Sign up
Price
Our doctors
- How do you get Hepatitis A?
- What are the symptoms of Hepatitis A?
- How is hepatitis A transmitted?
- Stages of Botkin's disease
- How to treat hepatitis A in a child
- How to treat hepatitis A in an adult
- How to treat chronic hepatitis A
- How to determine the presence of Botkin's disease
- What can you eat if you have hepatitis A?
- How to avoid getting hepatitis A
- Who to contact with hepatitis A
Hepatitis A or Botkin's disease is a medical term for a condition of acute damage to liver cells. The disease is caused by the virus of the same name (HAV) and is considered relatively safe for human life (compared to other types of hepatitis). The disease does not enter a protracted (chronic) stage; treatment of hepatitis A is quite productive, which leads to stable remission and subsequent complete cure.
TREATMENT OF HEPATITIS A IS AVAILABLE IN BRANCHES:
Treatment of hepatitis A in the Primorsky region
Address: St. Petersburg , Primorsky district, st. Repisheva, 13
Treatment of hepatitis A in the Petrograd region
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
Treatment of hepatitis A in Vsevolozhsk
Address: Vsevolozhsk , Oktyabrsky Prospekt, 96 A
The main symptom of hepatitis A is yellowing of the skin, which is why the disease is popularly called “jaundice.”
Vaccination
Vaccination against hepatitis A in Russia is not included in the compulsory vaccination calendar, although in other countries it is actively practiced and is mandatory. The Havrix 720 vaccine from the Belgian manufacturer has proven itself well. It is a suspended virus inactivated by formaldehyde.
Vaccination is carried out in advance: approximately 10–14 days before potential contact with the virus carrier. It is advisable to get vaccinated before going to a children's camp in another country where frequent outbreaks of Botkin's disease are recorded.
Administration of the vaccine is justified after direct contact between a person and an infected person. Deadline: first week after communication. Children tolerate the vaccine quite well. In rare cases, a slight deterioration in general health may occur. This is considered an acceptable physiological norm.
The drug is administered twice with an interval of 6–12 months, which provides stable immunity to the disease for at least 6 years. The prognosis for viral hepatitis A is favorable. The disease is characterized by a successful recovery 3–6 months after infection. Virus carriage and the transition of the disease to a chronic form are atypical.
Causes of hepatitis A (Botkin's disease)
“Disease of dirty hands” is exactly the definition given by doctors around the world to this condition. Hepatitis A occurs only through contact with a sick person. The virus excreted in feces during the incubation period of the disease is most active. Hepatitis of the icteric or erased form is often completely asymptomatic; the person does not understand that he is sick, being a source of infection for those around him and random people who come into contact with the patient’s waste products. People do not see a doctor for a long time, which aggravates the course of the disease and complicates the treatment of hepatitis A. Mortality from this condition is observed in only 0.5% of situations.
In 40% of cases, the hepatitis A virus causes the development of other hepatitis.
Preventive recommendations
To avoid Botkin's disease or reduce the risk of developing it, it is recommended to adhere to the following tips:
- wash your hands before eating and after visiting public places;
- observe precautions when living with a patient with hepatitis A in the same area;
- drink water only from proven sources;
- have one sexual partner or use barrier protection (condoms) during casual intimacy;
- follow food preparation technology without reducing the time of exposure to high temperatures;
Hepatitis A is a disease with a favorable prognosis, but treatment should not be neglected. Thanks to timely diagnosis and therapeutic measures, it is possible to reduce the area of liver damage and quickly restore its functioning.
Symptoms of Hepatitis A (Botkin's Disease)
You can find out about the presence of hepatitis in the body by the following signs:
- a sharp increase in body temperature (38.5-39°C);
- the appearance of signs of intoxication of the body, such as dizziness, nausea, severe weakness, a feeling of aching in the joints, bones, muscles;
- atypical belching, vomiting for no reason;
- feeling of heaviness under the ribs on the right side;
- diarrhea or constipation;
- pain in the abdominal area;
- loss of appetite;
- general malaise and severe weakness;
- Sometimes there is a sore throat and pain when swallowing.
Together, these symptoms indicate hepatitis disease and require immediate initiation of therapy. Treatment of hepatitis A often begins only after the onset of severe jaundice: yellowing of the sclera and skin, darkening of urine and sharp lightening of stool - usually this occurs on days 3-5 of the disease.
The incubation period for hepatitis ranges from 14 to 42 days.
How to protect yourself from hepatitis B?
The only means of protection is vaccination against hepatitis B, which is currently administered to all newborn children and adolescents. Adults with risk factors for infection should also be vaccinated. The hepatitis B vaccine is one of the safest vaccines in the world. Three-time administration of the vaccine according to a special scheme leads to the formation of specific antibodies that prevent the development of hepatitis B disease in 98% of those vaccinated. Immunity lasts for at least 8-10 years, but often remains for life.
Routes of transmission of hepatitis A (Botkin's disease)
The main routes of transmission of hepatitis A are:
- water - when sewage gets into the water supply network or when swimming in lakes and reservoirs in the warm season;
- food – poorly washed fruits and vegetables, dirty hands;
- household items - toys, dishes, linen, etc.;
- sexually - infection with hepatitis A is transmitted in this way extremely rarely, mainly among homosexuals;
- through blood - also in rare cases (situations were noticed among drug addicts and in recipients who received blood from a carrier of the hepatitis virus).
This type of hepatitis A often occurs in the summer, when it is warm outside, people begin to eat more food outside the home and appear in public places more often. Children who are not familiar with the rules of personal hygiene suffer more from the disease. A huge percentage of patients are observed in underdeveloped countries of the world, where there are significant environmental problems.
Causes
The disease is of infectious origin. It is caused by a virus that, upon entering the body, affects the liver and leads to the death of hepatocytes. Infection can occur:
while swimming in a polluted body of water and swallowing water;- when consuming contaminated products;
- when using an infected needle;
- during intimacy (more typical for homosexuals);
- when drinking poorly purified water;
- when using household items (dishes, towels) together with the patient. To avoid the spread of infection, the latter must be isolated throughout the jaundice. The dangerous period is the end of the incubation period and the height of pathology;
- when consuming infected marine life (shellfish).
