Alcoholic hepatitis is a complex of inflammatory and degenerative processes that occur in the liver and manifest as a result of regular consumption of alcohol-containing products. The definition is adopted in ICD-10, the classification of the disease according to it is K70.1.
The likelihood of developing the disease directly depends on how much and how often a person drinks alcoholic beverages.
It is important to take into account that the type of alcohol does not matter here; any alcohol-containing product can cause illness.
The pathology does not form immediately; with systematic intake of ethanol, a person initially develops fatty liver disease, only after alcoholic steatohepatitis. At the last stage, the disease progresses to cirrhosis. With this pathology, Dupuytren's contracture may develop, which is especially common in middle-aged men.
Alcoholic hepatitis is not dangerous to others, it is not contagious.
General information
Among the forms of chronic liver diseases, alcoholic liver disease occupies 24%. Alcoholic liver disease is a group of diseases that result from long-term alcohol abuse. These are sequentially developing conditions - from liver steatosis to cirrhosis , which are stages of one process. Alcohol has a toxic effect on liver cells and alcoholic toxic hepatitis .
Long-term and daily use is more dangerous than occasional alcohol consumption because it allows the liver to repair and regenerate. The toxic effect depends on the dose of ethanol and does not depend on the type of drink: 10 g of ethanol is contained in 25 ml of vodka, 200 ml of beer and 100 ml of wine. Patients do not classify beer as such, but meanwhile, daily consumption of this drink is enough for the development of hepatitis. It has been established that a risky dose of ethanol for the development of liver damage is daily consumption of 30-60 g of ethanol, a dangerous dose is 60-80 g, and a cirrogenic dose is considered to be 80-160 g. Women are more sensitive to alcohol, and they often develop severe forms of the disease with prolonged use of small doses of alcohol. The diagnosis is established on the basis of regular alcohol consumption, the presence of clinical changes and laboratory and instrumental abnormalities. The urgency of the problem lies in the fact that this pathology is associated with a high risk of developing liver cirrhosis , which leads to disability and death. Liver cirrhosis is the culmination of the disease. The ICD-10 code for alcoholic cirrhosis is K70.3.
Content:
- Causes of the disease
- How does alcoholic liver hepatitis occur?
- Classification varieties
- Symptoms
- Diagnostics
- Treatment
In addition to its intoxicating effect, alcohol has a pronounced toxic effect on the human body. Alcohol affects almost all organs. The brain is destroyed the most and fastest, but the liver gets a “double” blow. Its anatomical structural units - hepatocytes - not only suffer and undergo destruction, but are also forced to neutralize ethanol, decomposing it into safe compounds. Therefore, one of the most common and dangerous complications of drunkenness is alcoholic hepatitis. This disease leads to inflammatory changes in tissue. Subsequently, fatty degeneration develops. Its outcome is fibrosis, which gradually turns into cirrhosis - the replacement of cells with connective tissue, which becomes a causative factor in the complete loss of its main functions.
Pathogenesis
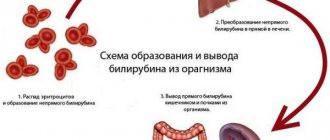
acetaldehyde, plays a role in liver damage . It enters into a chemical bond with intracellular components (proteins in the first place) and disrupts their functions. Under the influence of acetaldehyde, the cell membrane and phospholipids are destroyed, the transport of substances through the membrane is disrupted, and the level of cytokines increases - this is the reason for the appearance of first steatosis , then hepatitis , fibrosis and cirrhosis . When interacting with acetaldehyde, substances with antigenic properties are formed. They, in turn, increase the activity of stellate cells. Activated cells play a major role in fibrogenesis—the development and progression of liver fibrosis. Thus, acetaldehyde causes immune-mediated damage to liver cells. In addition, in people who drink alcohol for a long time, intestinal permeability increases significantly. As a result, waste products of intestinal bacteria enter the bloodstream, in response to which pro-inflammatory cytokines and tumor necrosis factor TNFα are produced, which damages hepatocytes and is of great importance in the development of alcoholic hepatitis. With the development of cirrhosis, the liver venules expand, the arterioles narrow, which leads to an increase in pressure in the portal vein system (portal hypertension develops with characteristic manifestations - varicose veins of the stomach, esophagus, anterior abdominal wall, enlarged spleen and ascites).
