Symptoms of meningitis
Signs of meningitis are as follows:
- severe pain in the head,
- temperature, pain in the muscles of the neck,
- hearing loss,
- fainting,
- vomiting and nausea,
- mental problems (paranoia, delusions, excited or apathetic state, increased anxiety),
- convulsive states,
- hives,
- drowsiness.
It all depends on the type of meningitis in adults , so the following stages of the disease can be noted:
- Purulent meningitis . The form is severe, pus appears in the brain capsules. This disease is provoked by bacterial infections, more precisely: staphylococcus, streptococcus, pneumococcus, meningococcus.
- Serous meningitis . The disease is less severe than the first option. At the time of inflammation, no pus appears. This is a kind of viral meningitis. This category includes such types as tuberculosis, influenza, mumps, and syphilitic.
Depending on the course of the disease, the following forms are observed:
- Instant. Symptoms of meningitis in children appear instantly. A person can die in the first 24 hours after infection.
- Spicy. Infectious type meningitis occurs within a couple of days after infection. A person can die instantly. Meningitis symptoms in adults have a bright course.
- Chronic. Symptoms gradually appear and get worse.
Depending on the duration of meningitis and the proliferation of inflammation, there are the following forms:
- Basal. Inflammation occurs in the center of the brain.
- Convexital. Pathological processes concern convex areas of the brain.
- Total. Inflammation affects all parts of the brain.
- Spinal. Inflammation is observed on the surface of the spinal cord.
Depending on the severity, the disease can be mild, moderate or severe.
Meningitis
Encephalitis
Fungus
Vomit
Rubella
Measles
31835 07 June
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Meningitis: causes, symptoms, diagnosis and treatment methods.
Definition
Meningitis is an infectious inflammation of the meninges of the brain and spinal cord, accompanied by intoxication, fever, increased intracranial pressure syndrome, meningeal syndrome, as well as inflammatory changes in the cerebrospinal fluid.
The meninges are connective tissue membranes that cover the brain and spinal cord. There are dura mater, arachnoid and pia mater.
The dura mater of the brain has a dense consistency and thickness of 0.2-1 mm; in places it fuses with the bones of the skull. The arachnoid membrane is a thin, translucent, non-vascular connective tissue plate that surrounds the brain and spinal cord. The soft shell is a thin connective tissue plate directly adjacent to the brain, corresponds to its relief and penetrates into all its recesses. In its thickness is the vascular network of the brain.
The most common inflammation is inflammation of the pia mater, and the term “meningitis” is used.
Causes of meningitis
The meninges can be involved in the inflammatory process primarily and secondary. Meningitis that occurs without a previous general infection or disease of some other organ is called primary. Secondary meningitis develops as a complication of an existing infectious process. Secondary ones include tuberculous, staphylococcal, pneumococcal meningitis. The primary ones are meningococcal, primary mumps, enteroviral meningitis and others.
The disease is transmitted by airborne droplets, household contact or nutrition.
Purulent inflammation of the meninges can be caused by various bacterial flora (meningococci, pneumococci, and less commonly, other pathogens). The cause of serous meningitis is viruses, bacteria, fungi.
According to the forecast, the most dangerous is tuberculous meningitis, which occurs when there is a tuberculous lesion in the body. The development of the disease occurs in two stages. At the first stage, the pathogen, through the bloodstream, infects the choroid plexuses of the ventricles of the brain with the formation of a specific granuloma in them. In the second, inflammation of the arachnoid and soft membranes is observed (as a rule, the membranes of the base of the brain are affected), which causes acute meningeal syndrome.
The development process of meningococcal meningitis also consists of several stages:
- contact of the pathogen with the mucous membrane of the nasopharynx;
- entry of meningococcus into the blood;
- penetration of the pathogen through the blood-cerebrospinal fluid barrier, irritation of pia mater receptors by toxic factors and inflammation.
The course of the infectious process depends on the pathogenic properties of the pathogen (the ability to cause disease) and the state of the human immune system.
Previous viral diseases, sudden climate change, hypothermia, stress, concomitant diseases, therapy that suppresses the immune system can be significant for the occurrence and course of meningitis.
Classification of the disease
According to the type of pathogen:
- Viral meningitis (influenza, parainfluenza, adenovirus, herpes, arbovirus (tick-borne), mumps, enterovirus ECHO and Coxsackie).
- Bacterial meningitis (meningococcal, tuberculous, pneumococcal, staphylococcal, streptococcal, syphilitic, brucellosis, leptospirosis).
