According to WHO, about 90% of those infected are unaware that they are carriers of the hepatitis B virus [1]. At the same time, they remain infectious to others, and their disease becomes chronic. In 15–40% of cases, the pathology causes life-threatening liver diseases, from which about 1 million people die annually [2].
Let's figure out how you can become infected with hepatitis B, for which symptoms it is important to see a doctor immediately, and how to protect yourself from the disease.
Hepatitis B: carriage or disease leading to cirrhosis and cancer?
Hepatology, the study and development of new treatments for liver disease, has made incredible progress over the past two decades. Methods for accurate virological assessment of the activity of hepatitis C and B viruses in the human body, which are the most common causes of chronic hepatitis, cirrhosis, and liver cancer, have been developed and implemented. So-called “non-invasive” methods have been developed and are widely used, that is, without the use of liver biopsy, diagnosing the degree of liver damage, or establishing the stage of cirrhosis. Even more impressive progress has been made in the treatment of these diseases. We have discussed the problem of hepatitis C many times. One has only to add that a new era is opening in the treatment of hepatitis C - drugs with a direct antiviral effect have been developed and are already beginning to be used, thanks to which it is believed that within a decade it will be possible to achieve one hundred percent effectiveness of treatment. In this article we will talk about hepatitis B and new advances in its treatment.
Symptoms of hepatitis B disease
The main signs of pathology include the following:
- nausea and appetite disturbances;
- increased weakness and fatigue;
- yellow tint of the skin;
- painful sensations in the area of the right hypochondrium;
- dark shade of urine.
There is also a fulminant form of development of the disease, in which swelling of the brain develops within a few hours, and the patient falls into a coma. Treatment in this case turns out to be ineffective, and the patient’s death occurs within a short period. Most often, hepatitis occurs in the acute stage, when pronounced symptoms of intoxication appear, followed by icteric syndrome. At the final stage, the patient recovers.
The hepatitis B virus is 100 times more contagious than HIV (human immunodeficiency virus).
Despite the widespread introduction of vaccination against hepatitis B, the prevalence of the disease remains high. In different regions of Russia, the prevalence of carriage of the virus ranges from 1.5% to 11.5%. As with hepatitis C, the source of infection is the blood of an infected person. The routes of infection are similar: the use of non-sterile needles, instruments for various medical and non-medical (piercing, tattoos, manicure/pedicure) manipulations, the use of personal hygiene items of an infected person in everyday life (razor, scissors, toothbrush, etc.), unprotected sexual contact, transmission of the virus from an infected mother to her child. The hepatitis B virus is more stable in the external environment and more contagious than the hepatitis C viruses and human immunodeficiency viruses. Therefore, the natural routes of transmission of the B virus (sexual transmission and mother-to-child transmission) are more significant for this virus.
Prognosis and prevention
Acute viral hepatitis B in adults ends in recovery in 90-95% of cases. But the prognosis of acute hepatitis B worsens significantly if a person has concomitant diseases of the liver and biliary tract, mixed infection (a combination of hepatitis B and D, C viruses), concomitant HIV infection.
With the chronic form of hepatitis B, without the necessary treatment, patients have an increased risk of death due to liver diseases and their complications.
Prevention of hepatitis B infection is based on careful compliance with sanitary and epidemiological measures, which include:
- use of disposable medical instruments;
- strict adherence to the rules of sterilization of reusable instruments;
- thorough screening of blood donors;
- thorough disinfection of dental instruments, devices for trimming manicures, pedicures, and tattoos.
Everyone can reduce the risk of contracting hepatitis B - to do this, you need to pay attention to the quality of sterilization of instruments when visiting a dentist, cosmetologist, tattoo artist, and use individual personal hygiene items. It is also important to give up drug use, casual sex, and undergo regular medical examinations and tests for hepatitis B.
The most effective measure to prevent hepatitis B worldwide is vaccination. It is indicated for every person who cares about their health. After vaccination, immunity is formed, which lasts an average of 15 years. Then it begins to weaken and to maintain it, revaccination is carried out - repeated administration of the vaccine.
Important! According to WHO, in 2022, the proportion of children with chronic hepatitis B in the world under the age of 5 years did not exceed 1%. This figure in 1980–2000 was 5 times higher. This improvement in incidence is due to the use of accessible, safe and effective hepatitis B vaccines.
Vaccination against hepatitis B in Russia
Vaccination against hepatitis B is included in the National Calendar of Preventive Vaccinations.
