are indicated for replacement therapy for clotting factor deficiency or defectiveness. Today, with the advent of more reliable, virus-inactivated lyophilized plasma preparations (factor concentrates) in many countries, the use of preparations such as cryoprecipitate or fresh frozen plasma is unacceptable. The US National Hemophilia Organization and Scientific Advisory Board recommend against their use if virus-inactivated drugs are available. In the United States and other countries where safe and hemostatically effective drugs are available for the treatment of bleeding associated with disorders of factors II, VII, VIII, IX, X, and von Willebrand factor. In the United States, the two most widely used drugs for treating von Willebrand disease are Humate-P (Haemate-P in other countries) and Alphanate SD. Both of these drugs are concentrates with high levels of factor VIII and von Willebrand factor. Monoclonal or recombinant factor VIII preparations should not be used for VWD because they do not contain von Willebrand factor.
Antifibrinolytics
Drugs such as aminocaproic acid may be useful in treating menstrual bleeding, as well as bleeding from the mucous membranes of the nose and mouth. These medications do not form a clot, they simply keep the clot in place longer by blocking the enzymes responsible for fibrinolysis (the spontaneous, normal process of breaking up a clot once it has formed). These drugs should not be used for joint and kidney bleeding.
NSAIDs and analgesics
Most NSAIDs tend to interfere with platelet function. They interfere with platelet adhesion and aggregation (platelets become unable to join to form a clot). Data exist to show that two anti-inflammatory drugs, choline-magnesium-trisalicylate (Tri-lisate) and salsalate (Disalcid), do not alter platelet function and may therefore be useful for use in individuals with bleeding disorders. These medications are often useful for managing pain associated with ovulation and menstruation. A new class of NSAIDs, Cox-2 inhibitors (Celebrex), do not cause platelet dysfunction and may be useful for people with bleeding problems.
Surgical issues
Intrauterine ablation
In women who do not respond to other treatments, the uterine lining may need to be removed to prevent menstruation, although this will render it sterile. This may serve as a safe alternative to hysterectomy for bleeding problems. There is scientific evidence in the literature supporting the safety and effectiveness of this procedure for women with a range of bleeding problems.
Hysterotomy
For some women who are minimally responsive or completely resistant to other therapies, hysterotomy may be the only acceptable treatment. Vaginal or transabdominal hysterectomies have been safely performed in women with bleeding problems after adequate and appropriate plasma factor concentrations have been achieved.
Laparoscopy
In women experiencing pain due to endometriosis (bleeding from endometrial tissue growing outside the uterine cavity), removal of migrating tissue using a laparoscopic technique can be effective. In this procedure, two small incisions are made in the abdomen. A special probe for visual manipulation is guided by the surgeon through one of the incisions, while the tissue is removed through the second incision.
Dilatation and curettage of the uterine cavity
These procedures entail relaxing and sufficiently dilating the cervix and scraping the endometrium. The use of these procedures with the intention of reducing the intensity of bleeding cannot be effective for women with bleeding, since this technique prevents thrombus formation on damaged vessels of the subendometrial location. Also, if dilatation and curettage of the uterine cavity are not performed for diagnostic purposes, this is unacceptable in cases with patients with increased bleeding.
Ovariectomy
Ovariectomy (removal of the ovaries) may be an acceptable option for women who experience bleeding during ovulation and who, for one reason or another, cannot benefit from hormone therapy. However, this procedure not only makes the woman sterile, but also stimulates menopause. It is imperative that women considering any of these options fully understand the risks, benefits, and alternatives before making a definite decision.
Conclusion
I hope that this article will be useful for women and practitioners looking for answers to some of the questions that arise in patients with problems with increased bleeding. I also hope the article will raise many questions that the medical and scientific communities will try to find answers to. The time has come to join forces to solve these problems.
additional literature
1. "Females Bleed Too." HANDI Quarterly (Fall 1993).
2. "Symptomatic Carriers." HANDI Quarterly (Fall 1994).
3. Medical and Scientific Advisory Council "Recommendations Regarding Women With Bleeding Disorders." Medical Advisory #303 (1997), National Hemophilia Foundation.
4. Medical and Scientific Advisory Council “Treatment of von Willebrand Disease.” Medical Advisory #314 (1998), National Hemophilia Foundation
5. Bottini, E., et al. “Prevention of Hemoperitoneum during Ovulation by Oral Contraceptives in Women with Type III von Willebrand Disease and Afibrinogenemia. Case Reports." Haemoatologica 76 (1991): 431-33.
6. Brenner, P.F., Ed., “Management of Bleeding Disorders in Women, The Role of the Obstetrician/Gynecologist.” American Journal of Obstetrics and Gynecology. (1996): Suppl. 175(3) Part 2. 761-792.