- Fungal (cryptococcal, candidiasis, etc.).
- Protozoal (toxoplasmosis, malaria).
- Mixed.
According to the nature of inflammation:
- Serous.
- Purulent.
According to the mechanism of occurrence:
- Primary.
- Secondary.
With the flow:
- Spicy.
- Subacute.
- Fulminant.
- Chronic.
By severity:
- Easy.
- Medium-heavy.
- Heavy.
According to the prevalence of the process:
- Generalized.
- Limited.
According to the presence of complications:
- Complicated.
- Uncomplicated.
Symptoms and syndromes of meningitis
There are a number of syndromes common to all meningitis:
- meningeal syndrome - manifested by rigidity (increased tone) of the neck muscles and long back muscles, hypersthesia (increased sensitivity) of the sensory organs, headache, vomiting, changes in the cerebrospinal fluid;
- cerebral syndrome - manifested by drowsiness, impaired consciousness, nausea, vomiting, dizziness, psychomotor agitation, hallucinations;
- asthenovegetative syndrome – manifested by weakness, decreased ability to work;
- convulsive syndrome;
- general infectious syndrome - manifested by chills and fever.
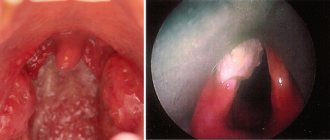
Meningococcal meningitis ranks first among purulent meningitis.
Its incubation period ranges from 1 to 10 days, with an average of 2-4 days. The disease usually begins acutely against the background of complete health or shortly after nasopharyngitis. Patients can indicate not only the day, but also the hour of illness; they are worried about chills, body temperature above 38℃, severe bursting headache, aggravated by any noise and movement of the head. Patients may experience pain in various parts of the body, and touching causes excruciating sensations. Vomiting is not associated with food intake and does not bring relief. Soon, stiffness of the neck and long back muscles sets in. Patients take a “meningeal” position. Infants cry constantly, they may experience bulging fontanelles and gastrointestinal disorders. Pneumococcal meningitis, as a rule, is observed in young children against the background of an existing pneumococcal process (pneumonia, sinusitis).
With streptococcal meningitis, hepatolienal syndrome (enlarged liver and spleen), renal failure, adrenal insufficiency, petechial rash (hemorrhages due to damage to the capillaries, as a result of which blood, spreading under the skin, forms round spots, the size of which does not exceed 2 mm).
Purulent meningitis caused by Pseudomonas aeruginosa and fungi are rare. The diagnosis is established only after additional laboratory tests.
Serous tuberculous meningitis is characterized by a gradual onset, although in rare cases it can manifest itself acutely. At the onset of the disease, patients complain of fatigue, weakness, irritability, and sleep disturbances. The temperature is usually no higher than 38℃, and there is an intermittent moderate headache. On the 5-6th day of illness, the temperature rises above 38℃, the headache intensifies, nausea, vomiting, and drowsiness appear. Unconsciousness develops quickly. A divergent strabismus, a low position of the upper eyelid in relation to the eyeball, and pupil dilation may be observed.
When diagnosing mumps meningitis, it is important to identify recent contact with someone with mumps.
Clinical manifestations of damage to the meninges may develop even before the enlargement of the salivary glands.
Enteroviral meningitis is characterized by two- and three-wave fever with intervals between waves of 1-2 or more days. Other manifestations of enterovirus infection are almost always observed (muscle pain, skin rash, herpangina).
For the diagnosis of measles and rubella meningitis, an indication of contact with a patient with these diseases, as well as typical clinical symptoms of measles or rubella, is of great importance.
Diagnosis of meningitis
To confirm the diagnosis of meningitis, the doctor may prescribe a set of laboratory and instrumental studies:
- clinical blood test with determination of hemoglobin concentration, number of erythrocytes, leukocytes and platelets, hematocrit and erythrocyte indices (MCV, RDW, MCH, MCHC), leukoformula and ESR (with microscopy of a blood smear in the presence of pathological changes);
Causes of the disease
The main causes of meningitis in children, symptoms and signs, lie in various infectious pathogens. The types of disease differ from each other depending on the sources:
- Bacterial. Often the disease is provoked by microbes, in particular, we are talking about staphylococcus, streptococcus, meningococcus, and E. coli.
- Viral. People suffering from meningitis often have herpes, mumps, and influenza viruses.
- Candida. Occurs due to candida and critococci.
- Simple microbes. These include amoebas and toxoplasma.
In a separate group, diseases of a combined form appear. In this situation, the disease appears due to several different pathogens.