Both children and adults can get vaccinated. Photo: AndreyPopov / Depositphotos, pediatr-russia.ru The national vaccination calendar of the Russian Federation, approved by Order No. 125n of the Ministry of Health of the Russian Federation dated March 21, 2014, includes three episodes of vaccination against hepatitis B: for newborns (in the first 24 hours of life), in 1 and at 6 months.7 Children from risk groups are vaccinated 4 times: in the maternity hospital, at 1, 2 and 12 months. In addition, vaccination is recommended for all unvaccinated and incompletely vaccinated adults, as well as for those who do not know their vaccination status. In the Russian Federation, mass vaccination against hepatitis started only in 1996, so vaccination is relevant for those who graduated from school earlier.
Conclusion
Viral hepatitis B is a dangerous disease that annually claims about 900 thousand lives. But despite the high risks of complications, timely diagnosis and necessary treatment make it possible to control the course of the disease, reduce the viral load and preserve liver function for many years. To prevent infection with this infection, a person must follow individual hepatitis B prevention measures, undergo regular medical examinations, follow a vaccination schedule for their children, and be vaccinated as adults.
How to protect yourself from hepatitis B?
The only means of protection is vaccination against hepatitis B, which is currently administered to all newborn children and adolescents. Adults with risk factors for infection should also be vaccinated. The hepatitis B vaccine is one of the safest vaccines in the world. Three-time administration of the vaccine according to a special scheme leads to the formation of specific antibodies that prevent the development of hepatitis B disease in 98% of those vaccinated. Immunity lasts for at least 8-10 years, but often remains for life.
Does hepatitis B infection always lead to illness?
Maintaining personal hygiene rules - preventing hepatitis
Almost always, infection leads to the development of the disease. The exception is cases when a vaccination has been given. Also, people who have already had this disease will not get sick.
If the baby was born from a mother suffering from this disease, he is given immunoglobulin in the maternity hospital, specially designed for such cases. This will protect the child by 85 - 95%. Such a high percentage of protection will be provided only if the child subsequently receives the vaccination itself on time.
This immunoglobulin is administered to adults. For example, employees of medical institutions, when it becomes known that a doctor is infected with hepatitis B. It should be noted that vaccination, which was done in advance, gives a guaranteed result.
After infection, people develop an acute form of the disease. If the patient was severely weakened, or the child was infected, then the acute stage most likely will not develop. And the disease will develop into a sluggish chronic form.
Re-infection with hepatitis B
If recovery from an illness is confirmed by laboratory testing, re-infection is almost completely excluded.
Hidden disease
As with hepatitis C, the acute phase of the infection often occurs without jaundice. In the vast majority of cases, patients with acute hepatitis B recover and acquire lifelong immunity to re-infection (protective antibodies to viral proteins are detected in their blood serum). After infection, some people become carriers of the HBsAg virus protein, also called the “Australian antigen.” Carriage most often occurs when infected in childhood. In a small proportion of patients, acute hepatitis drags on and becomes chronic. Chronic hepatitis B, like chronic hepatitis C, often occurs latently and unnoticed for a long time. For many years, a person can feel absolutely healthy, and the first symptoms of the disease appear only at the late stage of liver cirrhosis, when the disease is more difficult to treat and the overall prognosis is unfavorable.
Mechanisms of transmission
In highly endemic areas, hepatitis B is most often transmitted either from mother to child during childbirth (perinatal transmission) or through horizontal transmission (contact with infected blood), especially between infected and uninfected children in the first five years of life. Infants who are infected from their mother, or children who become infected under 5 years of age, very often develop chronic infection.
Hepatitis B is also transmitted through needle sticks, tattoos, body piercings, and contact with infected blood and body fluids, including saliva, menstrual and vaginal fluids, and semen. Infection can also occur through the reuse of contaminated needles and syringes or sharps in medical institutions or in domestic settings, as well as among people who inject drugs. Infection can be transmitted through medical, surgical and dental procedures, tattooing, and the use of razor blades and similar devices contaminated with infected blood. In addition, the hepatitis B virus can be transmitted through sexual contact, especially among unvaccinated individuals who have multiple sexual partners.
Chronic hepatitis B develops in less than 5% of people infected as adults, and in about 95% of those infected during infancy and early childhood. The hepatitis B virus can survive outside the human body for at least seven days. During this period of time, the virus retains the ability to cause infection if it enters the body of an unvaccinated person. The duration of the incubation period for hepatitis B ranges from 30 to 180 days and averages 75 days. The virus is detected in the blood within 30–60 days after infection and can persist in the body, causing chronic hepatitis B, especially if infected during infancy or childhood.