The effect of alcohol on the liver
The breakdown of alcohol begins when it enters the human stomach. The juice constantly contains the enzyme alcohol dehydrogenase, which oxidizes up to 25% of the ingested ethanol and converts it into acetaldehyde. Thus, ¼ part is absorbed into the blood bypassing the liver. The presence of food (especially fatty foods) delays absorption, but does not neutralize toxic products.
The opposite effect is possible if the patient is taking medications from the group of H2-histamine receptor blockers. They reduce the concentration of alcohol dehydrogenase in the stomach and sharply increase the volume of ethanol entering the blood.
Alcohol is carried by the bloodstream to all organs, enters any fluids and tissues, causing significant damage to the functioning of cells.
The enzymatic system of the liver enters the fight for neutralization due to its specific active proteins. The transformation reaction begins with the action of alcohol dehydrogenases and the transformation of ethanol into acetaldehyde (aka acetaldehyde, ethanal, methyl formaldehyde).
The substance is several tens of times more dangerous in its toxic properties than alcohol itself. It is classified as a first-order carcinogen due to its ability to destroy the DNA of genes and cause cancerous degeneration. Therefore, the negative consequences of the action, in addition to alcoholic hepatitis, include the development of malignant tumors of the stomach, esophagus and liver. Further transformation occurs under the influence of acetaldehyde dehydrogenase. It converts methyl formaldehyde into acetic acid and non-toxic substances that are excreted in the urine.
It is important that with constant consumption of alcoholic beverages, the synthesis of necessary enzymes lags behind the need. This leads to increased exposure of the liver to undegraded acetaldehyde. Liver cells (hepatocytes) respond with an inflammatory response.
In the pathogenesis of alcoholic hepatitis, damage to other organs of the digestive system plays a significant role:
- pancreas (pancreatitis);
- stomach (gastritis);
- gallbladder (cholecystitis).
Classification
Alcoholic liver disease has main forms:
- Alcoholic steatosis (alcoholic fatty infiltration).
- Acute or chronic alcoholic hepatitis (synonymous with alcoholic steatohepatitis).
- Alcoholic fibrosis and cirrhosis .
According to severity, alcoholic hepatitis is:
- Easy.
- Moderate weight.
- Heavy.
According to the flow, hepatitis is divided into:
- Persistent. It has a stable course and with proper treatment and avoidance of alcohol, the process is reversible.
- Progressive. It is characterized by deterioration of well-being and gradual progression of the process.
- cirrhosis , liver failure with encephalopathy and hepatic coma develops .
Cirrhosis is divided into stages:
- Stage I or A (compensated). At this stage, there are either no or mild manifestations.
- Stage II or B (it is considered subcompensated). Signs of organ dysfunction and portal hypertension .
- Stage III or C (this is the stage of decompensation). Signs of liver failure and portal hypertension are increasing.
Alcoholic steatosis (hepatosis) is the most common and widespread form of liver damage in alcoholism. It develops in 90% of people who drink 60 g or more of alcohol. Characterized by the accumulation of fat droplets inside the liver cells. Uncomplicated steatosis is asymptomatic or its manifestations are minor: heaviness in the right hypochondrium, slight enlargement of the liver, nausea and intolerance to fatty foods.
Liver test values remain normal or slightly elevated, and elevated alkaline phosphatase levels are associated with cholestasis (intrahepatic bile stagnation). Liver enlargement occurs due to an increase in hepatocyte organelles, which are involved in the metabolism of alcohol, and is considered as a reaction to a constant alcohol load. The degree of liver enlargement is directly related to the severity of fatty degeneration. However, when you give up alcohol, alcoholic steatosis decreases after 4-6 weeks and can completely disappear (intracellular fat deposits disappear).