The risk of infection increases when traveling to hot countries, as well as when hygiene rules are not followed.
The virus is an RNA pathogen and has good resistance to unfavorable conditions.
Stages of Botkin's disease
Hepatitis A in stage 1 is invisible, since the patient does not even understand that he is sick. The duration of the period is 14-42 days (depending on the person’s immunity and aggravating factors, the average is 28 days). At this time, treatment for hepatitis A is not carried out, since the disease is asymptomatic and does not manifest itself in any way.
At the next stage, which lasts from the moment the disease is detected to 54 days, the first symptoms appear:
- general weakness, deterioration of health, fatigue;
- pain in muscles and joints;
- pain in the right side, a feeling of tightness under the ribs in the liver area;
- liver enlargement;
- loss of appetite, dyspeptic disorders;
- itching of the skin.
In children, all these symptoms may be mild or completely absent.
At the third stage, hepatitis is complicated by infection with the HAV virus with characteristic symptoms:
- yellowing of the skin and sclera (“jaundice”);
- discoloration of stool;
- brown urine.
This stage occurs from days 54 to 90. At the first sign of yellowing, treatment for hepatitis A should be started immediately.
Symptoms of viral hepatitis
The duration of the incubation period is three to four weeks, after which the first signs of hepatitis A appear. An acute onset is typical for the disease. Pathology passes through several successive periods:
- pre-icteric or prodromal – can occur in febrile, dyspeptic and asthenovegetative forms;
- icteric;
- convalescence.
Symptoms of the disease depend on the severity of the disease
Symptoms of a febrile period are as follows:
- a sharp increase in body temperature;
- signs of intoxication of the body appear - general weakness, muscle pain and headaches;
- dry cough;
- runny nose;
- redness of the throat.
In some cases, dyspeptic symptoms are added - belching, attacks of nausea, loss of appetite. For the dyspeptic variant, the signs will be somewhat different - catarrhal symptoms and intoxication are slightly expressed. The main complaints are:
- indigestion;
- attacks of nausea ending in vomiting;
- bitter taste in the mouth;
- belching;
- violation of defecation - constipation replacing diarrhea.
A minor pain syndrome in the area of the right hypochondrium with spread to the epigastric area cannot be ruled out.
The pre-icteric period, which takes place in an asthenovegetative format, does not have specific symptoms. The complaints are standard: apathetic state, general weakness, sleep disorders - problems falling asleep. In rare cases, the prodromal period is asymptomatic and the disease immediately begins with jaundice.
Why does my liver hurt after eating?
The duration of the pre-icteric period is 2–10 days, but most often it is a week. The transition to the next phase of hepatitis A occurs gradually. During the icteric period, the symptoms of hepatitis A in adults change. Typical for him are: complete disappearance of signs of intoxication, normalization of body temperature, improvement of general well-being.
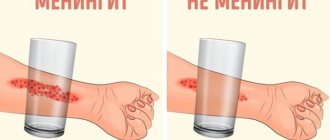
Symptoms of dyspepsia persist and even intensify. The formation of jaundice is slow. Initially, the patient experiences a change in the color of the urine: it becomes darker. Then the sclera of the eyes become yellowish. Then the mucous membranes of the mouth and soft palate turn yellow. The last thing to change is the color of the skin: it becomes an intense yellow-saffron hue.
Significant enlargement of the liver and spleen indicates a severe course of the disease
Severe hepatitis A is characterized by the following symptoms:
- the formation of petechiae, precise hemorrhages on the mucous membranes and surface of the skin;
- formation of a characteristic yellowish coating on the surface of the tongue and teeth;
- enlarged liver and spleen;
- slight pain upon palpation;
- bradycardia;
- decrease in blood pressure;
- discoloration of stool.
The duration of the icteric period is no more than a month. Most often it is limited to 2 weeks. This is followed by a period of convalescence (recovery). The condition returns to normal, the signs of jaundice disappear. The phase takes 3–6 months.
In most diagnosed cases, hepatitis A is mild or moderate. Severe course is rare. The patient, after complete recovery, is not a virus carrier.
Treatment of hepatitis A (Botkin's disease) in children
Therapeutic activities for children of different ages are carried out taking into account the stage and neglect of the process. Usually it is necessary to place the child in a hospital, where hepatitis A will be treated in accordance with the norms and rules of SanPiN. This prevents the spread of infection and cuts off routes of infection. Each child is housed separately in the hospital to prevent cross-transmission of the virus to each other. This greatly facilitates the process of treating hepatitis A in children, especially younger ones.
Therapy includes strict bed rest during the acute period. This treatment of Botkin's disease lasts until the color of urine normalizes and laboratory blood tests improve.
To alleviate the condition of intoxication, treatment of viral hepatitis A with detoxification agents is prescribed: saline solution and glucose solution intravenously. Patients take sorbents internally: activated carbon, Enterosgel, Filtrum, etc.
Hormonal therapy is not usually used in pediatric therapy, but is relevant for malignant progression and exacerbation of the process. If children show severe damage to liver cells (which can be seen if they are tested for hepatitis A and monitor the increase in enzyme levels by 5 or more times), the doctor additionally prescribes antiviral drugs. Usually “Interferon”, “Viferon”, “Raferon-A” and others are used.
Hepatitis A in children is often treated with the help of immunomodulators: Decaris, Cycloferon, Tactivin, etc.
To support the patient’s liver, hepatoprotectors are used: “Essentiale N”, “Essentiale Forte”. Thanks to the phospholipids they contain, treatment of hepatitis A proceeds faster due to the restoration of liver cells. Herbal preparations will also help in treating the disease: “Karsil”. "LIV 52", "Legalon" and others.
To speed up the restoration of the body's defenses, vitamin complexes and restoratives are taken. Some children are prescribed choleretic drugs: “Cholenzim”, “Hofitol”, etc.
Is it necessary to follow a diet for patients with chronic hepatitis B?