What is important to know about the forms of hepatitis B virus infection?
Chronic infection can occur in two main forms:
The first form is inactive carriage of HBsAg. It is characterized by the absence of viral particles in the blood serum or their detection in a low titer, the absence of inflammation in the liver and, as a rule, a non-progressive course. With a decrease in immunity, inactive carriage of HBsAg can turn into the active form of hepatitis B.
The second form is chronic active hepatitis B. It is characterized by the presence of a large number of viral particles in the blood, the presence of inflammation in the liver, which is reflected in changes in the so-called liver tests (or enzymes), and a progressive course with the risk of developing cirrhosis and liver cancer. In recent years, it has been found that the higher the concentration of virus in the blood, or “viral load,” the higher the risk of developing cirrhosis and liver cancer.
It is impossible to distinguish between these two forms based on the patient’s well-being and only clinical signs of the disease (which, as with inactive carriage, may be completely absent in a patient with chronic hepatitis B).
Hepatitis
Infectious diseases occupy a significant place among all human diseases and among the causes of mortality throughout the world. In the 20th century, humanity eliminated only one infection—smallpox—and discovered 36 new infectious diseases. The cause of these diseases is the entry into the body of living microorganisms: bacteria, viruses or protozoa. Today, in terms of its socio-economic significance, that is, in terms of damage caused to people’s health, material costs of providing medical care, and labor losses, viral hepatitis . This group includes diseases that are different in their origin, modes of transmission, course and outcomes, but they were artificially combined due to the fact that they are all accompanied by inflammation of the liver. Even relatively recently, until the sixties of the last century. When the viral nature of these infections was discovered, they were called Botkin's disease, named after the famous doctor who described this disease. When a person of the older generation says that he suffered Botkin's disease, this means that he suffered as a result of infection with one of the hepatitis viruses, the causative agents of which were unknown at that time; they were discovered later.
Today, in the group of infectious hepatitis, there are at least six independent diseases that differ in the properties of their pathogens, causes of occurrence, clinical manifestations and outcomes. Currently, they are called by pathogens designated as hepatitis viruses, using the Latin letters A, B, C, D, E, G.
There are other hepatitises, the causative agents of which are poorly studied or have not yet been identified. Each virus has only its own properties. Having contracted one of the viral hepatitis does not exclude the possibility of infection with any other.
According to the main signs and characteristics, viral hepatitis can be divided into two groups. Hepatitis A and E are characterized by a fecal-oral mechanism of infection - through water, food, and as a result of household contacts. Hepatitis B, C, D and G are characterized by so-called parenteral transmission of the virus - through damaged skin, mucous membranes with infected blood. The second group is distinguished by a tendency to a protracted and chronic course. Separately, all viral hepatitis have their own characteristics. Knowing them in general terms is useful for every person. This will allow you to consciously follow the rules of behavior that prevent infection. All known hepatitis viruses are registered among the population living in Russia. Russia is one of the regions of the world with an average prevalence of hepatitis A, B, C and D and a low prevalence of hepatitis E.
Hepatitis A
Hepatitis A is a widespread infection. In the early 70s, the World Health Organization legalized the current name of the disease; before that time it was called Botkin’s disease, infectious jaundice, epidemic hepatitis, etc.
This infection is found everywhere.
Who causes the disease?
The causative agent of hepatitis A is the hepatitis A virus (in medical literature it is abbreviated as HAV) - an RNA virus that was discovered recently, and to date more than 30 of its varieties have already been described. The hepatitis A virus is considered one of the most resistant to environmental influences and is well preserved in it; when boiled, it dies after 5 minutes.
How can you get infected?
A person can become infected with hepatitis A through the mouth by consuming contaminated water or food; in children, this happens when toys and other objects get into the mouth, as well as dirty hands. Having penetrated the human body, the hepatitis A virus intensively multiplies in the liver, from there through the bile ducts it enters the intestines and then into the external environment. The spread of the virus and, accordingly, an increase in the risk of infection is facilitated by the unsatisfactory sanitary condition of the home and place of work, inappropriate personal hygiene rules, overcrowding of the population, as well as violation of the rules of food preparation and storage. Serious shortcomings in providing the population with good-quality drinking water lead to the spread of hepatitis A.
How does the disease manifest?