7. Bunschoten, EP, et al. "Bleeding Symptoms in Carriers of Hemophilia A and B." Thrombosis and Hemostasis (Germany) 59, no. 3 (1988): 349-352.
8. Caldwell, David, et. al. "Hereditary Coagulopothies in Pregnancy." Clinical Obstetrics and Gynecology 28, no. 1 (March 1985).
9. Conti, M., et al. "Pregnancy in Women with Different Types of von Willebrand Disease." Obstetrics and Gynecology 68 (1986): 282.
10. Cohen, S., et al. "Epidural Analgesia for Labor and Delivery in a Patient with von Willebrand Disease." Regional Anesthesia 14 (1989): 95-97.
11. Ewenstein, B. “von Willebrand's Disease.” Annual Reviews in Medicine 48 (1997): 525-42
12. Kouides, P “Females with von Willebrand disease: 72 years as the silent majority.” Haemophilia 4 (1998): 665-676
13. Lee, CA "Women and von Willebrand disease." Haemophilia 5 (1999): Suppl. 2. 38-45
14. Murray E. and Lilicrap, D. “von Willebrand Disease: Pathogenesis, Classification, and Management.” Transfusion Medicine Reviews Vol. X, no 2 (1996): 93-110
15. Paper, R., Baker J and Larson K. “Women Can Have Bleeding Disorders.” Slide presentation. National Hemophilia Foundation. 1999
16. Robertson, L. E., et al. "Hereditary Factor VII Deficiency in Pregnancy: Peripartum Treatment with Factor VII Concentrate." American Journal of Hematology 40 (1992): 38-41.
17. Scott, J. P., and R. Montgomery. "Therapy of von Willebrand Disease." Seminars in Thrombosis and Hemostasis 19, no. 1 (1993).
18. Vosburgh, E. “Rational Intervention in von Willebrand Disease.” Hospital Practice (March 1993).
Classification of the disease
Types of hemophilia are distinguished based on the deficiency of a certain blood clotting factor in the patient's body. Basic information about the types of disease is presented in the table.
| View | Description |
| A | It is diagnosed in 84-86% of people suffering from the pathology in question. Caused by a deficiency of clotting factor VIII (antihemophilic globulin). |
| B | Occupies a share of 12-13% of clinically diagnosed cases of hemophilia. Develops against the background of deficiency of coagulation factor IX (thromboplastin) |
| C | Occurs no more often than 1-2%. Becomes a consequence of insufficient production of blood coagulation factor XI. |
About 0.5% of detected cases of hemophilia of various etiologies belong to other types - V, VII, X and others.
Gastrointestinal bleeding
In the case of severe hemoglobin and severe deficiency of coagulation factors (more often with a combined deficiency of factors VIII and IX), traces of blood can be noticed already during the first regurgitation after feeding the baby. Excessively hard food and children swallowing small objects (especially those with sharp edges or protrusions) can injure the mucous membrane of the gastrointestinal tract.
As a rule, if fresh blood is detected in the vomit or during regurgitation, then damage should be looked for on the mucous membrane of the esophagus. If the vomit looks like “coffee grounds,” then the source of the bleeding is in the stomach; the blood has had time to react with hydrochloric acid, and hydrochloric acid hematin has formed, which has a characteristic appearance.
If the source of the bleeding is in the stomach, there may also be the presence of black, often liquid, tarry stools called melena. If there is fresh blood in the child's stool, bleeding from the lowest parts of the intestine - the rectum and sigmoid colon - can be suspected.
Symptoms of hemophilia
The first signs of pathology can be detected in newborns. Thus, the likelihood of confirming the diagnosis of hemophilia in a child will be indicated by prolonged bleeding from the umbilical cord and numerous subcutaneous hematomas. Excessive bleeding in infants at the time of teething becomes no less alarming. But during lactation, the child receives a sufficient amount of thrombokinase with mother's milk.
Post-traumatic bleeding is typical for children who have learned to crawl and walk. In addition to nosebleeds, intermuscular hematomas and hemorrhages in the joints (hemarthrosis) are added. Against this background, anemia develops.
As children age, they may experience bleeding from the gastrointestinal tract. This is caused by injury or medical procedures. The greatest danger is bleeding from the nasopharynx and pharynx. Against this background, airway obstruction may develop.
Are you experiencing symptoms of hemophilia?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Hemarthrosis
Hemarthrosis is hemorrhage in the joints, which is more often observed in children with hemophilia from 1 to 8 years old. Large joints are predominantly affected, especially the knees and elbows, less commonly the hip and shoulder.