No special diet is required for chronic viral hepatitis, however, you should avoid drinking alcohol even in small doses, since the combined effect of alcohol and the virus on the liver significantly increases the risk of developing cirrhosis and liver cancer. If you are overweight, you should limit your intake of fats and high-calorie foods, since fat deposition in the liver accelerates the development of cirrhosis. Factors that reduce immunity, in particular sun exposure, should be avoided, that is, you should not use a solarium or sunbathe on the beach. It is advisable to quit smoking. You can continue to exercise. Swimming and hardening procedures that support the state of your immunity are useful.
Treatment of hepatitis A (Botkin's disease) in adults
After identifying the disease, it is necessary to limit communication with others, ideally to go to the hospital for the entire acute period. Treatment of hepatitis A in adults is carried out practically according to the same scheme as in children. This is the organization of bed rest, which is highly not recommended to be violated, the complete cessation of open communication with others, and the implementation of all doctor’s recommendations.
Timely seeking help from a doctor and taking a blood test for hepatitis A can determine the presence of concomitant diseases (including infection with other hepatitis viruses). If the immune system is strong and the body’s protective functions work as expected, special treatment for hepatitis A in adults is not necessary. In cases where the disease has seriously affected the patient’s well-being, the doctor prescribes the following medications:
- enterosorbents for detoxification and removal of toxic substances from the body - they allow you to relieve liver cells from additional stress (in this case, hepatitis A should be treated with the help of Ringer-Locke solutions, glucose, Atoxil and others);
- hepatoprotectors - the drugs include Hepatosan, Legalon, Ursonan, etc.;
- vitamins – B vitamins are especially important;
- medications to relieve symptoms.
A drug called ursodeoxycholic acid in the form of pharmaceuticals “Ursodex”, “Urosan”, etc. will help improve liver function.
Symptomatic treatment of hepatitis A is prescribed separately in each case. If the patient is bothered by nausea and vomiting, he is prescribed antiemetics, and for pain, painkillers. To improve general well-being, vitamin preparations and immunomodulatory complexes are used. If hepatic encephalopathy develops, corticosteroids are prescribed.
Treatment of Botkin's disease has a favorable prognosis, liver functionality is usually completely restored.
Why is jaundice dangerous?
Complications of Botkin's disease for newborns are extremely severe, and therefore require immediate hospitalization and intensive care. In older age, the disease occurs in a milder form, but the risk of undesirable consequences is still present. They are expressed:
- inflammation of the pancreas;
- joint damage (arthritis);
- inflammation of the mucous membrane of the digestive tract;
- vasculitis;
- renal dysfunction, which is expressed by nephrotic syndrome;
- inflammation of the organs of the hepatobiliary system.
Sometimes secondary infection, development of liver failure and encephalopathy are observed.
Consequences of jaundice in men
There is an opinion that Botkin's disease can cause infertility, but convincing evidence of this theory has not yet been provided. The pathogenesis of the development of this complication has not yet been established, therefore, in case of unsuccessful attempts to conceive, the cause should not be sought in viral liver damage.
Jaundice is just as dangerous for men as it is for women. The severity of complications depends on concomitant diseases and lifestyle.
Given the prevalence of alcoholism among the stronger sex, Botkin's disease can quickly lead to liver failure. The fact is that the breakdown products of alcohol have a toxic effect on hepatocytes, which is why they gradually die. Viral infection due to alcoholism can lead to decompensation of the gland, up to complete failure. Note that cirrhosis develops faster in men.
The stronger sex is less inclined to follow a dietary diet, as a result of which the affected hepatocytes in Botkin's disease experience additional stress (fatty, spicy foods). This can result in liver failure due to irreversible cell death.
Consequences of Botkin's disease in women
According to statistics, the weaker sex more often suffers from cholecystitis, cholangitis and bile duct dyskinesia. From this it follows that hepatitis A can provoke an exacerbation of chronic diseases of the biliary tract.
On the other hand, women are more susceptible to hormonal fluctuations. They can be caused by endocrine pathology, taking oral contraceptives, stress and pregnancy. All this affects metabolic processes, resulting in an increased risk of obesity and the progression of related diseases.
Treatment of chronic hepatitis A (Botkin's disease)
Hepatitis A is completely curable with well-designed therapy and does not progress to a long-term (chronic) stage. There may be a complication caused by a global disruption of the liver and the inability to establish its normal functioning for a long period (from 1-2 years to decades) after the illness. Treatment of chronic hepatitis A in this case is symptomatic and is aimed at restoring damaged liver cells, improving the functioning of the gallbladder, monitoring the patient’s general well-being and diet, especially in the acute period.
Prevention
There is no specific prevention of infection. General measures to prevent infection are:
- high-quality purification of drinking water supply sources;
- compliance with sanitary and hygienic requirements;
- epidemiological control at enterprises involved in the production, storage and transportation of food products.
In the event of an outbreak of hepatitis A in organized groups, anti-epidemic quarantine measures are mandatory. Sick people are isolated for a period of 2 weeks. Patients cease to pose a danger to others after the onset of the icteric period.
They are allowed to work and study only after clinical recovery, i.e. when test results return to normal. Persons who have had direct contact with infected people need to be monitored for 35 days. Quarantine is declared in kindergartens and schools for this period. All surfaces in the room are thoroughly sanitized.
It is easier to prevent the development of pathology than to engage in long-term treatment
Diagnosis of hepatitis A
Before starting treatment for hepatitis A, it is necessary to diagnose the disease and determine at what stage of development it is. The disease is diagnosed by an infectious disease doctor who will suggest testing for hepatitis A. In most cases, diagnosis is carried out in several stages:
- interviewing or collecting anamnesis from the patient or his relatives (for children);
- conducting a blood test for hepatitis A (detection of virus markers);
- biochemical blood and urine tests;
- examination of the abdominal cavity using ultrasound.
After this, treatment for hepatitis A is prescribed and monitoring of the patient during the recovery period is organized.
Characteristics of the pathogen
The hepatitis A virus belongs to the Hepatovirus group, the genome is RNA. Stable outside the wearer's body. At room temperature it dies within a few weeks, at +4 it can survive for several months, at -20 it remains active for years.
