Meningitis is a disease during which the membranes of the brain (meninges and subarachnoid space) become inflamed. It is caused by viruses and bacteria, depending on this the course of the disease occurs. In any case, this is a dangerous disease that requires medical treatment. It can lead to infection of the bloodstream or brain, as well as sepsis, which can be fatal.
Bacterial meningitis is believed to be more severe. If this form is diagnosed, the patient requires emergency medical care. In patients with viral meningitis, the symptoms and course of the disease are milder, but treatment is also in a hospital.
Meningitis in adults and children can have different symptoms, so next we will look at these two groups separately.
According to statistics, 90% of meningitis cases are children. In adults, those bacteria and viruses that can cause meningitis provoke the appearance of sore throat or tonsillitis. In some cases, the infection reaches the brain, affecting it and causing inflammation. Meningitis can also be a complication after sinusitis, tuberculosis and other similar diseases.
What is this?
Meningitis (from the Latin meninx - “brain membrane”, suffix -itis - “inflammation”) is an inflammation of the membranes of the brain and spinal cord.
It is the membranes, and not the brain tissue itself. Inflammation of the brain is encephalitis (from the Latin encephalon - “brain”, suffix -itis - “inflammation”).
The brain has three membranes:
- hard;
- arachnoid (arachnoid);
- soft (Fig. 1).
Figure 1. Meninges of the brain.
Source: SVG by Mysid, original by SEER Development Team [1], Jmarchn / Wikipedia (Creative Commons Attribution-Share Alike 3.0 Unported license) The dura mater is adjacent to the inner surface of the skull. It consists of two leaves: outer and inner. The outer leaf is tightly adjacent to the inner surfaces of the bones of the vault and base of the skull, the inner leaf forms dense outgrowths of this shell into the cranial cavity, which play the role of a frame for the brain and divide it into several sections. Between the leaves there are important formations - venous sinuses. They collect blood, which flows from the brain, enters the jugular veins and then into the heart through the superior vena cava.
The arachnoid membrane is thin, it occupies an intermediate position between hard and soft and connects them to each other.
Finally, the pia mater is loose and covers the brain, extending into all its grooves and crevices. In the thickness of the soft shell there are a large number of vessels that nourish the brain tissue.
Most often (perhaps due to the abundant blood supply), it is the pia mater that becomes inflamed. However, inflammation of the dura and arachnoid membranes also occurs. If both the arachnoid and soft membranes are inflamed at the same time, the disease is called leptomeningitis, if we are talking only about the hard membrane - pachymeningitis.
The spinal cord also has dura, arachnoid and pia mater. In structure, they are almost no different from the membranes of the brain. Their inflammation is also called meningitis. It is dangerous because it can spread to the tissue of the spinal cord itself. However, these will be different pathological conditions with their own complications.
Prognosis of viral meningitis
For most adult patients with viral meningitis, the prognosis is good. In only 10% of cases, the disease can result in severe complications. Such complications include headache, asthenia, coordination disorders, memory impairment, inattention, and problems with concentration. However, all these symptoms of viral meningitis pass quite quickly - within a few weeks, less often - a couple of months. For children, the prognosis is less favorable, since the disease leads to serious complications such as intellectual impairment, mental retardation, and hearing loss.
Causes
There are many reasons why inflammation can occur.
All of them are divided into two large groups: infectious and non-infectious.
Infectious causes
Pathogens that can cause meningitis include:
- bacteria (meningococcus, pneumococcus);
- viruses (enteroviruses, herpesviruses);
- mushrooms (candida);
- protozoa (malarial plasmodium, toxoplasma).
The most common are bacterial and viral meningitis. Protozoal infections are usually recorded only in certain regions, and fungal infections are typical for people with sharply reduced immunity, for example, patients with HIV infection in the last stages.
In this case, the infection can penetrate to the meninges in several ways. Thus, with an existing purulent infection of the nasal sinuses, inflammation of the middle ear or purulent pathology of the teeth, it can spread by contact to nearby tissues and organs. In the presence of an open craniocerebral injury or a crack in the skull bones, the pathogen can also penetrate with the lymph flow along the nerve endings. However, most often the infection enters the cranial cavity through the bloodstream.
A healthy person becomes infected from a carrier of the infection through airborne droplets (through coughing, sneezing and kissing), through contaminated food and untreated water. In some cases, the pathogen is transmitted from mother to fetus, or as a result of the bite of an insect vector (for example, in the case of malaria).
When it enters the body, the pathogen enters the blood and immediately causes inflammation of the meninges (primary meningitis), or affects other organs and tissues, and then through the bloodstream reaches the meninges and brain (secondary meningitis).
How often do people get meningitis and how dangerous is it?