The clinical manifestations of the disease are very diverse: from imperceptibly occurring anicteric forms to severe illness with jaundice. From the moment of infection to the appearance of symptoms, an average of 3-4 weeks passes, in rare cases up to 7 weeks. The onset of the disease is acute. There is a short-term increase in temperature (2-3 days) to 38-38.5°C, moderate headache, and muscle pain. At the same time, appetite decreases, bitter belching, nausea, vomiting, weakness, fatigue, dull pain in the epigastric region and right hypochondrium appear. On the 5th-7th day of illness, icteric staining of the sclera, mucous membranes and skin appears. As a rule, with the appearance of jaundice the patient’s well-being improves. During the icteric period, urine becomes dark yellow or brown (the color of dark beer), and feces become discolored. Often patients themselves note the appearance of a jaundiced coloration of their skin, which forces them to see a doctor.
Diagnostics.
A biochemical analysis of blood and urine helps to make a diagnosis, but the final diagnosis (due to the similarity of manifestations in the acute period of all viral hepatitis) is made only on the basis of special immunodiagnostic methods.
Treatment
Treatment must be carried out in a hospital. Bed rest, diet, vitamins, and infusion therapy are prescribed.
Outcome of the disease:
In the vast majority of cases, hepatitis A, regardless of the severity of the course, ends with complete recovery of the patient and restoration of his liver function. The transition from acute to chronic hepatitis is not observed, complications are rare. With hepatitis A, there is no long-term carriage of the virus in the body after recovery.
Who is most at risk of infection:
-children and adolescents in closed or semi-closed groups;
- workers servicing sewer systems;
-organized contingents, for example, units of the armed forces, which are sent to regions with unsatisfactory sanitary conditions.
What helps reduce the incidence of hepatitis A?
-creation of satisfactory sanitary and hygienic living conditions;
-quality water supply;
- modern arrangement of children's and adolescent institutions;
- compliance with the regime at public catering establishments;
-compliance with personal hygiene rules.
Personal prevention measures:
— Never use water from random sources and reservoirs. In the absence of a reliable source of water, it must be boiled not only for drinking purposes, but also for washing vegetables and fruits.
— When identifying a patient with hepatitis A, you should follow the recommendations of doctors to isolate the patient and carry out disinfection at home. Recently, in some professional groups, as well as among people traveling to areas with high incidence, vaccination against hepatitis A has begun.
— When contacting a patient, immunoglobulin administration is practiced in children's institutions and families. You should not refuse the offer to administer it to your child; the protective effect of this drug has been proven, as well as its harmlessness.
Hepatitis B
This infection, caused by the hepatitis B virus, is a common human disease. Until the 70s it was called serum hepatitis. The disease is characterized by a variety of clinical manifestations and outcomes. In clinically pronounced cases, symptoms of acute liver damage and intoxication are characteristic.
The disease can occur unnoticed, in an anicteric form and is often not diagnosed. For every 1 icteric hepatitis there are 5-6 anicteric (atypical) hepatitis. Hepatitis B is characterized by asymptomatic virus carriage, which causes certain difficulties in preventing this infection. A person can remain a carrier of the virus for life.
Who causes the disease?
The causative agent of the disease is a DNA virus that is very resistant to high temperatures. The peculiarity of the pathogen is its high contagiousness, higher than that of HIV infection. The virus is stable in the external environment: at room temperature - up to 3 months, in the cold season - up to 6 months, when frozen - up to 15 years.
Who is the source of infection?
The source of infection is patients with acute, protracted and chronic forms of the disease, as well as virus carriers.
How can you get infected?
Infection with the hepatitis B virus occurs when it enters the bloodstream through natural and artificial means:
- Natural routes of transmission:
- sexual tract. During sexual intercourse, regardless of the method of its implementation, through semen, vaginal discharge and blood (microscopic, invisible to the eye injuries to the surface of the genital organs and rectum). All this is possible during unprotected sex, and much more often during homosexual contacts. For obvious reasons, an increased risk of infection exists among people who are promiscuous and prostitutes.
- vertical path - from mother to child during pregnancy, during childbirth and after childbirth, during child care and breastfeeding.
— transmission of the virus is also possible through close household contacts, through blood-contaminated razors, toothbrushes, washcloths, etc. In addition, transmission of the virus is possible during work activity - through abrasions, invisible microtraumas.