The pathogen is killed by boiling after 5 minutes and may remain active for a short time in chlorinated tap water. It is transmitted by the fecal-oral route, mainly through food and water. Infection through contact and household contact cannot be ruled out: transmission occurs through the use of shared utensils or household items.
Diet for hepatitis A
As with some other liver diseases, treatment of hepatitis A is impossible without following a strict diet. Without this, the weakened liver will not cope with the load placed on it and will not be able to process even those familiar foods that were previously in the diet constantly. To make it easier to treat hepatitis A, and the disease went away faster, Soviet-era specialists developed a special diet, which received the official name “Table No. 5.” Her recommendations are still followed today, despite the abundance of goods on store shelves. It is better to avoid modern food products of imported and domestic production. This is easily explained: new generation products often contain preservatives, dyes, and food additives that have a detrimental effect on even perfectly healthy liver cells.
Table No. 5: which foods should be completely excluded?
If you have hepatitis A, you should completely avoid alcohol. The use of tobacco and narcotic, potent and certain medications also needs to be stopped. During treatment for viral hepatitis A, you should not eat fried, smoked, salty or fatty foods. Pickled foods, fatty meats, and any fast-cooking foods are removed from the diet.
Products such as chips, crackers, instant foods, carbonated water and other drinks with dyes are strictly prohibited during the period of treatment for hepatitis A and for at least six months after recovery.
What can you eat?
- Meat or fish (it is better to choose low-fat varieties), steamed or boiled;
- dairy and fermented milk products: kefir, 10-15% sour cream, yogurt without additives, cottage cheese;
- stewed or fresh vegetables;
- lean soups, sometimes borscht is allowed;
- egg whites (better cooked in a steam omelet);
- homemade crackers without salt or other flavor enhancers;
- yesterday's bread;
- weak black, green or herbal tea (with or without milk), compotes, jelly and homemade juices (from sweet fruits and berries), chamomile or rose hip decoction, still mineral water.
It is impossible to treat hepatitis A without following a diet; this can lead not only to disruption of the liver, but also to its complete stop, which will lead to disastrous consequences for the patient.
Kinds
The following forms of viral hepatitis A are known:
- icteric;
- with erased jaundice;
- anicteric.
A separate subclinical (inapparent) form is distinguished, which is diagnosed only on the basis of laboratory test results.
The course of the disease can be acute, protracted, subacute and chronic (extremely rare). According to the severity of clinical manifestations, acute infectious hepatitis can be mild, moderate and severe.
Prevention of hepatitis A (Botkin's disease)
It is always easier to prevent a disease and prevent it from developing than to treat its consequences for the body. To avoid infection with hepatitis, doctors have compiled a list of recommendations that absolutely all people should adhere to, regardless of their body characteristics, status, position in society, place of stay, or age.
It is necessary to remember these rules of conduct:
- wash food thoroughly before giving it to children or eating it - vegetables, fruits and berries should be soaked in water for several minutes and then washed well with your hands or a sponge;
- You should always follow simple rules of personal hygiene not only in public places, but also at home, at work - you must wash your hands with soap after returning from the street, visiting the restroom and before eating (even if it comes to a snack);
- never use tap water for food, even if it is a personal well with seemingly absolutely clean water without chemicals (there may be pathogens that have entered the groundwater);
- avoid swimming in bodies of water with stagnant water (especially in the hot season and in unfamiliar areas);
- never drink raw water from unknown sources;
- vaccinate;
- stop eating junk food and enrich your daily diet with foods containing fiber, natural vitamins and microelements;
- forget about bad habits: avoid the use of alcohol and drugs, tobacco products;
- do not self-medicate: all medications should be prescribed by a doctor, and if it is necessary to carry out continuous therapy with a group of drugs, you should select those that have the most gentle effect on the liver (you can discuss this issue with your doctor or by studying the instructions for the medications);
- Before going to another country on a tourist or work visit, you need to stock up on personal hygiene products: wet and dry wipes, special cleaning compounds for disinfecting the surface of your hands, a container for water (at least 0.5-1 liter). This is especially true for countries with an unfavorable epidemiological situation, where finding water for washing hands is extremely problematic, but you still have to eat;
- Before traveling to other regions and countries, you should check the epidemiological situation. If it is unfavorable, you should postpone your trip (if possible).
All these recommendations will allow you to protect yourself from becoming infected with viral hepatitis A.
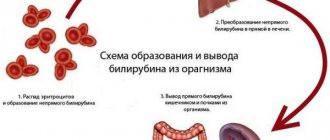
Diagnosis of pathology
The diagnosis is made based on characteristic symptoms, as well as physical examinations and laboratory tests. Patients must donate blood. Biochemistry shows the following changes:
- increased bilirubin levels (bilirubinemia);
- increase in the activity of liver enzymes - AST, ALT;
- decrease in prothrombin index;
- decrease in albumin levels;
- decrease in thymol and increase in sublimate test.
Changes are also recorded in the general blood test. There is an increase in the erythrocyte sedimentation rate, as well as leukopenia and lymphocytosis. There is also a specific diagnosis based on the detection of antibodies. The ELISA and RIA techniques are used. A more accurate method is serodiagnosis, which allows one to detect viral RNA in the blood.
What specialists should I contact if I have hepatitis A?
At the slightest suspicion of illness, you need to stop or limit contact with others and consult a doctor as soon as possible. To clarify the diagnosis (in the initial stages), you need to consult a therapist. When symptoms become more pronounced, you should contact a hepatologist, gastroenterologist, or infectious disease specialist. These specialists will help cure hepatitis A, eliminate its symptoms, and avoid unpleasant consequences.
This disease cannot be treated independently, because if treated incorrectly, its consequences can be disastrous for a person.
Diagnostics
Diagnosis of hepatitis A is based on clinical signs of the disease: liver enlargement, jaundice and other symptoms. The doctor also takes into account epidemiological factors, that is, how the infection is contracted (drinking unboiled water, products of unknown purity, and so on).