Diagnosis of meningitis
The diagnosis of meningitis can be made based on the results of additional studies - laboratory and instrumental:
- detailed blood test;
- fundus examination;
- X-ray examination of the skull;
- heart electrocardiograms;
- electroencephalography;
- computer and magnetic resonance imaging.
To confirm the diagnosis of meningitis, doctors use bacteriological examination of mucus from the nasopharynx and cerebrospinal fluid. During bacterioscopic examination of cerebrospinal fluid, smears are stained with Gram or methylene blue. To exclude fungal meningitis, the specimen containing cerebrospinal fluid is stained with ink. Laboratory assistants isolate a pure culture on media with the addition of normal horse serum or cattle serum and identify it by biochemical activity and antigenic structure.
In case of viral meningitis, in preparations prepared with Gram staining and ink, it is impossible to identify the causative agent of the infection. Cultivation of bacteria and fungi also gives negative results. By culturing cellular material with standard laboratory cell lines, a pathogen serologically identical to the measles virus can be isolated. Rubella virus is isolated using the co-cultivation method.
To identify oligoclonal immunoglobulins, the method of agarose gel electrophoresis or isoelectric focusing of cerebrospinal fluid gamma globulins is used. Immunoglobulins appear in a number of viral infections. As a result of immunological studies, viral antigens or antibodies are detected in the cerebrospinal fluid, and the nucleic acid of the virus is detected using the polymerase chain reaction method. The enzyme immunoassay method detects pathogen antigens in feces, urine or saliva. Express methods allow you to quickly and early determine the presence of the herpes simplex virus antigen in the cerebrospinal fluid and blood or the DNA of the virus (using the polymerase chain reaction method).
CSF cytosis in meningitis
Analysis of cerebrospinal fluid allows not only to confirm the diagnosis, but also to differentiate purulent and serous meningitis, identify the causative agent of the disease, determine the degree of intoxication, and also makes it possible to monitor the effectiveness of treatment.
Bacteriological examination of cerebrospinal fluid in the case of tuberculous meningitis may give a false negative result. Detection of tubercle bacilli in the cerebrospinal fluid depends on the thoroughness of the research. At the Yusupov Hospital, all diagnostic procedures are performed using modern medical equipment and the use of new drugs and techniques. The results of studies conducted at the Yusupov Hospital are reliable and as informative as possible.
How can you get infected?
If you are interested in how you can become infected with meningitis, then first you should know about the way the infection multiplies. The methods of its reproduction are different, but the most common are:
- Airborne (the patient may sneeze and cough).
- Contact and household (personal hygiene rules are not followed).
- Oral-fecal (eating unwashed foods or eating with unwashed hands).
- Hematogenous (infection occurs through blood).
- Lymphogenic (infection through lymph).
- Placental (at the time of pregnancy and birth of a child from mother to her fetus).
- If a person bathes in dirty water, the infection enters the body.
The incubation period for this disease ranges from 2 to 4 days, this period from infection to the first signs. But sometimes it lasts a couple of hours or, on the contrary, it takes up to 20 hours. It is also important to consider that the disease can be primary and secondary. The first option is an independent disease. The second is a consequence of the fact that there is already an infection in the body, for example, a person suffers from influenza, otitis media, tuberculosis.
meningitis symptoms
If it is serous meningitis, then it is considered contagious. If the disease is secondary, then other people will not become infected with it.
Causes of meningitis
Meningitis can be of infectious or non-infectious origin. The infectious form of the disease develops as a result of the penetration of microorganisms into the body: bacteria, viruses, fungi and parasites. Non-infectious meningitis develops in patients as a result of taking certain medications and the formation of tumors.
Make an appointment
In medicine, classification is used according to the type of pathogenic microorganisms. It is important for a modern person to know how to recognize meningitis and what types of disease exist:
- bacterial meningitis is most often caused by streptococci, meningococci, pneumococci and Haemophilus influenzae, which are transmitted by airborne droplets;
- viral meningitis. The most common form of the disease. This type is characterized by the least severity. The causative agents of viral meningitis are enteroviruses;
- fungal meningitis develops as a result of the activity of certain types of fungal microorganisms;
- parasitic meningitis.
The list of therapeutic measures for meningitis is determined by the factors that caused the development of the disease. Thus, when treating bacterial meningitis, antibiotics are prescribed, which are ineffective for viral meningitis. If a person knows how to recognize meningitis, then the likelihood of diagnosing the disease at the initial stage and the effectiveness of therapeutic measures are high.