- Artificial routes of transmission of infection are associated with medical procedures, such as injections, surgeries, and also during the provision of dental care. The virus can be transmitted through blood-contaminated needles, instruments, blood transfusions, as well as through tattooing and piercing. People who use drugs through intravenous injection are especially susceptible to infection.
How does the disease manifest?
There are acute and chronic course of the disease, as well as virus carriage.
Acute course. The period from infection to the onset of the disease can last from 30 days to 6 months (most often 60-120 days). This circumstance complicates the establishment of the possible cause of the disease. The onset of the disease is often gradual. The following come to the fore: loss of appetite, nausea, vomiting, heartburn, belching, dull pain in the epigastrium. After 2-3 weeks, the urine darkens, the feces become light, jaundice appears, digestive disorders and intoxication symptoms intensify: weakness, fatigue, headache, apathy, irritability. Possible skin itching. The disease can occur in an anicteric or erased, weakly expressed form, which is difficult to suspect and can only be detected with the help of special laboratory tests.
Chronic forms are characterized by a change in the active course of the disease with its extinction, but with a gradual deterioration of the condition, the development of cirrhosis of the liver and, in 90% of cases, the death of patients.
Diagnostics.
A biochemical analysis of blood and urine helps to make a diagnosis, but the final diagnosis (due to the similarity of manifestations in the acute period of all viral hepatitis) is made only on the basis of special immunodiagnostic methods.
Treatment
Treatment must be carried out in a hospital. Bed rest, diet, vitamins, and infusion therapy are prescribed.
Outcome of the disease
In most cases, acute hepatitis B ends in recovery. In a small proportion of patients (10%), the disease can take a protracted course. If the disease lasts more than 6 months, it is regarded as chronic hepatitis.
Prevention
Measures to prevent the transmission of the hepatitis B virus and pathogens of other infections with a similar transmission mechanism are regulated in the documents of the Ministry of Health of the Russian Federation.
— special attention is paid to monitoring blood donors. All transfused blood is subject to mandatory laboratory testing for the presence of hepatitis B, C, AIDS, etc. viruses.
— examination of pregnant women, patients with sexually transmitted diseases, drug addicts, prostitutes, conducting anonymous examinations.
— the use of disposable needles, syringes, and other instruments eliminates the possibility of transmitting infection.
— Vaccination is an effective preventive measure against hepatitis B. In our country, since 1996, the so-called specific prevention of hepatitis B began, that is, the introduction of a vaccine among newborns and adolescents. By order of the Russian Ministry of Health, vaccination against hepatitis B was included in the National Calendar of Preventive Vaccinations in 1997, which is enshrined in the Federal Law “On Immunoprophylaxis of Infectious Diseases.” In 2006-2007 As part of the national project, the population is immunized against hepatitis B.
Hepatitis C
Hepatitis C is the most severe form of viral hepatitis, which is also called post-transfusion hepatitis or non-A non-B hepatitis. This means that they became ill with it after a blood transfusion, since testing donor blood for the hepatitis C virus began only a few years ago, when laboratory methods for detecting the hepatitis C virus appeared.
The causative agent of the disease is the hepatitis C virus, which is highly variable. Protective immunity is not developed to it and this does not allow the creation of a vaccine to prevent hepatitis C.
Infection occurs in the same way as with hepatitis B, through blood, sexual contact and from mother to fetus. Quite often, infection occurs through syringes among drug addicts.
The period from infection to the appearance of the first symptoms of the disease is from 3 weeks. up to 6 months The disease can occur with or without jaundice. The clinic of acute hepatitis C is similar in its clinical manifestations to the clinic of hepatitis B. The greatest danger is the chronic form of this disease, which often develops into cirrhosis and liver cancer. The chronic course develops in approximately 70-80% of patients and its development does not depend on the severity of the acute disease, it occurs gradually, over a long period of time (up to 20 years). When hepatitis C is combined with other forms of viral hepatitis, the disease becomes more severe and can result in the death of the patient.
Prevention includes the same measures as for hepatitis B, with the exception of vaccination.
Hepatitis D
Hepatitis D or delta infection is characterized by a more severe course than other viral hepatitis. A prerequisite for its development is the presence of the hepatitis B virus in the body. It has been established that about 5% of hepatitis B virus carriers are also infected with the D virus.
The causative agent of the disease is a virus that does not have its own envelope and realizes itself only in the presence of a helper virus, that is, the hepatitis B virus.
The source of the disease is sick people or virus carriers.