Every year, about 2.8 million cases of meningitis are registered worldwide.1 More than 300 thousand become fatal, of which a third are children under 5 years of age.
Every fifth survivor of the disease has complications: behavioral problems, incoordination, hearing loss, paralysis, seizure activity, etc. The highest morbidity and mortality rates are observed in the “meningitis belt” located in sub-Saharan Africa, from Senegal in the west to Ethiopia in the east. This small area accounts for more than 10% of all reported cases of the disease (Fig. 2).
Figure 2. Incidence of meningitis in the world (number of cases per 100 thousand population), 2016. Source: WHO
Bacterial meningitis
As a rule, it is the most difficult. The main pathogens: meningococcus, pneumococcus, staphylococcus, Haemophilus influenzae, listeria, tubercle bacillus.
Most epidemics (including outbreaks in the meningitis zone) are caused by meningococcus, or the bacterium Neisseria meningitidis.
Meningococcus causes different forms of infections:
- asymptomatic carriage of bacteria, when a person does not even suspect that he is infected. According to research, from 5 to 10% of the total population of the planet become carriers4.
- nasopharyngitis, occurring with symptoms of a typical cold;
- meningitis;
- meningococcemia (meningococcal sepsis).
Meningococcal meningitis and sepsis can often be characterized by a lightning-fast course, then no more than a day passes from the onset of the disease to death. Therefore, at the first signs of meningococcemia or with the development of meningitis, when the causative agent of the disease has not yet been identified, it is necessary to seek medical help as soon as possible and prescribe antibiotics. In this case, the count goes to hours and even minutes.
Carriage of meningococcus, as well as increased sensitivity to the pathogen, often occurs among members of the same family. Therefore, if there are several children in a family, and one of them has already suffered meningococcal meningitis, it is recommended to examine and, if necessary, treat and vaccinate the remaining children, as well as their parents.
Another bacterium that also often causes meningitis is Streptococcus pneumoniae, also known as pneumococcus. Its difference is that in addition to meningitis, it causes sinusitis, otitis, pneumonia and other diseases. In this case, the infection can spread over time and develop into secondary meningitis. That is why it is important to begin treatment of pneumococcal diseases as early as possible and not wait for the pathological process to worsen.
Viral meningitis
Viral meningitis occurs almost twice as often as bacterial meningitis. However, they are easier. With a mild form of viral meningitis, the symptoms go away on their own, without specific treatment, within 7-10 days. The mortality rate from viral meningitis with proper treatment is 5-13%³.
Among viruses, meningitis is most often caused by enteroviruses (Coxsackie viruses and echoviruses) - up to 80% of all cases5 - and herpes viruses.
Fungal meningitis
Most often found in people with immunodeficiencies. For example, cryptococcal meningitis in AIDS or candidal meningitis caused by the Candida fungus, which normally lives on a person’s skin and inside the body and does not cause any problems.
Fungal meningitis develops when an infection spreads from the lungs to the brain and spinal cord and requires mandatory use of antifungal drugs. It is not transmitted from person to person.
Protozoal meningitis
It is also rare and mainly occurs in people with weakened immune systems. The most common pathogens are Toxoplasma gondii and Plasmodium falciparum.
Separately, parasitic meningitis is distinguished.
Why don't all infections end in meningitis?
Despite the abundance of infectious agents, meningitis occurs infrequently. Meningococcal infection often occurs asymptomatically or in the form of nasopharyngitis; enteroviruses and herpesviruses also affect other organ systems. This happens for two reasons. Firstly, a healthy immune system has time to cope with the infectious agent before any serious symptoms appear. Secondly, the blood-brain barrier (BBB) protects the brain from exposure to microbes. It is a physiological barrier between the blood and the central nervous system (brain and spinal cord), consisting of various types of cells. It protects brain tissue from toxins, microorganisms, cells and active immune system molecules that circulate in the blood. Through it, nutrients needed by the brain are selectively supplied. If the BBB is weakened or damaged, its genetic characteristics, or with hereditary or acquired high sensitivity to the microorganism, the latter is able to penetrate the barrier. However, pathogens that account for the majority of cases of meningitis (meningococci, pneumococci, listeria, Haemophilus influenzae) have additional mechanisms for penetrating the protective barrier.
Non-infectious causes
Such meningitis is the most rare. This includes forms caused by non-infectious diseases or a specific reaction to a drug.
What non-communicable diseases can cause meningitis? For example, autoimmune diseases, in which the immune system begins to destroy the body’s own tissues: systemic lupus erythematosus, rheumatoid arthritis and others.
Meningitis can also occur:
- with ruptures of benign tumors (cysts) located in the brain area;
- when the membranes of the brain are damaged by a malignant tumor;
- brain and spinal cord injuries;
- after operations performed on the brain;
- reactive in response to medications (non-steroidal anti-inflammatory drugs, certain groups of antibiotics, etc.).