It is not possible to determine meningitis on your own. The clinical picture of the disease is varied. Signs differ according to the etiological factor. The initial symptoms of meningitis are often mistaken for cold symptoms. As the infection spreads, the condition worsens sharply. The high risk of death due to meningitis persists for 1-2 days from the onset of the first pathological symptoms. Delayed diagnosis and therapy lead to the development of severe, life-threatening complications.
Who is at risk?
A key factor contributing to the onset of meningitis is a weak immune system. It is the body’s defense against various infections. Human immunity becomes weak due to:
- previously suffered infectious diseases (respiratory, pneumonia, pharyngitis, influenza, sore throat),
- chronic pathologies, especially syphilis, HIV, tuberculosis, liver cirrhosis, severe stress,
- vitamin deficiency and strict diets,
- head and back injuries,
- total hypothermia of the body,
- alcohol and drug abuse,
- long-term use of tablets with non-compliance with recommendations.
All this can cause infection in a person, as the body becomes weak.
Prevention
The most effective way to reduce the burden of disease and mitigate the negative impact of meningitis on public health is to provide long-term protection against the disease through vaccination.
In the risk group for meningococcal meningitis and meningitis caused by group B streptococcus, antibiotics are also used for preventive purposes. Both vaccination and antibiotics are used to control epidemics of meningococcal meningitis.
Vaccination
Registered vaccines against meningococci, pneumococci and haemophilus influenzae have been on the market for many years. There are several different strains (also called serotypes or serogroups) of these bacteria, and vaccines aim to provide immunity to the most dangerous ones. Over time, great strides have been made in terms of coverage of different strains and availability of vaccines, but a universal vaccine against all these pathogens has not yet been developed.
Meningococci
There are 12 serogroups of meningococci, of which in most cases the causative agents of meningitis are bacteria of serogroups A, B, C, W, X and Y.
There are three types of vaccines:
- Polysaccharide-protein conjugate vaccines are used to prevent and respond to disease outbreaks: Such vaccines provide long-term immunity and also prevent the carriage of infection, thereby reducing the spread of infection and creating herd immunity.
- They are effective in protecting children under two years of age from the disease.
- These vaccines come in different forms: monovalent vaccines (serogroup A or C)
- quadrivalent vaccines (serogroups A, C, W, Y).
- combination vaccines (meningococcus serogroup C and haemophilus influenzae type b)
Global public health response: eliminating epidemics of group A meningitis in the African meningitis belt
Before the introduction of the conjugate vaccine against group A meningococcus as part of mass vaccination campaigns (since 2010) and its inclusion in the routine vaccination calendar (since 2016) in the countries of the African meningitis belt, this pathogen caused 80-85% of all meningitis epidemics. As of April 2022, 24 of the 26 countries in the meningitis belt had conducted mass prevention campaigns among children aged 1–29 years (nationally or in high-risk areas), and half of them included the vaccine in their national routine schedules. vaccinations. Among the vaccinated population, the incidence of serogroup A meningitis has decreased by more than 99%, and no cases of serogroup A meningococcal disease have been identified since 2022. To avoid resurgence of epidemics, it is critical that efforts continue to include this vaccine in the routine immunization schedule and support high level of vaccination coverage.
Isolated cases and outbreaks of meningitis caused by meningococcal serogroups other than serogroup B continue to be reported. The introduction of multivalent meningococcal conjugate vaccines is a public health priority to eliminate epidemics of bacterial meningitis in the African meningitis belt.
Pneumococcus
There are more than 97 known serotypes of pneumococci, 23 of which cause the majority of cases of pneumococcal meningitis.
- Conjugate vaccines are effective from 6 weeks of age for the prevention of meningitis and other severe pneumococcal infections and are recommended for vaccination of infants and children under 5 years of age, and in some countries, adults over 65 years of age, as well as representatives of certain risk groups. Two conjugate vaccines are used that protect against pneumococcal serotypes 10 and 13. New conjugate vaccines designed to protect against more pneumococcal serotypes are currently in development or have already been approved for vaccination in the adult population. Work continues to create protein-based vaccines.
- There is a polysaccharide vaccine designed to protect against 23 serotypes, however, like other polysaccharide vaccines, it is considered less effective than conjugate vaccines. It is used mainly for vaccination against pneumonia among people over 65 years of age, as well as members of certain risk groups. It is not used to vaccinate children under 2 years of age and is less effective in preventing meningitis.