Infection with hepatitis D occurs only when the virus enters directly into the bloodstream naturally (sexually, from mother to child during pregnancy, through close household contacts) or artificially (during injections or other medical procedures, intravenous drug administration). The virus enters the liver through the bloodstream, where it multiplies, leading to the development of an acute disease.
From the moment the D virus enters the body until the onset of illness, 8-10 weeks pass. The disease is characterized by a more pronounced acute onset, with symptoms characteristic of many other diseases: fatigue, decreased appetite, nausea, vomiting, fever. And only with the appearance of a yellow color of the skin and sclera, dark urine and light-colored stool, an increase in intoxication and the appearance of pain in the right hypochondrium (in the liver area), allows an accurate diagnosis to be made, confirming it with laboratory tests. Hepatitis D is characterized by bleeding gums, nosebleeds, and bruising due to minor injuries, which is associated with impaired formation of blood clotting components in the liver.
The disease often becomes chronic, followed by the development of liver cirrhosis.
Prevention, as with hepatitis B.
Hepatitis E is similar to hepatitis A, but it starts gradually and is more dangerous for pregnant women. The last in the hepatitis family, hepatitis G , is similar to C but less dangerous.
PREVENTION OF HEPATITIS
1. Today, the most accessible and reliable method of prevention is vaccination. Vaccination of newborns has been carried out since 1984 in more than 100 countries around the world. There are vaccines against hepatitis A and B. Vaccination against hepatitis B is included in the National Vaccination Schedule. The vaccine is administered intramuscularly (into the deltoid muscle) according to the 0-1-6 scheme, i.e. twice with an interval of 1 month and subsequent revaccination 6 months after the first administration of the vaccine. The production of antibodies is observed in 94% of vaccinated people. In addition, vaccination against hepatitis B was included in the program of the priority national project “Health” for 2006-2007 with the goal of not only reducing the frequency of new cases of infection, but also significantly reducing the number of long-term consequences of infection with the hepatitis B virus.
2. To avoid infection of family members, it is necessary to observe basic rules of personal hygiene - individual use of a toothbrush, razor, manicure accessories, towels. It is necessary to protect children from contact with these objects.
3. The use of barrier contraceptives (condoms) is mandatory for persons with frequent changes of sexual partners. It is especially important to take precautions during sex during menstruation and anal intercourse, but oral sex can also be dangerous. Avoid promiscuity because using a condom does not provide 100% protection against sexually transmitted infections.
4. Never use drugs. Indeed, in addition to the harm caused to your body, drug use, especially by injection, increases the risk of developing such terrible diseases as AIDS and infectious hepatitis. If you cannot refuse them and get out of addiction, never share needles, syringes, solutions or any similar devices with anyone, and do not use others. Also try not to abuse alcohol, because acute and chronic viral hepatitis, which develops against the background of alcohol abuse, has a more severe course and more often an unfavorable outcome, since liver function is initially impaired under the influence of the toxic effects of alcohol.
5. If you are a medical worker, then you should always follow safety precautions, especially when working with any sharp objects. Get vaccinated against hepatitis B.
6. If you come to a medical facility or dental office, make sure that all potentially dangerous manipulations are performed with gloves and only with disposable instruments.
7. Think carefully before you go and get a tattoo or piercing, and watch where and to whom you are going. The master must work with gloves and disposable sterile instruments.
What to do if you are diagnosed with HBsAg?
Unfortunately, hepatologists are often faced with underestimation on the part of the patient, as well as doctors of other specialties, of the seriousness of HBsAg detected over many years. A patient who is diagnosed with HBsAg for the first time must undergo an examination, which will make it possible to make a correct diagnosis - to distinguish between inactive carriage of HBsAg and active chronic hepatitis B that requires treatment. To do this, the hepatologist will suggest that you do a number of studies: - a study of a biochemical blood test, - a study of the viral load using quantitative PCR (polymerase chain reaction) - a study for the presence of another protein (or antigen) of the hepatitis B virus, which characterizes the high infectiousness of the patient, — HBeAg — study for the presence of a companion virus of hepatitis B - delta virus — study of alpha-fetoprotein (tumor marker of a liver tumor) — ultrasound examination of the liver — fibroelastography to clarify the stage of liver fibrosis (other studies are possible according to indications)
Who is at risk
- Those who are promiscuous and have a non-traditional sexual orientation. To minimize the chance of contracting hepatitis B, contraception should be used;
- Injecting drug addicts using poorly disinfected syringes;
- Infants born from sick mothers;
- Those undergoing hemodialysis, if medical specialists do not follow precautionary measures;
- Tourists vacationing in countries with unfavorable epidemiological conditions;
- Family members of a hepatitis patient who do not follow hygiene rules;
- Those working in the healthcare sector and in direct contact with infected people;
- Those serving sentences in penitentiary institutions.