Laboratory tests are crucial. Disease-specific tests:
- polymerase chain reaction to detect viral genetic material;
- enzyme immunoassay for detecting antibodies to pathogens of the IgM class.
If only IgG antibodies are detected in the body, this indicates a previous disease or immunity to it. The chronic form of the disease does not occur, but there are cases of healthy virus carriers.
Nonspecific laboratory signs of the disease in women and other groups of patients are necessary to assess the severity of the infectious process and the effectiveness of prescribed drugs:
- ALT and AST;
- bilirubin and its fractions (direct, indirect);
- serum protein level, fibrinogen.
Ultrasound is used to determine the size of the liver.
The appointment is conducted by doctors:
Children's specialists
Consults online
Greshnyakova Vera Alexandrovna
Infectious disease specialist, hepatologist, gastroenterologist, candidate of medical sciences, first category
Kizhlo Lyudmila Borisovna
Infectious disease specialist, hepatologist, gastroenterologist, candidate of medical sciences, highest category
Nozhkin Mikhail Sergeevich
Infectious disease specialist, hepatologist
Revchuk Ekaterina Vladimirovna
Infectious disease specialist, hepatologist, gastroenterologist
Rovny Viktor Borisovich
Infectious disease specialist, hepatologist, gastroenterologist, candidate of medical sciences, highest category
Chernykh Mikhail Dmitrievich
Infectious disease specialist, hepatologist, gastroenterologist, candidate of medical sciences, highest category
Viral hepatitis A: modern clinical features, diagnosis and prevention
Viral hepatitis A (HA) has traditionally been considered primarily a childhood, mild, benign, self-limiting disease and therefore has not attracted much attention from either clinicians or scientists. However, in recent years, new data has emerged, prompting a reconsideration of some provisions that previously seemed unshakable. In particular, in Russia the incidence of GA in adults exceeds that in children; the disease does not always proceed “smoothly”; Russian doctors know about the possibility of death from GA not only from foreign literature, but also from their own experience.
HA is one of the most common human diseases on earth; about 1.4 million cases are registered annually in the world [5]. And in Russia, the incidence of GA remains high to this day; in the general structure of acute viral hepatitis it accounts for more than 50%. In terms of economic costs, HA ranks 5th in Russia among all registered infections. It is not surprising that in recent years GA has attracted the attention of both practicing doctors of various specialties (infectious disease specialists, pediatricians, gastroenterologists, therapists) and representatives of medical science. In June 2010, the All-Russian Scientific and Practical Conference was held in Moscow, at which modern aspects of epidemiology, clinical manifestations, specific laboratory diagnostics and prevention of hepatitis A were summarized [1].
The causative agent of hepatitis A is a virus (HAV, Hepatitis A virus, HAV), first identified by Finestone and co-authors in 1973; is hepatotropic, has a weak cytopathogenic effect on liver cells. HAV is one of the most resistant human viruses to environmental factors; it can survive for a long time in water, food products, wastewater, and on various environmental objects [2, 6].
Epidemiology. HA is a classic anthroponosis; the only source (reservoir) of the infectious agent is humans. The virus is isolated by patients with various forms of the disease, including the most common (especially in children): anicteric and erased, which are usually not diagnosed; accordingly, patients with these forms are not hospitalized, lead an active lifestyle and can infect others. From patients with the icteric form, the virus is excreted in feces most intensively at the end of the incubation and during the pre-icteric periods, i.e., also before recognition of GA. With the appearance of jaundice in most cases, the infectiousness of patients is significantly reduced. It is this feature—the most active release of the virus from the patient’s body before the appearance of jaundice, combined with the high resistance of HAV in the external environment—that causes the widespread spread of hepatitis A. The HA virus is highly infective; only a few viral particles are enough to become infected with hepatitis A [7–9].
GA is a typical intestinal infection with a fecal-oral transmission mechanism. Routes of transmission: water, food and household. Transmission factors, as with all intestinal infections, are various food products (including seafood, frozen vegetables and fruits) that are not heat-treated, as well as water and dirty hands. Large outbreaks of GA are associated with fecal contamination of water bodies or wastewater entering the water supply network. In children's groups, the contact and household route of transmission through dirty hands and various household items is of great importance: toys, dishes, linen, etc. Water and food outbreaks have been repeatedly recorded in Russia (including in Moscow, St. Petersburg, Nizhny Novgorod , Tver region) in 2005–2010. [1].
Human susceptibility to hepatitis A is universal. In regions with widespread distribution of the HA virus (countries of Africa, Southeast Asia, Latin America), most cases of infection occur in young children [8, 11].
In developed countries, the first encounter with the HA virus may occur in adolescence or later. The risk of infection is especially high when traveling to hot countries (tourism, travel) with water shortages, poor sewerage and water supply systems, and low levels of hygiene of the local population. It is no coincidence that HA is called a traveler's disease. The development of mass tourism and visits to regions of the world endemic for GA pose an increased risk of infection for Russians. Mass migration also contributes to the active circulation of HAV in Russia.
In Russia, GA was previously predominantly a childhood infection, but in recent years, due to a number of reasons (declining birth rates, a decrease in the number of children attending preschool institutions, etc.), the incidence of GA has shifted to older age groups.
Immunity after hepatitis A is strong and long-lasting, almost lifelong.
Clinic. The duration of the incubation period ranges from 7 to 50 days, averaging about one month.
The clinical classification of HA provides for the identification of several variants: icteric, anicteric, erased and subclinical (inapparent).
The classic, although not the most common, is the icteric variant of GA, which occurs cyclically, in which the incubation period is followed by the pre-icteric one. The disease usually begins acutely with an increase in body temperature to 38–39 ° C, symptoms of intoxication (headache, dizziness, unexplained weakness, weakness, aches in muscles, bones, joints, etc.) and dyspeptic syndrome (decreased appetite, nausea, bitterness in the mouth). mouth, belching, vomiting, heaviness in the epigastric region and right hypochondrium, delayed or loose stool). At the same time or earlier than dyspeptic symptoms, mild catarrhal symptoms sometimes appear in the upper respiratory tract (sore throat, slight pain when swallowing, etc.), which is often the basis for the erroneous diagnosis of “ARD” [9, 10]. Children may have intense abdominal pain, simulating acute appendicitis, biliary colic; This is not typical for adults.