Acute alcoholic hepatitis is a severe form of alcoholic liver disease. It is associated with toxic liver necrosis , which occurs when large doses are taken during binge drinking. It occurs against the background of chronic liver diseases - viral hepatitis or cirrhosis and poses a threat to life. There are several forms: icteric, latent and fulminant alcoholic hepatitis. The latter is characterized by a severe course, develops rapidly and has a high mortality rate. The risk of developing it increases in such patients when taking paracetamol (even moderate doses). The patients are in serious condition, they develop jaundice, fever, nausea, ascites renal failure quickly develops .
The disease ends in hepatic coma, and a few weeks later - in the death of the patient. The icteric form is the most common. In addition to jaundice, the patient is worried about pain, nausea, vomiting, lack of appetite, itching, fever up to 39-40°C. Also, stool is discolored and dark urine appears. Often ascites and bacterial complications ( pneumonia , peritonitis , pyelonephritis , lung abscess ). Patients experience mental disturbances, they are agitated, and sleep is disturbed.
Unfavorable signs are:
- Jaundice with bilirubin level more than 300 µmol/l.
- Ascites.
- Encephalopathy.
- Development of DIC syndrome.
The latent version of hepatitis is manifested by moderate pain, nausea, and belching. Hepatitis is the stage at which treatment is effective.
Chronic alcoholic hepatitis has the following forms: with minimal activity, moderate activity and severe. Chronic hepatitis against the background of alcoholism with moderate activity is characterized by scant manifestations: weakness , dyspeptic symptoms , decreased performance. Hepatitis C with severe activity is considered a continuation of acute hepatitis. The icteric form is most often observed, but the jaundice is not pronounced, there is no skin itching, nausea and weight loss, asthenia, a slight enlargement of the liver are bothersome, and sometimes ascites develops. The disease progresses even if the patient stops drinking alcohol.
Chronic alcoholic hepatitis always occurs with concomitant diseases - pyelonephritis , pancreatitis , pulmonary tuberculosis , encephalopathy , pneumonia , muscle atrophy, pathology of the cardiovascular and nervous system, alcoholic polyneuropathy . In a biochemical blood test - an increase in transaminases by 2-5 times depending on the degree of activity, an increase in bilirubin , alkaline phosphatase and cholesterol , as well as immunoglobulin A.
Alcoholic liver fibrosis occurs latently and develops gradually. In 60% of patients who drink 40-80 g of alcohol per day, fibrosis develops within 25 years. It initially appears in the area around the liver veins. The reason for its development is the ability of ethanol to stimulate the growth of connective tissue. At this stage, patients complain of constant pain in the right hypochondrium, weakness and fatigue. On examination, there is a moderate enlargement of the liver. A needle biopsy of the liver is necessary to determine the stage of fibrosis. Further alcohol abuse inevitably leads to the development of cirrhosis .
Alcoholic cirrhosis of the liver. This is the final stage of alcoholic organ damage. The disease is characterized by a poor prognosis, even if the patient stops drinking alcohol, since cirrhosis has a high risk of hepatocellular carcinoma. The symptoms of cirrhosis vary, which is associated with the degree of organ dysfunction, the stage of cirrhosis and the severity of portal hypertension.
Variceal bleeding worsens the course of the disease, as it is often followed by ascites , encephalopathy , and deterioration to coma . Patients exhibit signs of protein and vitamin deficiency; they have a characteristic appearance (pseudo-Cushingoid). Encephalopathy is a serious complication that often ends in coma and death. Manifests itself with psychoneurological symptoms: agitation or inhibition, decreased reaction, hallucinatory disorders, stuporous state. If the onset of coma is acute, then precoma rapidly develops with agitation and vomiting, and then the patients fall into a coma and paresis of the limbs appears. If the development of coma is slow, then the prodromal period with encephalopathy and jaundice lasts several days or even weeks. Pain in patients with cirrhosis is caused by pancreatitis, and pain in the liver area is not typical. If constant pain occurs, cirrhosis-cancer .
Methods of treating the disease
Alcoholic hepatitis is treated and diagnosed by a gastroenterologist or hepatologist. Treatment is carried out comprehensively, taking into account the fact that most patients are dependent on alcohol. Therefore, rehabilitation is often carried out with the involvement of other doctors (nutritionist, psychiatrist, narcologist, psychotherapist, etc.).