Meningitis in children: symptoms, signs and causes
The cause of meningitis in children can be viruses of different natures - polio, Coxsackie, enteroviruses, etc. The disease is also caused by bacteria: staphylococci, meningococci, Haemophilus influenzae, etc. A newborn can become infected during childbirth.
The risk of meningitis is very high in the following categories of children:
- premature babies with weak immune systems;
- newborns who were born with hypoxia, infections and severe pregnancy in the mother;
- young children (most often under three years of age) who have other foci of infection (ARVI, tonsillitis, otitis, etc.);
- children with brain and spinal cord injuries;
- children diagnosed with disorders of the nervous system.
At-risk groups
There are factors that increase your risk of getting meningitis. These include:
- Age. Newborns, children of primary school age, adolescents 13-17 years old, as well as older people are considered more susceptible to meningitis pathogens.
- Organized teams. Outbreaks of meningococcal infection have been observed more than once in places where a large number of people are forced to stay in one area for a long time: in barracks, university campuses, etc.
- Medical factors. This may include certain health problems: immunodeficiency conditions and diseases of the immune system, HIV infection, absence of a spleen, taking certain groups of medications that lower natural immunity (chemotherapy, cytostatics, etc.), as well as surgical interventions.
- Contact with infections that cause meningitis. This factor is especially relevant for microbiologists, who may regularly come into contact with meningitis pathogens due to the specific nature of their work.
- Trips. Visiting geographic areas where a particular pathogen is endemic (its characteristic habitat) also increases the risk of meningitis. For example, staying in the countries of the meningitis belt in Africa.
Preventive measures for viral meningitis
Of course, there are preventive measures that, if followed, can help prevent the disease. It must be remembered that the virus is spread by airborne droplets and also depends on the rules of food processing and personal hygiene. Based on this, it becomes clear that in order to prevent the disease, it is necessary to exclude any contact with patients with ARVI, mumps, influenza, properly handle water and food, and maintain personal hygiene.
It is extremely important to consult a doctor promptly for advice. Timely identification of the causative agent of the disease and proper therapy will help reduce the rate of spread of infection. If the patient is isolated in time, the risk of infecting his family with the virus can be reduced. If viral meningitis is detected in a child attending a kindergarten, the child must be quarantined for a period of two weeks. All premises of the institution must be disinfected.
It is quite difficult to prevent an epidemic of viral meningitis, since the virus is highly resistant to environmental factors. In addition, the disease can be caused by a variety of viruses, so it is quite difficult to develop a uniform standard for prevention. Therefore, the only thing that can help prevent illness is personal hygiene (hand washing, frequent sanitation, disinfection of premises).
Types of meningitis
There are several classifications of the disease:
- Depending on the pathogen, infectious meningitis is usually divided into:
- bacterial;
- viral;
- fungal;
- protozoans.
- According to the development mechanism, they are distinguished:
- primary meningitis - develops without previous general infection and inflammation of other tissues and organs. In this case, the infection, having entered the body, first affects the meninges.
- Secondary meningitis is a complication of another disease.
- According to the nature of the inflammatory process and changes in the cerebrospinal fluid, meningitis occurs:
- serous: lymphocytes predominate in the cerebrospinal fluid (cerebrospinal fluid, which is examined to make a diagnosis). This picture is typical for most viral meningitis.
- purulent: neutrophils predominate in the cerebrospinal fluid, which is typical for bacterial meningitis.
- according to the prevalence of the inflammatory process:
- limited meningitis: the area of inflammation is limited to a separate area of the brain (for example, basal meningitis - inflammation of the meninges at the base of the brain);
- generalized meningitis - the meninges of all areas are affected.
Forms of meningitis
The forms of the course differ in the speed of development of the inflammatory process and the severity of the disease:
- Meningitis can be:
- fulminant (development of symptoms of meningitis in less than 24 hours);
- acute (inflammation develops in 1-2 days);
- subacute (develop over a period of several days to several weeks);
- chronic (develop slowly and last 4 weeks or longer).
- According to the severity of symptoms, they are distinguished:
- light form;
- moderate meningitis;
- severe form;
- extremely severe form.
Lumbar puncture
Lumbar puncture is rightfully considered the most effective method for diagnosing the disease. Cerebrospinal fluid examination reveals mildly elevated protein levels, normal glucose concentrations, and lymphocytosis.
In the first two days after infection of the body, cytosis is predominantly neutral. That is why it is worth repeating the study after 8-12 hours to monitor whether a lymphocytic shift has appeared or not. As a rule, the glucose concentration in viral meningitis is normal. Its decrease indicates tuberculous or fungal meningitis, as well as a non-infectious disease.