At the end of the pre-icteric period, which most often lasts from three to seven days (with fluctuations from two to 14), the urine becomes dark yellow and the feces become lightened. However, these symptoms, which are very important for the timely diagnosis of hepatitis A, are not always noticed by patients.
In children, already in the pre-icteric period, liver enlargement can be detected.
In the blood serum of patients with HA in the pre-icteric period, the activity of aminotransferases - ALT and AST - increases significantly (10 times or more), and the content of urobilin in the urine increases. After 3–5 days from the onset of the disease, body temperature usually normalizes, but icterus appears—first in the sclera, then in the skin. The icteric period begins. However, in 2–5% of cases, the symptoms of the pre-icteric period described above are not detected, and then GA begins with a change in the color of stool and icteric staining of the sclera.
Usually, with the appearance of jaundice, the patient’s well-being begins to improve quite quickly, body temperature normalizes, and the symptoms of the pre-jaundice period disappear. Weakness and loss of appetite persist longer than others. In recent years, often in patients with HA, against the background of emerging jaundice, fever continues and symptoms of intoxication increase; This usually happens in patients with chronic alcohol intoxication or drug addiction.
Jaundice with GA increases quickly, usually reaching a maximum in 3–5 days, in the next 5–10 days it remains at the same level, and then its intensity decreases. On average, the duration of the icteric period is about two weeks. Upon examination, an enlarged liver is revealed, which is compacted, with a rounded edge, and is sensitive to palpation; An enlarged spleen is observed in 10–15% of cases, more often in children. At the height of jaundice, bradycardia is characteristic.
As the intensity of jaundice decreases, the color of stool and urine normalizes, and the size of the liver gradually decreases.
In the icteric period, pronounced hyperenzymemia persists with a predominant increase in ALT activity compared to AST (accordingly, the de Ritis coefficient is always less than 1). Hyperbilirubinemia is usually moderate and short-lived, caused predominantly by the bound fraction of bilirubin. A significant increase in the thymol test is characteristic.
The hemogram shows normocytosis or leukopenia, relative lymphocytosis; ESR is normal.
The period of convalescence is usually characterized by a fairly rapid disappearance of clinical and biochemical signs of viral hepatitis, in particular hyperbilirubinemia. Later, ALT and AST activity levels return to normal; An increase in the thymol test can persist for a long time, for several months. The state of health of those who have recovered from GA is usually satisfactory; fatigue after physical activity, discomfort in the abdomen after eating are possible, and sometimes a slight enlargement of the liver persists. The duration of this period in most cases does not exceed three months.
In some cases, the period of convalescence can last up to 6–8 months or more, exacerbations (enzymatic or clinical) are possible, as well as (in 3–20%) relapses. The latter usually occur in people 20–40 years old 1–3 months after the main wave and, as a rule, are milder than the first wave of the disease. However, relapses with acute renal failure and death have been described.
The icteric variant of HA described above most often occurs in mild or moderate forms. A severe form of HA occurs in no more than 1% of patients, mainly in people over 40 years of age, in patients with chronic alcohol intoxication or drug addiction, chronic viral hepatitis of other etiologies (B, D, C). Among children, a severe form of HA is recorded during puberty, as well as against the background of obesity and a burdened allergic history.
The fulminant form of HA with the development of acute liver failure and encephalopathy is rare, occurring in 0.1–1% of all cases.
Sometimes, especially in older age groups, HA is accompanied by a pronounced cholestatic component, while the icteric period is extended to several months, the intensity of jaundice is great, the disease is accompanied by itching of the skin, and the activity of alkaline phosphatase in the blood serum significantly increases [3, 6].
Cholestasis syndrome is also characteristic of HA with an autoimmune component, combined in this case with other systemic immune disorders, such as vasculitis, nephritis, polyarthralgia, purpura, acute hemolytic anemia, fever, etc. Cryoglobulins and rheumatoid factor appear in the blood serum, and CEC levels are increased , the gamma globulin fraction of the protein spectrum, autoantibodies can be detected (in particular, to smooth muscle).
The anicteric variant is characterized by the same clinical and laboratory signs as the icteric variant, however, the absence of one of the most noticeable manifestations of hepatitis - jaundice and, accordingly, hyperbilirubinemia, makes diagnosis difficult. The clinical symptoms of the anicteric variant correspond to the manifestations of the pre-icteric period of the classic icteric variant. A short-term increase in body temperature, dyspeptic symptoms, weakness, catarrhal syndrome, etc. are possible for 3–5 days. The liver enlarges and becomes slightly painful on palpation, and the urine may darken. Hyperfermentemia is detected, ALT and AST levels increase almost as significantly as in the icteric form, and the thymol test indicator increases.
The anicteric variant develops tens of times more often than the icteric variant, but is rarely recorded, usually only during a targeted examination of children's groups and in epidemic foci of GA. The younger the child, the greater the likelihood of the anicteric variant of HA; In adolescents and adults, jaundice predominates.
The erased variant is manifested by minimal and quickly passing clinical symptoms (including jaundice) in combination with hyperfermentemia and an increased thymol test.
In the subclinical (inapparent) variant, in contrast to the anicteric and erased variant, the well-being of the sick is not disturbed, the liver does not enlarge, jaundice does not appear, but the activity levels of ALT and AST are increased, and specific markers of GA are determined in the blood serum.
In recent years, Russia has seen an increase in the incidence of not only hepatitis A, but also viral hepatitis of other etiologies (primarily B and C), as well as HIV infection. The consequence is an increase in cases of hepatitis of mixed etiology, differing in course and outcome from monoinfection caused by HAV. In particular, in one of the first works devoted to the characteristics of HA in people with viral hepatitis C (HCV infection), it was noted that wave-like hyperfermentemia in convalescents of HA with HCV is observed in 68% of cases within 6 months and in 41% up to a year. On the other hand, during co-infection with HAV and HCV, a competitive interaction of viruses was revealed, which leads to a temporary suppression of HCV replication.