Depending on the complexity of the disease, various treatment methods are used. In mild forms, the patient is offered drug treatment with hepatoprotectors. But if a severe form of the disease is observed, the doctor may prescribe antibiotics. These drugs help prevent infectious complications.
The last stage of the disease cannot be treated and the use of various drugs is not able to provide a positive effect. In this case, the only option for the patient is a liver transplant. This comes with a number of difficulties. First of all, this is an expensive procedure that many simply cannot afford. And secondly, it is necessary to find a healthy donor organ. A relative of the patient can act as a donor. The operation involves transplanting up to 60% of the liver, which over time regenerates and grows to normal size.
Causes
Alcohol abuse, which is to some extent associated with genetic predisposition. In half of the cases, the predisposition to addiction is inherited and is associated with changes in the GABRA2, PNPLA3 and PARy2 genes. It was found that carriers of the PNPLA3 gene mutation have a 2.8-fold increased risk of liver cirrhosis.
There is a connection with chronic viral hepatitis. The combination of hepatitis C virus and alcoholism causes more significant organ damage.
It is also worth noting the factors influencing the development of severe alcoholism:
- dose and duration of use;
- type of alcohol;
- gender (in this case female);
- obesity;
- nutritional imbalance (consumption of excess fat, lack of vitamins and proteins);
- trophological deficiency.
Differential diagnosis of chronic form
Diagnostics needs to identify differences with non-alcoholic steatohepatitis in metabolic disorders and drug-induced hepatitis. Metabolic steatohepatitis is more often observed in women aged 40 to 60 years who suffer from:
- obesity,
- diabetes mellitus
At the same time, triglycerides accumulate in the liver, which can damage cell membranes and stimulate the development of fibrous tissue (the path to cirrhosis).
A blood test reveals a violation of the composition of fat components, a sharp increase in triglycerides, and hyperglycemia. There is no jaundice in the symptoms. Drug-induced steatohepatitis occurs as a result of side effects of medications with long-term use:
- drugs from the estrogen group;
- Amiodarone;
- high doses of acetylsalicylic acid;
- Sulfamethoxazole;
- calcium antagonists;
- anti-inflammatory drugs of the aminoquinolone series (Delagil, Plaquenil).
In the pathogenesis of this type of hepatitis, it is important to suppress the process of fatty acid oxidation at the level of hepatocyte mitochondria and activate the peroxide type of lipid oxidation. The doctor can find out what drugs the patient took, their dangerous dosage and duration of treatment. The outcome of non-alcoholic steatohepatitis also becomes cirrhosis of the liver. Rarely, fatty degeneration is droplet in nature and causes a fulminant form of acute hepatitis.
The final confirmation of non-alcoholic lesions can only be based on the results of a liver biopsy. Statistics show the presence of steatohepatitis in 7–9% of cases of all studies. Some experts consider it necessary to take into account the disease as a separate nosology.
Symptoms of alcoholic hepatitis
Manifestations of alcoholic liver damage depend on the type of damage and its severity. Thus, alcoholic hepatosis is asymptomatic or with minimal symptoms. Patients are concerned about periodic heaviness in the hypochondrium on the right, which appears after drinking alcohol, nausea and poor tolerance to fatty foods. On examination, the liver is enlarged; liver test results are normal or elevated. An increase in the level of alkaline phosphatase is characteristic.
Symptoms of alcoholic hepatitis are variable, depending on the activity of the process. Most often, hepatitis occurs with increasing jaundice, which is the main symptom, weight loss, fever, nausea, and decreased appetite.
The development of jaundice is associated with fever, weight loss, and nutritional deficiency (nutrition deficiency). In severe cases, jaundice is observed in 100%; in such patients the temperature rises to 38-40 C. Ascites with hepatitis is rare, but patients have an increased risk of infections.
The severity of hepatitis is determined by the degree of liver dysfunction.
- In mild cases, enzyme activity is three times higher than normal.
- At an average degree - five times.
- In severe cases - more than five times.
Most people experience improved liver function after months of abstaining from alcohol.