People at risk need to know exactly how hepatitis B is transmitted. They should undergo regular testing for the presence of the virus, and if it is detected, begin treatment immediately. Remember: the result of the fight against this dangerous pathology depends on the timeliness and adequacy of therapy.
Modern treatment of chronic hepatitis B can stop the disease!
If you are nevertheless diagnosed with chronic hepatitis B, it is necessary to prescribe antiviral treatment, that is, treatment using drugs that can block the replication of the virus.
The goal of modern antiviral therapy for chronic hepatitis B is to persistently suppress the replication of the virus, achieve remission of the disease, that is, transfer the process to an inactive state. When this result is achieved, the development of liver cirrhosis and its complications (such as ascites, internal bleeding, liver failure) is prevented, and the risk of developing liver cancer is greatly reduced.
A number of drugs with antiviral effects are currently registered for the treatment of chronic hepatitis B. Among the new generation of drugs there are safe drugs that can be used for several years, drugs to which the virus does not develop resistance. Your attending physician will help you choose a treatment appropriate to the stage and form of your disease.
Symptoms
The incubation period for hepatitis B lasts on average 75 days, but can increase to 180 days. The virus can be detected 30-60 days after infection.
During the acute infection stage, most people do not experience any symptoms. However, for some, acute hepatitis B infection may cause symptoms that last several weeks, including yellowing of the skin and eyes (jaundice), dark urine, extreme tiredness, nausea, vomiting, and abdominal pain. A relatively small number of patients with acute hepatitis may develop acute liver failure, often leading to death (fulminant hepatitis).
In some people, the hepatitis B virus can also cause a chronic liver infection that can later develop into cirrhosis or liver cancer.
Complications after an illness
Hepatitis B is dangerous because of its consequences: it is one of the main causes of liver cirrhosis and the main cause of hepatocellular cancer of the liver. The likelihood that hepatitis B virus infection will become chronic depends on the age at which a person acquires the infection. Children most likely to develop chronic infections are those infected before the age of six:
- chronic infections develop in 80-90% of children infected during the first year of life;
- Chronic infections develop in 30-50% of children infected before the age of six.
- 15-25% of adults who become chronically infected during childhood die from liver cancer or cirrhosis.
Among adults:
- Chronic infections occur in <5% of infected, otherwise healthy adults;
- 20%-30% of chronically infected adults develop cirrhosis and/or liver cancer.
The probability of complete recovery from chronic hepatitis B is very low - about 10%. But a state of relative health (remission), in which the virus practically does not bother the patient, can be achieved in more than 80% of cases.
Is it necessary to follow a diet for patients with chronic hepatitis B?
No special diet is required for chronic viral hepatitis, however, you should avoid drinking alcohol even in small doses, since the combined effect of alcohol and the virus on the liver significantly increases the risk of developing cirrhosis and liver cancer. If you are overweight, you should limit your intake of fats and high-calorie foods, since fat deposition in the liver accelerates the development of cirrhosis. Factors that reduce immunity, in particular sun exposure, should be avoided, that is, you should not use a solarium or sunbathe on the beach. It is advisable to quit smoking. You can continue to exercise. Swimming and hardening procedures that support the state of your immunity are useful.
Routes of transmission of viral hepatitis B in adults
Blood is the main source of hepatitis B virus. It can also be found in other tissues and body fluids, but in lower concentrations.
The hepatitis B virus can be transmitted in several ways.
Through blood.
This may happen in the following cases:
- punctures of the skin with infected needles, lancets, scalpels or other sharp objects;
- direct contact with open sores of an infected person;
- splashes of infected blood on the skin with minor scratches, abrasions, burns or even minor rashes;
- splashes of blood on the mucous membranes of the mouth, nose or eyes;
- using other people's toothbrushes or razors.
Contact with surfaces contaminated with blood can also cause illness, but to a lesser extent.
By the way, the virus can remain stable in dried blood for up to 7 days at 25 °C.
Hand contact with blood-contaminated surfaces such as laboratory benches, test tubes, or laboratory instruments can transmit the virus to the skin or mucous membranes.
Through saliva.
The saliva of people with hepatitis B may contain the virus, but in very low concentrations compared to blood. Nevertheless, infection is possible, for example, through bites.