HA against the background of chronic infection with the hepatitis B virus is characterized by a prolonged course and persistent residual effects. In HIV-infected patients, the acute period of HA does not have any remarkable features, but there has been a report of long-term persistence of HAV RNA in the blood and hyperfermentemia for more than three months in an HIV-seropositive patient.
HA and chronic alcohol intoxication have a mutually aggravating effect. With this combination, fever can last more than two weeks against the background of jaundice, often a combination of clinical signs of HA and alcohol withdrawal syndrome, up to meta-alcohol psychosis; Decompensation of alcoholic liver disease often develops, and death is possible, which is confirmed by our observations.
Complications for hepatitis A are not typical; the most severe of them, hepatic coma, is extremely rare. Among possible complications, one should keep in mind functional and inflammatory diseases of the biliary tract. Acute renal failure and hemolytic-uremic syndrome associated with HAV infection have also been described. In our clinic, we observed an 18-year-old patient whose HA was complicated by massive intravascular hemolysis, acute renal failure, and disseminated intravascular coagulation syndrome; death occurred, the immediate cause of which was massive pulmonary hemorrhage. Individuals with impaired T-suppressor function during and/or after HA may develop type 1 autoimmune hepatitis.
A lethal outcome from HA is extremely rare, but is nevertheless possible in older age groups and patients with previous liver diseases (alcoholic liver disease, chronic hepatitis of various etiologies). The cause of death may be cerebral edema in patients with acute liver failure.
Thus, the main features of modern hepatitis A are:
- an increase in the proportion of sick adults, including older age groups;
- frequent combination with chronic alcohol intoxication, chronic hepatitis B and C, HIV infection;
- the presence of cholestatic syndrome and an autoimmune component;
- more frequent development of moderate, severe and fulminant forms;
- tendency to a protracted course with exacerbations and relapses.
Diagnostics. The diagnosis of hepatitis A is established taking into account clinical, epidemiological and laboratory data. The basis for the assumption of GA are:
- acute onset of the disease with high body temperature, dyspeptic and asthenovegetative phenomena;
- short pre-icteric period;
- liver enlargement;
- improvement of well-being, normalization of temperature when jaundice appears;
- hyperenzymemia (ALT, AST) with a de Ritis coefficient less than 1;
- hyperbilirubinemia (mainly due to the bound fraction);
- high thymol test;
- an indication of contact with a patient(s) with jaundice 7–50 days before illness or consumption of raw water from random sources, unwashed vegetables and fruits, etc.; cases of GA in the community, the area where the patient was located during the period corresponding to the incubation period, travel to the countries of Africa, Asia, Latin America.
A specific marker of HA are antibodies (immunoglobulins) to the hepatitis A virus class M (anti-HAV or anti-HAV IgM), detected by enzyme-linked immunosorbent assay (ELISA) in the blood serum from the first days of the disease and then for 3-6 months. These antibodies (“early”) are produced in all patients with GA, regardless of the clinical variant and form of severity; their detection is an early and reliable diagnostic test that allows not only to confirm the clinical diagnosis of GA, but also to identify its anicteric, erased and subclinical variants. After 6–8 months, anti-HAV IgM is undetectable. The synthesis of specific “late” anti-HAV (anti-HAV) IgG begins from the 2-3rd week of the disease, their titer increases slowly and reaches a maximum after 4-6 months, then decreases, but for several decades (possibly lifelong) they detected by ELISA. Anti-HAV (anti-HAV) IgG is detected in a proportion of adults, which is considered evidence of previous HAV and indicates immunity to this infection. Anti-HAV IgG is also produced in those vaccinated against HA.
In recent years, it has become possible to test HAV RNA using molecular genetic methods (polymerase chain reaction (PCR)). HAV RNA in blood serum can be detected several days before the increase in ALT activity, that is, PCR is a highly specific early method for diagnosing HA, but is rarely used in practice.
Treatment. Patients with mild hepatitis A can be treated at home; the rest are subject to hospitalization and treatment in infectious diseases hospitals or departments. Causal therapy has not been developed, antiviral drugs are not used [4].
In mild cases, they are limited to basic therapy, which includes an appropriate diet and gentle regimen. Fried, smoked, pickled foods, and refractory fats (pork, lamb) are excluded from the diet. Alcohol in any form is strictly prohibited. It is recommended to drink plenty of water (up to 2-3 liters per day) of loosely brewed tea with milk, honey, jam, as well as rosehip decoction, freshly prepared fruit and berry juices, compotes, and alkaline mineral waters.
For the purpose of detoxification, patients with a moderate form of HA are prescribed enterosorbents (Enterodes, Enterosgel, etc.), and in case of nausea, refusal to drink, intravenous drips of 5% glucose solution, Ringer's solution, etc.; in severe cases, intensive pathogenetic therapy is carried out, including plasmapheresis. In cases with severe cholestatic syndrome, fat-soluble vitamins A and E, enterosorbents, and ursodeoxycholic acid preparations are recommended.
For GA patients with chronic alcohol intoxication, ademetionine is indicated intravenously in the first two weeks at 800–1600 mg daily, then 2–4 tablets per day.
The need for vitamins should be met through natural foods. If this is not possible, multivitamin preparations (Aevit, Ascorutin, Undevit, etc.) are additionally prescribed 3 times a day after meals. It is necessary to monitor daily bowel movements. For constipation, lactulose should be used, the dose of which is selected individually (30–60 ml/day) so that the stool is formed or pasty every day.
All convalescents of HA should be under clinical observation for 3–6 months, depending on their well-being, the speed of normalization of liver size and the dynamics of the results of biochemical studies. If convalescents do not have any clinical and laboratory deviations from normal parameters, they can be removed from the register with a recommendation to be released from heavy physical work and sports. For six months, preventive vaccinations are contraindicated, except (if indicated) tetanus toxoid and rabies vaccine. It is undesirable to carry out planned operations; the prescription of hepatotoxic medications within six months after undergoing GA is contraindicated.