Symptoms of alcoholic cirrhosis of the liver depend on the stage of cirrhotic changes. For many years, cirrhosis has been compensated. In the initial stage, patients complain of flatulence , heaviness in the right half of the abdomen, weight loss, and general weakness. In more advanced stages, an enlarged abdomen is observed, dilated veins appear on the abdominal wall (venous collaterals develop), diuresis decreases, there may be an increase in temperature, jaundice, bleeding (nasal and esophageal), redness of the palms (“liver palms”). Dilatation of the saphenous veins on the abdominal wall (“head of the jellyfish”) indicates an increase in pressure in the portal vein system. If there are obstacles to the passage of blood through the liver due to cirrhosis, venous blood is redistributed along bypass outflow tracts.
Dilatation of the veins of the esophagus occurs in half of the patients. Decompensated cirrhosis is manifested by complications: jaundice , bleeding , ascites and encephalopathy . Jaundice develops due to liver failure, and ascites due to increased pressure in the portal vein and sodium retention. Typically, decompensation develops after bleeding and bacterial peritonitis. Both complications are associated with high mortality.
With significant impairment of organ function, hepatic encephalopathy develops. These may be minimal mental disorders or hepatic coma. Hepatic encephalopathy can be episodic (after a provoking factor), recurring (twice a year) and recurrent (develops after interruption of treatment).
Features of the chronic form
Chronic alcoholic hepatitis occurs with long-term constant consumption of alcohol; detection shows its presence in 1/3 of patients with alcoholism. Symptoms are mild and may be completely absent. The diagnosis is made when violations are detected by laboratory methods and compared with the patient’s alcohol history.
A detailed survey reveals some signs of pathology:
- loss of appetite;
- tendency to constant bloating;
- rare attacks of nausea;
- insomnia;
- decreased libido (sexual desire) due to impaired synthesis of sex hormones.
Palpation reveals a dense, painful edge of the liver protruding from under the right hypochondrium, signs of organ enlargement. This form of liver damage is also called alcoholic steatohepatitis, since fatty degeneration occurs in hepatocytes.
According to the clinical course, degrees are distinguished:
- mild – the patient has no complaints, but examination reveals an enlarged liver;
- medium - in addition to the enlarged organ, the patient has obvious pain in the right hypochondrium, yellowness of the sclera and skin, weight loss, loss of appetite;
- severe – characterized by a significant enlargement of the liver and spleen, the onset of cirrhosis.
Tests and diagnostics
In diagnosing alcoholic liver disease, it is important to carefully collect anamnesis (duration of abuse, amount of alcohol consumed, frequency of binges, etc.).
- A clinical blood test allows ( neutrophilic leukocytosis , increased ESR, anemia ).
- Increased total bilirubin, transaminase activity (AST increases more than ALT), alkaline phosphatase and γ-glutamyl transpeptidase (GGTP), decreased albumin .
- Ultrasound of the liver. Different changes are detected at different stages. At the stage of fatty infiltration, the liver is enlarged and has a homogeneous hyperechoic structure (it is described as a “large white liver” that has unclear contours). Chronic ultrasound reveals a moderate or slight enlargement of the liver; the structure of the parenchyma remains fairly homogeneous with a moderate increase in the echogenicity of the organ. With cirrhosis, the liver is enlarged, its contour is uneven, coarsely lumpy.
- The structure of the parenchyma is heterogeneous due to nodes of regeneration and fibrosis. The spleen is enlarged, the splenic vein is dilated (this is an early sign of increased pressure in the portal system), the portal vein is dilated, and free fluid (ascites) is detected in the abdominal cavity.
- Computed tomography is an additional method for determining fatty liver disease.
- During gastroscopy, dilation of the veins of the stomach and esophagus (the risk of bleeding is assessed) and sometimes hepatogenic gastric ulcer .
- Liver biopsy is rarely performed.
Etiology
The most obvious reason for the development is long-term abuse of alcoholic beverages. In this case, not only the amount of alcohol matters, but also the frequency of drinking episodes and the specific type of strong drinks. For most people, the critical dose of ethanol is 80–160 g per day over 10–20 years of regular drinking.
But in women, the disease develops when drinking much smaller doses of alcohol (20–40 g per day) and over a shorter period. This is explained by the smaller number of enzymes involved in the breakdown of ethanol. And if therapy is started too late, in 50% of women the pathology progresses to hepatocellular carcinoma, even if they get rid of addiction.