Examination of the cerebrospinal fluid also suggests isolation of the virus from it. However, this method is rather auxiliary, since it does not allow obtaining an extensive clinical picture of the disease. This is due to the fact that the virus is present in the cerebrospinal fluid in small quantities. Moreover, the disease can be caused by a variety of viruses, and they need to be cultured differently. To isolate the virus, you need to obtain at least two milliliters of cerebrospinal fluid, and then immediately send the material to the laboratory.
The virus can be isolated not only from cerebrospinal fluid, but also from other sources. For example, adenoviruses and enteroviruses can be detected in a patient’s stool, cytomegalovirus in urine, enteroviruses and arboviruses in blood, and mumps virus and enteroviruses in nasopharyngeal washings. However, it must be taken into account that the presence of enteroviruses in stool may not indicate viral meningitis, but a recent infectious disease.
Symptoms of meningitis
With infectious meningitis, the general symptoms, as a rule, differ little, do not depend on the pathogen and at first are similar to the symptoms of a common cold. These are chills, fever, weakness, drowsiness, headache, muscle discomfort. As the temperature increases, the breathing and heart rate increases.
Over time and the development of inflammation of the meninges, more specific symptoms appear:
- photophobia and increased sensitivity to any external irritants;
- rigidity (tension, tight mobility) of the neck muscles;
- feeling of nausea and vomiting against a background of severe headache. In this case, vomiting does not bring relief.
Apathy and confusion, convulsions may develop. This is the so-called meningeal syndrome caused by damage to the meninges.
Important ! Symptoms may be milder because you are taking antibiotics for another condition. And also in people with weakened immune systems (due to the use of drugs or with diseases that suppress the immune system (for example, AIDS), in alcoholics and in the very elderly. In the elderly, the only symptom may be confusion.
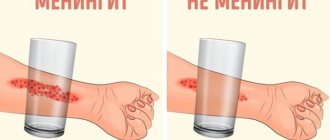
In addition to the main symptoms, additional symptoms characteristic of a specific pathogen may be observed. Thus, one of the forms of meningococcal infection is meningococcal sepsis. This is the most dangerous form of infection. In addition to the symptoms of meningitis, elements of a hemorrhagic rash can be found on the body, which do not disappear with pressure. You can check this using a glass beaker: if, when you press the wall of the glass on an element of the rash, it does not turn pale and does not disappear, you should suspect meningococcemia.
Hemorrhagic rash due to meningococcemia. Source: Journal of global infectious diseases / Open-i (Attribution 2.0 Generic)
The rash in this case appears due to the fact that meningococcus secretes a toxin that affects the walls of blood vessels. The blood supply to the limbs and internal organs is disrupted, which can lead to shock, necrosis and death.
Hemorrhagic rash can occur not only with meningococcemia. For example, it may be characteristic of various vasculitis - a group of diseases in which inflammation of the walls of blood vessels occurs. However, meningococcemia in any case is a condition requiring emergency medical care. Therefore, if you notice that a rash has been added to the general infectious symptoms, you should immediately consult a doctor for examination.
Signs of meningitis in babies
The clinical picture of meningitis in newborns and children of the first years of life differs from the clinical picture in adults.
The regulatory processes and immunity in the child’s body are not yet mature enough, so in most diseases, general symptoms prevail over local ones. In addition, the child is still too young to complain about something or show where it hurts. Therefore, it is more difficult to make an accurate diagnosis. Symptoms of meningitis in young children may include:
- restless behavior and irritability;
- constant crying, the child is almost impossible to calm down;
- refusal to feed;
- vomit;
- lethargy, difficulty waking up;
- heat.
In severe cases of meningitis in children under one year of age, bulging fontanelles may be observed due to increased intracranial pressure.
Meningitis
Meningitis is a disease that causes inflammation of the meninges: the protective membranes that cover the brain and spinal cord. Meningitis is most often caused by bacteria, viruses, protozoa and fungi. However, a non-infectious form of meningitis is possible, when the meninges become inflamed due to certain diseases, medications, or injuries. (1)
Causes of meningitis
The causes of the disease are various types of pathogens. Depending on their type, there are types of meningitis that they can cause:
- bacterial. It can be caused by various types of bacteria, including meningococci, staphylococci, streptococci, E. coli and others.
- viral. Possible pathogens of this form are mumps, herpes, influenza viruses, etc.;
- fungal can be caused by candida, cryptococcus;
- a form of meningitis caused by protozoa - its causes can be amoebas, toxoplasma and other protozoa;
- a mixed form of meningitis occurs if several pathogens are simultaneously detected in the body, each of which can cause meningitis.