When jaundice and hyperenzymemia (ALT, AST) recur in a convalescent HA patient, re-hospitalization is necessary to distinguish a possible relapse of HA from the manifestation of hepatitis of a different etiology (including autoimmune). For convalescents with a persistent moderate increase in ALT and AST activity, it is advisable to prescribe one of the hepatoprotectors: Phosphogliv 1 capsule 3 times a day, silibinin (Karsila), Essentiale N 1-2 capsules 3 times a day, ademetionine 2-4 tablets a day, ursodeoxycholic acid 15 mg/kg/day.
The prognosis for GA is favorable. In the vast majority of cases, complete recovery occurs within one to three months after discharge from the hospital. Among other outcomes of GA, residual effects are possible in the form of prolonged convalescence (asthenic syndrome, functional disorders of the gastrointestinal tract, a slight increase in the activity of aminotransferases and/or thymol test persist for 3–6 months). In some cases, during the period of convalescence of HA, Gilbert's syndrome first appears. In addition, after undergoing GA, dyskinesia or inflammation of the biliary tract may be detected.
In any case, hepatitis A, which occurs as a monoinfection, ends with complete recovery, and the formation of chronic hepatitis does not occur.
Prevention of GA, as well as other intestinal infections, includes sanitary and hygienic measures (including personal hygiene, regular hand washing, drinking only boiled water), providing the population with good-quality drinking water and food, and proper disposal of wastewater. Early diagnosis of HA and isolation of sick people even before they develop jaundice can prevent infection of others.
Specific prevention is carried out with inactivated vaccines, both domestic and foreign. In Russia, vaccination against GA is included in the National Calendar of Preventive Vaccinations for epidemic indications. The following are subject to vaccination: children from three years of age living in areas with a high incidence of hepatitis A; medical workers, teachers and staff of preschool institutions; food service workers; workers maintaining water and sewerage facilities; persons traveling to hyperendemic regions and countries, as well as contacts in the focus of hepatitis A. Military contingents stationed in the field are also vaccinated [1].
Vaccination against hepatitis A is also indicated for patients with chronic liver diseases, including asymptomatic carriers of the Australian antigen (HBsAg), patients with chronic hepatitis B and C. The high epidemiological and economic effectiveness of vaccine prevention currently determines it as the most effective means of controlling viral hepatitis A .
Literature
- Current issues of epidemiology and prevention of hepatitis A. Sat. abstracts of the All-Russian Conference, 2010. 44 p.
- Balayan M. S. Hepatitis A: yesterday, today, tomorrow // Medicine for everyone. 1999; 2 (13): 22–25.
- Diseases of the liver and biliary tract: A guide for doctors, edited by V. T. Ivashkin. M.: LLC Publishing House "M-Vesti", 2002; 416 pp.
- Viral hepatitis. Standards of medical care for patients. Clinic, diagnosis, treatment and medical examination of adults and children with viral hepatitis. Methodological manual / On improving medical care for patients with viral hepatitis: Order of the Moscow Health Committee. M., 2000; 98 p.
- Hepatitis A. WHO Fact Sheet No. 328, 2008.
- Infectious diseases: national guidelines. Ed. N. D. Yushchuk, Yu. Ya. Vengerova. M.: GEOTAR-Media, 2009. 1056 p.
- Lectures on infectious diseases. Ed. Academician of the Russian Academy of Medical Sciences N. D. Yushchuk, corresponding member. RAEN Y. I am Vengerova. 3rd ed. M.: Medicine, 2007; 1032 pp.
- Mayer K.-P. Hepatitis and the consequences of hepatitis: Trans. with him. Scientific editor A. A. Sheptulin. M.: Geotar Medicine, 1999. 423 p.
- Guide to Infectious Diseases. Ed. Corresponding member RAMS Yu. V. Lobzin. St. Petersburg: Foliot, 2000. 932 p.
- Sorinson S. N. Viral hepatitis in clinical practice. 2nd ed., revised. and additional St. Petersburg: Teza, 1998; 330 pp.
- Sherlock S., Dooley J. Diseases of the liver and biliary tract: A practical guide.: Trans. from English Ed. Z. G. Aprosina, N. A. Mukhina. M.: Geotar Medicine, 1999. 864 p.
G. N. Karetkina, Candidate of Medical Sciences, Associate Professor
MGMSU, Moscow
Contact information about the author for correspondence
Cost of hepatitis A treatment:
| Services list | Price in rubles | |
| Saint Petersburg | Vsevolozhsk | |
| Initial appointment with a 2nd stage hepatologist | 2100 | — |
| Repeated appointment with a 2nd stage hepatologist | 1900 | — |
| Initial appointment with a hepatologist, leading specialist | 2500 | — |
| Repeated appointment with a hepatologist, leading specialist | 2300 | — |
| Initial appointment with hepatologist Kizhlo L.B./Rovny V.B. | 3000 | 3000 |
| Repeated appointment with hepatologist Kizhlo L.B./Rovny V.B. | 2700 | 2700 |
| Initial appointment with hepatologist M.D. Chernykh | 3300 | — |
| Repeated appointment with hepatologist Chernykh M.D. | 2900 | — |
Complications
Hepatitis A rarely causes complications; usually the disease ends in complete recovery. The most severe complication of Botkin's disease is liver failure. After recovery from hepatitis A, strong immunity usually remains and re-infection is not possible. However, if treatment is not completed and complete recovery does not occur, a second wave of the disease may occur - a relapse. This happens in 15% of people with Botkin's disease and can occur repeatedly.
Liver failure is a rare and potentially life-threatening complication of hepatitis in which the liver may stop functioning normally. The following groups of people are usually affected by it:
- people with weakened immune systems (as a result of a chronic disease such as diabetes or a side effect of certain treatments such as chemotherapy).
- people with existing liver disease such as cirrhosis or hepatitis C (a more severe type of hepatitis);
Some symptoms of liver failure are similar to those of hepatitis A and include jaundice, nausea and vomiting.