According to experts, one-time alcoholic excesses (even with significant alcohol abuse) are safer, since a rare intake of alcohol gives the liver the opportunity to “recover”, which cannot be said about daily drunkenness.
In addition, the risk of alcoholic liver toxicosis is increased if:
- genetic characteristics due to which the mechanisms for the production of enzymes that affect the metabolism of alcohol are disrupted;
- being overweight, which provokes the accumulation of visceral fat;
- concomitant viral and infectious liver diseases;
- taking hepatotropic medications (antifungals, antibiotics, immunosuppressants), antiulcer medications that reduce the activity of alcohol dehydrogenase;
- autoimmune diseases.
Diet
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
Diet for hepatitis
- Efficacy: therapeutic effect after a week
- Terms: 6 months or more
- Cost of products: 1400-1450 rubles per week
Diet for liver cirrhosis
- Efficacy: therapeutic effect after 3-4 months
- Terms: lifelong
- Cost of products: 1600-1800 rubles. in Week
For all liver diseases, diet Table No. 5 . In the stage of cirrhosis, when the patient has insufficient protein-forming function of the liver, it is necessary to monitor the intake of protein in the body and maintain it in the amount of 1.2-1.5 g per kg of weight. The main thing is that the patient has a normal energy value of food (at least 2000 kcal) and a sufficient amount of vitamins (group B and folic acid). Patients should be given multiple meals with light snacks during the day and at night.
- Increase the content of foods that provide essential nutrients.
- In case of decompensated cirrhosis with encephalopathy , protein intake should be limited, and in case of ascites , unsalted food is recommended.
- Use nutritional mixtures (orally) for energy malnutrition.
- Use of whole protein mixtures.
- For hepatic encephalopathy - mixtures based on branched chain amino acids (so-called BCAA amino acids).
- For ascites - concentrated and high-calorie mixtures.
- For anorexia, they switch to enteral tube feeding.
- For hyperammonemia, Hepasol A is a special agent for parenteral nutrition.
Treatment at home
When treating alcoholic hepatitis, folk remedies can be used in parallel with taking medications. However, this can only be done after consulting a doctor. The following are the most common remedies for treating alcoholic hepatitis at home:
- Dandelion root. Grind the root to make 1 tbsp. l. Pour the crushed root into 200 ml of cooled boiled water. After this, the product should be put on low heat and simmered for about 1 hour. You need to take the medicine 1 hour before meals, a maximum of 3 times a day.
- Beetroot and radish juice. Chop the vegetables, squeeze the juice out of them, mix in equal proportions. Every day you need to drink 150 ml of juice.
- Dill infusion. Grind the dill to make 1 tbsp. l. Add 1.5 cups of boiling water to the chopped dill and let it brew. You need to drink the product every day.
Consequences and complications
Severe complications occur with liver cirrhosis. Among them it is worth highlighting:
- Variceal bleeding due to portal hypertension .
- Hepatic encephalopathy.
- Ascites.
- Infection. This is a common complication in severe hepatitis and cirrhosis . The most common causes are spontaneous bacterial peritonitis , bacteremia , respiratory infection, and urinary tract infections.
- Hepatorenal syndrome . This is the development of renal failure with severe impairment of liver function.
- Hepatocellular carcinoma.
What does the dose of alcohol matter?
The development of alcoholic hepatitis is due to:
- dose of ethanol contained;
- quality of the alcoholic drink;
- duration of use.
The daily amount of alcohol for the development of hepatitis and cirrhosis of the liver is:
- for an adult man 50–80 g;
- women – 30–40;
- teenager – 15–20.
Doctors categorically deny the safety of beer.
Men drink 3–5 liters at a time, which is equivalent to 120–200 g of ethanol and is 3–4 times higher than the permissible norms
For a teenager, 0.5 liters of “non-alcoholic” beer poses a danger. According to the preparation technology, it must contain up to 5% ethanol. In addition, with beer, the load on the liver increases due to the carbohydrates contained, which are processed into fats and remain in the parenchymal cells.