Types, forms of meningitis
Depending on the speed of development of the disease, several forms are distinguished. Very rapid, sudden development of symptoms is a fulminant form of meningitis. The acute form of meningitis develops within 1–2 days. In subacute meningitis, symptoms develop over several days or weeks. Chronic meningitis lasts more than 4 weeks, and if after the symptoms disappear, the disease returns again, then it is recurrent meningitis.
Based on the type of inflammatory process, there are two types of meningitis - serous, which most often develops with a viral infection (enteroviruses, adenoviruses, mumps virus, influenza, tick-borne encephalitis) and purulent meningitis - a more severe form caused by a bacterial infection. The most common causative agents of purulent bacterial meningitis are meningococci, pneumococci, and Haemophilus influenzae type b (Hib).
Based on their origin, forms of meningitis are divided into primary and secondary. Primary develops as an independent disease. Secondary meningitis is a consequence or complication of an infection already existing in the body, for example, otitis media, influenza, tuberculosis, and often occurs in the form of serous meningitis.
According to the prevalence of inflammation, they are distinguished: spinal (or spinal cord meningitis) - the inflammatory process develops in the membranes of the spinal cord. If the inflammation is mainly localized in the upper part of the brain, then it is convexital meningitis, and with inflammation of the lower part of the brain, basal meningitis develops. The process, which involves both the brain and the spinal cord, is called cerebrospinal - this is how meningococcal meningitis often occurs. (1)
Symptoms of meningitis of the brain
Depending on the cause of meningitis, the symptoms of this disease may vary. But meningitis also has common symptoms called meningeal. They are divided into general cerebral symptoms - arising due to increased intracranial pressure and true meningeal symptoms, which arise due to inflammation of the lining of the brain. (1)
Among the early cerebral symptoms, headache most often appears. It can be widespread, or it can be observed in certain areas of the head; the severity of pain also varies. For many, the pain intensifies with noise, changing position, or turning on the lights. Young children may react to it with the so-called “brain scream” - these are repeated, monotonous, high-pitched screams.
The headache may be accompanied by severe sudden vomiting, which does not bring relief. There may be seizures, tics (uncontrolled movements of small muscles), and changes in consciousness.
Meningeal symptoms may include:
- typical pose with head thrown back, arms bent and legs pulled up to the stomach (“cooper dog pose”);
- rigidity (stiffness) of the neck muscles: an attempt to press the patient’s chin to the chest from the side fails;
- other symptoms indicating irritation of the meninges.
Other symptoms may vary depending on the type of pathogen that led to the disease and the type of meningitis. They are discussed separately in the description of the corresponding forms.
Viral meningitis
Viral meningitis can be caused by enteroviruses, including Coxsackie A, ECHO, mumps, parainfluenza viruses, viruses of the herpes family (causing herpes simplex, herpes zoster, Epstein-Barr disease, roseola infantile), tick-borne encephalitis virus and others.
According to the type of inflammation, this is most often serous meningitis.
The incubation period - the time from the moment the pathogen enters the body until the development of symptoms of the disease - in adults averages from 6 to 14 days. In children, it may be shorter or longer, and the signs of the disease may be less pronounced.
Viral meningitis clinic
As a rule, the first complaints to appear are those that may indicate an infectious disease: weakness, malaise, fever, headache. Then, within 1–3 days, meningeal symptoms appear, which may include neck stiffness, Brudzinski's symptoms, Kernig's sign, hypersensitivity to light, sounds, and touch. In infants, the fontanel may bulge and pulsate, and Lesage's symptom may be observed, in which the child, taken from the armpits, pulls his legs toward his stomach.
With some types of viral serous meningitis, the clinical picture may be unexpressed, erased, complaints may be moderate, and meningeal symptoms may appear erased and not obvious. Thus, meningitis that occurs against the background of adenovirus infection often occurs without meningeal symptoms, but with severe inflammation of the nasopharynx and upper respiratory tract, conjunctivitis.
Meningitis caused by the mumps virus can occur with intense abdominal pain, signs of pancreatitis, and inflammation of the testicles or ovaries.
A prolonged course can occur with meningitis caused by herpes viruses. It often begins with signs of herpes - typical blisters on the mucous membranes, herpes zoster, etc. Often, such meningitis occurs without meningeal symptoms.
Meningitis with tick-borne encephalitis is usually characterized by a rapid onset, with a rise in temperature, severe intoxication, muscle pain and meningeal symptoms. It can occur in waves - after an acute period, the temperature drops, and after a few days it rises again. Recovery is often delayed; weakness, asthenia, and neurological symptoms persist for quite a long time.
Diagnosis of viral meningitis
Only a doctor can make a correct diagnosis, so if you suspect that a patient may have meningitis, you should seek medical help. The doctor will interview the patient or his relatives, examine and assess the condition, and if necessary, in order to make sure that the symptoms are caused by inflammation of the meningeal membranes, he will prescribe a sample of cerebrospinal fluid and an assessment of its indicators.