- Acute hemarthrosis is a newly emerging condition with a turbulent clinical picture.
- Recurrent hemarthrosis is frequent, repeated hemorrhages in the same joint.
The frequency and location of hemorrhages in the joints depends on the severity of hemophilia and the type of physical activity:
- When running and jumping quickly, symmetrical hematomas can form in the knee joints.
- If you fall on any side, hemarthrosis occurs on the corresponding side.
- When loading the upper limbs (pull-ups, hanging, push-ups and other types of activity associated with the work of the arms and shoulders), hemorrhages in the elbow and shoulder joints and small joints of the hands are common. The affected joint increases in volume, there is swelling, pain when palpating and moving.
Hemarthrosis without treatment, especially recurrent ones, can be complicated by suppuration of the contents of the joint capsule, as well as organization (degeneration into scar tissue) and the formation of ankylosis (stiff, immobile joint).
Diagnosis of pathology
Diagnostic procedures are performed by doctors of several specializations: neonatologist, pediatrician, geneticist and hematologist. For concomitant pathologies, consultation with a gastroenterologist, orthopedist, otolaryngologist and neurologist may be required.
At-risk couples should visit a doctor before conceiving a child. Molecular genetic research of biomaterials from future parents will allow us to take into account the risk of having a child with hemophilia. After conception, prenatal screenings may be performed. Their results will confirm or refute the fact that the child inherited hemophilia.
Neonatal tests performed in the first days of a baby’s life are no less effective. A coagulogram provides the neonatologist with comprehensive information about the production of coagulation factors by the newborn’s body.
In case of hemarthrosis, the child is prescribed an X-ray examination of the joints. Ultrasound diagnostics is performed when signs of internal bleeding and retroperitoneal hematomas are detected.
Treatment of the disease
Therapeutic measures during the treatment of hemophilia belong to one of two groups - preventive or symptomatic. In the first case, a patient with a severe form of pathology receives regular doses of blood clotting factor concentrates. Their presence reduces the risk of developing arthropathy and internal bleeding. When planning surgical interventions (including tooth extraction), the patient receives repeated drug transfusions.
Symptomatic procedures are performed for cuts and external bleeding. Doctors recommend using a hemostatic sponge and applying a pressure bandage. Small wounds should be treated with thrombin.
4.What can be done at home for hemophilia?
To prevent bleeding and improve your well-being, patients with hemophilia can recommend the following:
- Ask your doctor about how to manage bleeding if you have hemophilia;
- Maintain a healthy weight. Additional stress on joints due to excess weight can cause bleeding in hemophilia;
- Choose forms of physical activity with caution. It is better to give preference to swimming and other sports that do not put unnecessary stress on the joints;
- Consult your doctor before taking any medications. And do not take aspirin, ibuprofen or other non-steroidal anti-inflammatory drugs because they affect blood clotting.
- Organize your living space to avoid injuries and accidents as much as possible.
Forecast
Replacement therapy allows the patient's body to produce a sufficient amount of antibodies that block procoagulant activity. Additional measures to support boys or men include plasmapheresis and the use of immunosuppressants. Against the background of regular blood and plasma transfusions, patients may encounter HIV, hepatitis, herpes or cytomegalovirus.
Mild hemophilia does not have a significant impact on the quality and life expectancy of patients. In severe forms of the pathology, the survival prognosis is significantly worse. Clinical guidelines for hemophilia include regular consultation of patients with a hematologist and monitoring of blood clotting parameters through laboratory tests.
Types of hemophilia according to the nature of its course
According to the nature of the course, they are distinguished: mild, moderate and severe.
In mild cases, bleeding occurs only after operations or serious injuries; the disease first appears at school age.The average stage progresses as follows: injuries and hematomas lead to bleeding; the disease is first detected at an early age.
A severe degree is detected in the first months of a child’s life, when teeth begin to cut, during motor activity.
Bleeding in a patient is divided into ordinary and deadly. The second category, for example, includes bleeding of internal organs.
Questions and answers
Is it possible to be completely cured of hemophilia?
Drug therapy and blood or plasma transfusion procedures relieve acute pathology syndromes. Sometimes patients are prescribed long-term use of medications selected based on medical history. But completely eliminating the symptoms of hemophilia remains impossible.
Does hemophilia pose a threat to a child's life?
If parents seek medical advice in a timely manner, the baby will be out of danger. A quick correct diagnosis and initiation of treatment will allow the child not to limit himself in physical activity and games.
Can a boy with hemophilia pass it on to his sons?
The risk of having children with hemophilia from a father with bleeding problems is minimal. The disease will be inherited by sons only if their mother is one of the carriers of the altered gene.