A special role in the development of the acute form of alcoholic hepatitis is given to poisoning with surrogates of alcohol-containing household liquids. Toxic substances in these cases are, in addition to alcohol:
- isopropyl alcohol;
- diethyl phthalate;
- methyl alcohol;
- polyhexamethylene guanidine hydrochloride (component of disinfectants);
- acetaldehyde.
Most attending physicians (gastroenterologists, hepatologists) consider it important in making a diagnosis not to specify the dose of the drink consumed by the patient, but to determine the regularity of alcohol entering the body.
Forecast
Complete cessation of alcohol consumption is the only factor in increasing the life of patients. How long do people live with alcoholic hepatitis? It depends on the severity of the course (mild, moderate and severe) and the form of hepatitis - persistent or progressive. The first form has a more favorable course and prognosis.
With complete abstinence from alcohol in patients with hepatitis, cirrhosis develops only in 15% of cases. If patients continue to take alcohol, cirrhosis develops in 30-40% of patients, and only 15% of patients survive for two years. Chronic active hepatitis has a poor prognosis as the disease progresses to cirrhosis . With heavy drinking, hepatitis worsens, and patients die from hepatic cell failure. The mortality rate for any liver damage is proportional to protein deficiency. Lack of protein and vitamins A and E significantly worsens the course of the disease. The introduction of unsaturated fats into the diet (flaxseed oil, olive oil, walnuts, flax seeds and chia seeds) has a protective effect on the liver.
If we consider a patient with cirrhosis , then the prognosis is disappointing. For the prognosis, the following indicators are important: ascites albumin levels , bilirubin and prothrombin time , as well as the presence of encephalopathy and stages of cirrhosis - I, II, III. How long do they live with him? Taking into account all these indicators, people with alcoholic cirrhosis live from one to three years. When comparing men and women, women have a 2-fold higher risk of death due to cirrhosis.
The presence of complications aggravate the course of the disease and lead to earlier death. With cirrhosis, patients are at risk of bacterial peritonitis and bleeding from the veins of the esophagus - these complications often result in death. Life expectancy after bacterial peritonitis is reduced because it is poorly treated, prone to recurrence, and often accompanied by renal failure .
Mortality with peritonitis against the background of cirrhosis approaches 80%. Ascites is also a significant complication of cirrhosis, which develops in a third of patients within 5 years from diagnosis. Its development is considered an unfavorable sign, since it indicates the progression of cirrhosis and in half of the patients it ends in death within one year. Hepatorenal syndrome is another complication of cirrhosis that affects patient survival. With this complication, severe acute renal failure develops.
Classification varieties
Alcoholic hepatitis has many different course options. It is important for doctors to consider a number of main characteristics when choosing treatment tactics.
On this basis, they distinguish 2 main types along the flow:
- Persistent. This form is characterized by a stable character and reversible development, provided that a sober lifestyle is maintained.
- Progressive. This process is characterized by a rapid increase in symptoms, cell destruction and organ damage (fine-focal necrosis with transition to cirrhotic changes).
Stages of the disease:
- Easy.
- Average.
- Heavy.
The disease has phases:
- Acute – more pronounced and fast-flowing.
- Chronic, characterized by a sluggish course with periodic exacerbations.
List of sources
- Alcohol disease. Damage to internal organs / Ed. V. S. Moiseeva. – 2nd ed., revised and expanded – M.: GEOTAR-Media, 2014. – 480 p.
- Burnevich, E. Z. Hepatic encephalopathy in liver cirrhosis / E. Z. Burnevich, M. S. Krasnova // Hepatological forum. – 2008. – No. 2. – P. 19–24.
- Ivashkin V. T., Mayevskaya M. V. Alcohol-viral liver diseases. M.: Litterra, 2007. 160 p.
- Maev I.V. Alcoholic liver disease / I.V. Maev, D.T. Abdurakhmanov, D.T. Dicheva // Clinical hepatology. – 2012. – No. 2. – P. 33.
- Mayevskaya, M. V. Algorithm for the management of patients with alcoholic liver disease / M. V. Mayevskaya, M. A. Morozova, V. T. Ivashkin // Russian Journal of Gastroenterology, Hepatology, Coloproctology. – 2011. – T. 21, No. 1. – P. 4–10.