Treatment
In most cases, treatment of viral meningitis is symptomatic. Recommends bed rest, dim lighting. At the onset of the disease, detoxification therapy is carried out according to indications, drugs are prescribed to alleviate symptoms: headache, vomiting, fever, abdominal pain, spasms, convulsions. For meningitis caused by a virus from the herpesvirus family, the doctor may prescribe an intravenous drip of the antiviral drug acyclovir.
With proper treatment, viral meningitis is usually quite mild, and the prognosis in most cases is favorable. (12)
Prevention
Vaccination in accordance with the National Vaccination Calendar of the Russian Federation can serve as the optimal way to protect against the risk of developing certain forms of viral meningitis. This is a vaccination against polio, mumps and measles viruses.
For other viruses, measures aimed at reducing the risk of transmission of the virus from carriers and patients to healthy people may be effective. These include:
- identification of sick people and timely separation of contacts (quarantine);
- compliance with personal hygiene and sanitary standards;
- strengthening and maintaining immunity;
- a set of measures from health authorities. (12)
Bacterial meningitis
Bacterial meningitis can be caused by meningococci, pneumococci, Haemophilus influenzae, tubercle bacilli, as well as staphylococci, salmonella, listeria and other bacteria. The inflammatory process in the membranes of the spinal cord and brain, caused by bacteria, in most cases is purulent.
“In 2015 in the Russian Federation, out of 2452 cases of purulent bacterial meningitis […] the etiological structure was dominated by meningococcus (44%). Next in frequency of isolation was pneumococcus (26%), followed by Haemophilus influenzae (10%). The share of other microorganisms accounted for 19%.” (3)
According to source (3) “the greatest risk of developing purulent bacterial meningitis of any etiology is typical for children under 5 years of age, while the risk of developing generalized forms of meningococcal infection is more pronounced in this group, followed by hemophilic meningitis in this age group, followed by pneumococcal meningitis”
Meningococcal meningitis
An acute onset of the disease is typical for this form. Intoxication and fever can be severe, as well as other symptoms. The intensity of complaints increases very quickly, there is a severe headache, fever, repeated vomiting that does not bring relief, a sharp increase in sensitivity to light, sounds, touches, and movement. Meningeal symptoms soon follow: “pointing dog pose,” Kernig’s and Brudzinski’s symptoms. In severe cases, the patient may experience convulsions, disturbances of consciousness, even coma.
In infants, the onset of purulent meningitis is accompanied by crying against a background of restless behavior, refusal to breastfeed, screams, a sharp reaction to touch (withdrawal of limbs, shuddering, increased crying), and convulsions. During the examination, meningeal symptoms may be detected - Lesage, stiff neck, typical meningeal posture.
As infection and inflammation spread and meningococci enter the blood, the patient's condition worsens. Meningococcemia (sepsis, blood poisoning) and infectious-toxic shock may develop. The symptoms described above will be accompanied by a hemorrhagic rash, and the functioning of the heart and blood vessels will deteriorate. With infectious-toxic shock, the deterioration of the condition can progress very quickly, fever and rash appear almost simultaneously, convulsions develop, and consciousness is impaired.
If you suspect meningococcal meningitis, it is recommended to seek urgent medical attention, as this form of meningitis can progress rapidly (even to death) and cause serious complications.
To make a diagnosis, the doctor relies on examination data and other examinations, based on the results of which he can prescribe cerebrospinal fluid tests, blood tests, and molecular diagnostic methods (for example, PCR) to clarify the type of pathogen. Based on the examination data, a diagnosis is established and treatment is prescribed: antibiotics, detoxification and symptomatic therapy; if necessary, correction of dehydration and other metabolic disorders can be carried out.
The duration of the disease with proper treatment can average from 2 to 6 weeks. Without treatment, there is a high probability of death or the development of severe complications leading to disability: according to the source, 10–20% of those who have had bacterial meningitis develop brain damage, hearing loss, cognitive impairment, and learning difficulties. In severe cases, gangrene of the fingers, toes, and ears is possible. (4)
Prevention
Currently, the following vaccines are registered in Russia for the prevention of severe forms of meningococcal infection.
- Meningococcal polysaccharide vaccines:
- monovalent (serogroup A) - monovalent against serogroup A polysaccharide dry;
- tetravalent (serogroups A, C, W, Y).
- Meningococcal conjugates:
- monovalent (serogroup C);
- tetravalent (serogroups A, C, Y, W).