Haemophilus influenzae
There are 6 known serotypes of haemophilus influenzae, of which the main causative agent of meningitis is serotype b.
- There are conjugate vaccines that provide specific immunity to haemophilus influenzae serotype b (Hib). They are a highly effective means of preventing disease caused by Hib and are recommended for inclusion in routine vaccination schedules for newborns.
Group B streptococcus
There are 10 known serotypes of group B streptococci, of which the most common causative agents of meningitis are streptococci types 1a, 1b, II, III, IV and V.
- Currently, work is underway to create conjugate and protein vaccines to prevent infection with group B streptococci in mothers and newborns.
Prophylactic use of antibiotics (chemoprophylaxis)
Meningococci
Timely administration of antibiotics to persons who have been in close contact with patients with meningococcal infection reduces the risk of transmission of infection. Outside the African meningitis belt, chemoprophylaxis is recommended for family members of patients who are in close contact with them. In countries with a meningitis belt, it is recommended to prescribe chemoprophylaxis to persons who have had close contacts with patients in the absence of an epidemic. The drug of choice is ciprofloxacin; Ceftriaxone is prescribed as an alternative.
Group B streptococcus
In many countries, it is recommended to identify mothers whose children are at risk for group B streptococcus. One way to achieve this goal is universal screening of pregnant women for carriage of group B streptococcus. To prevent group B streptococcal infection in newborns, mothers at risk are prescribed penicillin intravenously.
When should you see a doctor?
Every person needs to know how to detect signs of meningitis in children . There is no need to delay contacting a doctor if you often experience headaches, nausea and vomiting, an increase in body temperature, photophobia, sensitivity to sounds, or muscle pain in the back of the head. Also considered key symptoms are apathy and a constant desire to sleep, fainting, anxiety, and convulsions. A rash with meningitis is also observed; it affects the skin and mucous membranes. Mental disorders are also observed.
diagnosis of meningitis
Meningitis must be treated by a doctor in the infectious diseases department.
Pain due to meningitis
The most characteristic sign of pathology is headache. It occurs in any form of meningitis and appears from the first days of the disease. Headaches can vary in nature, but, as a rule, patients complain that their entire head hurts. Also, attacks of nausea and vomiting are often observed against the background of headaches.
What kind of pain occurs?
The manifestation of pain directly depends on the localization of the area of brain damage, the nature of the occurrence of meningitis (viral or infectious, or as a consequence of the development of the disease due to narrowing of blood vessels and spinal disorders).
In all cases, the nature of the headache will be different. Pain depends on the location of the inflammation, its prevalence, and the degree of impact on brain function.
Headache with serous meningitis
With serous meningitis, moderate pain is observed throughout the skull. In this case, there is no fever or increase in body temperature. The patient also experiences chills, nausea and vomiting against the background of constant headaches. However, after vomiting the patient does not feel any relief.
How does a headache occur with purulent meningitis?
With this form of meningitis, the patient develops severe headaches that are bursting in nature. The pain either subsides or increases again. Characteristic symptoms in this case are nausea, vomiting, fever, and chills.
Pain from subarachnoid hemorrhage
In this situation, headaches are constant, that is, they do not subside either day or night, neither in summer nor in winter. Headache is characterized by intense, sharp and acute manifestation.
How does a headache occur with tuberculous meningitis?
This is the weakest form of meningitis in its manifestations, characterized by an increasing nature of the manifestation of symptoms. Patients experience constant weakness, increased sweating, and depression. Nausea and vomiting occur very rarely.
With any form of meningitis, headaches lead to blurred vision. Patients often develop intolerance to loud sounds and photophobia. The pain intensifies several times when pressing on the area of the temples or eyes.
How to prepare for going to the doctor?
To go to the doctor, you don’t need to make any extensive preparations; on the contrary, if there are symptoms of meningitis , you shouldn’t put off going to the doctor, in this case you need to react immediately. Just remember all the signs that you had and tell your doctor about them. This will help make a correct diagnosis. You can't ignore these signs. Signs of meningitis in an adult can appear within a couple of hours, so urgent help is needed to avoid complications and even death.
Treatment of purulent meningitis
For purulent meningitis, patients are treated only in a hospital. Patients should immediately undergo a lumbar puncture with further bacterioscopic examination of the cerebrospinal fluid. After the etiology of meningitis has been established, the patient is prescribed a course of antibiotics. The latter often involves the use of ampicillin with drugs from a number of cephalosporins, including cefotaxime, ceftriaxone and ceftazidime. If the causative agent of purulent meningitis is not identified, initial therapy consists of intramuscular administration of aminoglycosides or their combination with ampicillin. In severe forms of purulent meningitis, intravenous antibiotics may be prescribed.