But it is impossible to become infected through dishes or mouthpieces (smoking or musical instruments) - such cases have not been registered.
Through semen or vaginal secretions.
Hepatitis B is found in semen and vaginal secretions. The virus can be transmitted during unprotected sex and from mother to child during childbirth.
Feces, nasal discharge, sputum, sweat, tears, urine, and vomit do not spread hepatitis B. Unless they are contaminated with blood, the risk of contracting hepatitis B from these fluids is very low.
Synovial fluid (lubricant for joints), amniotic fluid, cerebrospinal fluid, and peritoneal fluid (found in the abdomen) may contain hepatitis B virus, but the risk of transmission is unknown.
Hepatitis B is not spread by sneezing, coughing, shaking hands, hugging, kissing, breastfeeding, or sharing cutlery, water, or food.
Symptoms of viral hepatitis B in adults
The main symptoms of hepatitis B include:
- dark urine;
- clay-colored stool (gray-white);
- jaundice;
- heat;
- joint pain;
- abdominal pain;
- fatigue;
- lack of appetite;
- nausea, vomiting.
Symptoms may vary depending on the person's age.
Many people may not show symptoms (asymptomatic disease). A very small proportion of patients develop a critical form of the disease called fulminant hepatitis B. This condition occurs as a result of a sudden loss of liver function.
Prevention of viral hepatitis B in adults at home
The most reliable prevention is vaccination.
Since 2000, it has been administered to all children, starting at birth. And more recently, for adults too. Vaccines provide safe and reliable protection—tests show that 90 to 95% of vaccinations in healthy people result in resistance to hepatitis B. Hepatitis B vaccination is safe. Side effects are usually minor, most often soreness at the injection site.
A contraindication to vaccination is an allergy to any ingredients of the vaccine.
Treatment of hepatitis B in the chronic stage
Treatment of hepatitis B can take about six months if the disease is advanced. Dormant hepatitis does not require antiviral treatment. Therapy with interferon-Alpha, zidovudine and lamivudine is effective in increasing the inflammatory process when the virus leaves the liver cell. The drugs are able to stop the replication of the DNA of the microorganism, prevent the malignancy of the disease and the development of cirrhosis. Otherwise, the treatment of hepatitis B does not differ from that described above - diet and detoxification.
Very often there is a situation in which people attribute poor health to stress or a sedentary lifestyle and try to correct the situation by active sports. Treatment of hepatitis B in men is especially complicated, since it is they who most often violate doctors’ orders and seek to get rid of the disease through increased activity, and often alcohol. The patient's liver is not able to cope with its function as a natural filter and acute intoxication may occur. This absolutely cannot be allowed!
TREATMENT OF HEPATITIS B IS AVAILABLE IN BRANCHES:
Treatment of hepatitis B in the Primorsky region
Address: St. Petersburg , Primorsky district, st. Repisheva, 13
Treatment of hepatitis B in the Petrograd region
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
Treatment of hepatitis B in Vsevolozhsk
Address: Vsevolozhsk , Oktyabrsky Prospekt, 96 A
Treatment information
In 90% of cases, acute hepatitis B is treatable. The patient's recovery occurs 1-6 months after the start of therapy. The prognosis improves markedly when symptoms of the disease are detected at an early stage. Diagnosis and treatment of all forms of viral hepatitis B is carried out by a hepatologist or infectious disease specialist. In a chronic course, the prognosis is poor, recovery is impossible, the patient will die in 6-10 years due to complications.
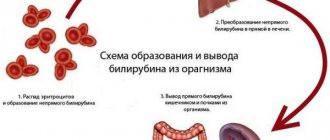
Diagnosis of hepatitis B is achieved by detecting specific virus antibodies in the serum and immunoglobulins to them in the blood. Using a PCR test, the DNA of the virus is isolated to assess activity. Serological tests ELISA and RIA are carried out.
Treatment of hepatitis B should be supervised by a specialist. Self-medication will not lead to good results. Therapy is based on several principles:
- detoxification of the body;
- support of vital functions;
- strengthening the immune system;
- diet;
- suppression of symptoms.
For mild hepatitis, a gentle diet is necessary. The patient should eat in small portions 5-6 times a day, stay in bed, getting up only for self-care. If the condition is moderate, detoxification drugs are administered by drip, hepatoprotectors are used to protect cells from destruction, and vitamins are used. In severe cases, treatment is provided in intensive care.