Pneumococcal meningitis
This type of meningitis is caused by various types of pneumococci. Most often it develops in young children. “Young children under 2 years of age, whose bodies are unable to resist the infection, are especially defenseless against pneumococcus.” For this age group, pneumococci are the most common cause of severe forms of pneumonia, otitis media, and the second most common cause of bacterial meningitis. infection No. 1 and the most common cause of severe forms of pneumonia, otitis media, meningitis.” (9)
Pneumococcal meningitis occurs in the form of purulent meningitis, and can be primary or secondary, when it occurs against the background of an existing disease - otitis media, pneumonia, sinusitis.
The development of infection and, accordingly, complaints and clinical signs can develop in two forms. Primary pneumococcal meningitis develops, as a rule, acutely and is most typical for children over 5 years of age and adults. Body temperature rises sharply, symptoms of intoxication quickly appear - weakness, lethargy, drowsiness, nausea, headaches. After 2-3 days from the appearance of the first signs, meningeal symptoms and repeated vomiting without relief appear. Infants cry monotonously, periodically scream and moan, and the fontanel bulges. In children and adults, rashes may appear on the mucous membranes, in the form of small petechiae, resembling a hemorrhagic rash.
Often the process of inflammation affects the substance of the brain (meningoencephalitis), and against its background there are severe manifestations of the nervous system: convulsions, paresis, chaotic movements of the limbs, disturbances of consciousness, which can result in coma.
Secondary pneumococcal meningitis most often has a protracted course. Symptoms develop gradually over 2–7 days; at first they resemble ARVI; body temperature may be elevated, but sometimes may remain normal. Then, within a few days, the complaints become similar to those of acute pneumococcal meningitis.
To establish a diagnosis and prescribe adequate therapy, the doctor may order blood and cerebrospinal fluid sampling followed by laboratory testing. Treatment consists of prescribing antibiotics to which the pathogen is sensitive, taking measures to maintain the functioning of organs and systems, and symptomatic therapy. (12)
With timely treatment, the condition begins to improve during the first week, and the inflammation and the symptoms caused by it gradually subside. However, the prognosis for pneumococcal meningitis is serious, since with this form of meningitis “complications in the form of mental retardation, impaired motor activity, epilepsy and deafness are significantly more common than in the outcome of bacterial meningitis of other etiologies” (9). The prognosis can be especially difficult if meningitis transforms into a septic form, which can lead to endo- and pericarditis, arthritis and other serious complications.
Prevention
According to the website yaprivit.ru, “mass vaccination reduces the incidence of pneumococcal meningitis by more than 80%... The carriage of pneumococci in children is decreasing, and accordingly, unvaccinated children and adults get sick less.”
In the Russian Federation, vaccination is carried out with the following vaccines:
- 10-valent pneumococcal conjugate vaccine - PCV10;
- 13-valent pneumococcal conjugate vaccine - PCV13.
Both of these vaccines can be used in children from 2 months of age and in adults.
- 23-valent polysaccharide vaccine - PPV23.
Can be used in children from the age of 2 years and adults. (6)(9)
Haemophilus influenzae meningitis (Hib meningitis)
This form of meningitis is caused by Haemophilus influenzae type b and is most often observed in children under 5 years of age, but can also occur in older children - up to 8 years of age, and an increase in incidence in adults has also been noted. (7)(9)
Complaints and symptoms depend on the age of the patient, the condition of his body and the duration of the disease. In children, Hib meningitis often begins suddenly, with fever, repeated vomiting, and headache. In young children, bulging fontanelle and severe anxiety. These general cerebral symptoms are accompanied by meningeal symptoms: Brudzinsky and Kernig symptoms, Lesage symptoms in children under one year of age, neck stiffness. Convulsions, disturbances of consciousness, even coma can also quickly appear.
If Hib meningitis develops as a secondary disease, then the development of symptoms is slow, starting with complaints about the underlying disease, and then the symptoms of meningitis and cerebral symptoms join.
Treatment begins immediately after diagnosis, even before receiving the results of blood and cerebrospinal fluid tests. Combinations of antibiotics are prescribed in large doses, symptoms are combated, complications are prevented, and after the examination data has been clarified, antibiotics are selected taking into account the identified pathogen.
The hemophilic form of meningitis is difficult to treat due to the peculiarity of the pathogen: Hib bacilli produce an enzyme that protects them from antibiotics. For this reason, a third of patients who received proper treatment develop various neurological complications: seizure syndrome, developmental delay, loss of hearing and vision. Mortality in severe purulent hemophilic meningitis can reach 16–20%. (1) (7) (9)
Prevention
A highly effective measure for preventing Hib meningitis (and other forms of Hib infection) is vaccination (8). Currently, vaccination of all children in the first year of life against this infection is included in the vaccination schedules of more than 180 countries around the world (8). Currently in Russia, unlike most other countries, the vaccine against Hib infection is recommended only for children from certain risk groups (5). In Russia, vaccines against Hib infection are available both in the form of monovaccines and as part of combined (5-, 6-component) vaccines.