To reduce brain swelling, dehydration therapy with mannitol and furosemide can be prescribed. If we talk about the pathogenetic type of treatment, it involves the use of dexamethasone or prednisolone, in a word, glucocorticosteroids. The prescribed doses will depend on the severity of the disease. In addition, doctors prescribe symptomatic therapy. If the patient also has a sleep disorder, then tranquilizers are prescribed. In order to relieve psychomotor agitation and eliminate seizures, lytic mixtures, as well as valproic acid or diazepam, are prescribed. Infusion therapy will be prescribed in the presence of infectious-toxic shock.
How is the treatment carried out?
Treatment of meningitis is performed using several methods:
- Antimicrobial. Used when illness is caused by germs.
- Antiviral. Here doctors prescribe interferon and glucocorticosteroids to block the spread of the virus and improve the functioning of the immune system.
- Antifungal. If the disease appears due to candida, then antimycotic medications are used.
Therapy is also aimed at eliminating symptoms, that is, they give pain-relieving injections, normalize body temperature, and eliminate intoxication and dehydration.
How is meningitis treated?
At the Yusupov Hospital, patients can receive a full range of medical services for the detection and treatment of meningitis, rehabilitation after illness and prevention. Patients with meningitis can contact the neurologist clinic of the Yusupov Hospital every day for 24 hours to receive emergency care.
When patients are admitted to the Yusupov Hospital, a comprehensive diagnosis is carried out, including a number of examinations to identify the causes of meningitis, collection of complaints and symptoms. Patients with meningitis need inpatient treatment, so the Yusupov Hospital has created comfortable living conditions and ensures interaction with qualified personnel.
Misconceptions regarding the treatment of meningitis
- You can get meningitis if you don't wear a hat. Usually these phrases scare children. Sources of infection are considered to be a consequence of the inflammatory process, but not cold.
- Meningitis is not a dangerous disease at all. In reality, death is possible.
- Meningitis cannot be cured. In reality, fungal and bacterial forms can be treated with drugs, since special drugs have been created against such infections. If the form is viral, then things are worse, since there are no effective antiviral agents.
- After meningitis, a person is prescribed disability. In reality, after suffering bacterial meningitis, only 20% of people become disabled. The most common complication is hearing loss, but there are also problems with remembering and completing schoolwork if meningitis is detected in children.
Risk group
Children and the elderly are at risk for meningitis. In addition, this disease is often diagnosed in people with an absent spleen and immunodeficiency.
The spread of meningitis, like all other infectious diseases, is more active in crowded places, closed groups, for example, in kindergartens, schools, student dormitories, barracks, since it is easier to get meningitis if you are in the company of asymptomatic carriers.
Most often, meningitis is transmitted by airborne droplets. This mechanism of infection transmission is considered the most common and characteristic of meningitis of viral origin. The infectious agent is transmitted through coughing, sneezing, kissing and sexual contact.
Newborn babies can become infected from an infected mother through the birth canal. The likelihood of infection is especially high in children born by caesarean section. Bacterial and viral meningitis can be transmitted this way.
Infection with meningitis can occur through the oral-fecal route: through dirty food or untreated water.
In addition, meningitis can develop as a result of the bite of an insect or animal that carries an infectious agent.
What prevention is there?
There is a special vaccination against meningitis. This is what helps prevent the spread of the disease. It should be done for people who often communicate with infected people. Doctors also recommend doing this to children, as they are often exposed to this disease. Vaccination against meningitis is indicated for people with weak immune systems.
Moreover, prevention consists of increasing human immunity. It is necessary to strengthen the body, lead a healthy lifestyle, play sports, often be in the fresh air, and also protect yourself from infectious sources. You can also drink complexes with vitamins and minerals to boost your immunity. It is very important to maintain a balanced diet.
Prognosis of purulent meningitis
According to statistics, about 15% of all cases of purulent meningitis are fatal. If the diagnosis was made in a timely manner and treatment was started urgently, then the prognosis of the disease will be favorable.
It should be said that after a person has had purulent meningitis, he may develop asthenia with characteristic liquor-dynamic disturbances and inherent hearing loss of a sensorineural nature. Also, in some cases, subtle focal symptoms may be observed.
Such severe complications after suffering purulent meningitis, such as complete deafness, hydrocephalus, amaurosis, dementia or epilepsy, are very rare today.