Show sources
Sources
- Berezhnova I. A. Infectious diseases. - Textbook / I. A. Berezhnova - M.: RIOR. - 2007. - 319 p.
- Childhood diseases: textbook / Ed. A. A. Baranova - 2nd ed., - M.: GEOTAR-Media. - 2009. - 1008 p.
- Information and analytical review “Meningococcal infection and purulent bacterial meningitis in the Russian Federation. 2015.” Russian reference center for monitoring bacterial meningitis. - M., - 2016.
- Meningococcal infection [Electronic resource]. — Access mode: https://www.yaprivit.ru/diseases/meningokokkovaya-infekciya — Article. — (Date of access: 04/17/2018).
- Order of the Ministry of Health of the Russian Federation dated March 21, 2014 No. 125n “On approval of the national calendar of preventive vaccinations and the calendar of preventive vaccinations for epidemic indications” (with amendments and additions). — Access mode: https://base.garant.ru/. (Date of access: 04/17/2018).
- Abramtseva, M.V. Meningococcal infection. Conjugate polysaccharide meningococcal vaccines and new generation vaccines. Message 3 / M. V. Abramtseva, A. P. Tarasov, T. I. Nemirovskaya // Journal “Biopreparations. Prevention. Diagnostics. Treatment". Volume 16 No. 1 (57) / January-March 2016. — P. 3–13.
- Journal "Medical Alphabet" No. 6 / 2016, volume No. 1 Epidemiology and hygiene.
- World Health Organization. Haemophilus influenzae type b (Hib) vaccination position paper - July 2013. Wkly Epidemiol Rec 2013; 88:413-426 [Electronic resource]. — Access mode: https://www.who.int/wer/2013/wer8839.pdf. (Date of access: 04/17/2018)
- Pneumococcal infection [Electronic resource]. — Access mode: https://www.yaprivit.ru/diseases/pnevmokokkovaya-infekciya/. - Article. — (Date of access: 03/19/2017). (as of 04/17/2018)
SPRU.MENAC.18.03.0031(1)
When should you see a doctor?
You should seek medical help as soon as possible if you notice the following symptoms (all or some of them) in yourself or someone in your family:
- heat;
- excruciating headache;
- confusion;
- vomit;
- stiff neck muscles;
- rash.
Do you have meningeal symptoms? Call an ambulance immediately!
Checking for meningeal symptoms can help make a preliminary diagnosis. It can be done at home.
Symptom of neck stiffness
The patient lies on his back, without a headboard. While holding his chest with one hand, the other should be placed under the occipital region and try to bring the chin closer to the sternum. If the symptom is positive, then due to the increased tone of the muscles of the back of the head, it will be impossible to do this; the movement will cause involuntary resistance and pain in the patient. A measure of the severity of muscle tension is the distance between the patient's chin and sternum.
Kernig's sign
The patient lies on his back. You should bend one leg at the hip joint at an angle of 90°, and then try to straighten it at the knee joint (Fig. 4). If the symptom is positive, then straightening the leg at the knee will be impossible, this will cause resistance and pain.
Kernig's sign. Source: Annals of Indian Academy of Neurology/Open-i (Attribution-NonCommercial-ShareAlike 3.0 Unported)
Brudzinski's sign
This set of signs of meningitis includes several symptoms:
a) upper - bringing the chin closer to the chest while examining the rigidity of the muscles of the back of the head causes involuntary bending of the legs at the knees and bringing them in the stomach;
b) medium - the same reaction of bending the legs will be caused by pressing on the stomach above the pubic bones;
c) lower - examined simultaneously with Kernig's symptom - when trying to straighten one leg at the knee joint, the second leg bends at the knee and is brought to the stomach.
Lower and upper Budzinski's symptoms. Source: Annals of Indian Academy of Neurology/Open-i (Attribution-NonCommercial-ShareAlike 3.0 Unported)
Lesage's sign
In children of the first year of life and newborns, due to the natural increased tone of the limbs, the above tests are not informative. They are tested for Lesage's symptom: the child, raised by the armpits, pulls the legs towards the stomach and keeps them in a taut position (Fig. 3).
Figure 3. Lesage's sign. Source: image from the PSPbSMU website
You can learn more about the technique for checking meningeal symptoms by watching Video 1.
Video 1. Technique for checking meningeal symptoms. Source: ONMedU
Bacterial meningitis is a serious disease that can be fatal within a few days without prompt antibiotic treatment. Also, starting treatment late increases the risk of permanent brain damage. Therefore, even if you are not sure of your assumptions, feel free to consult a doctor. It is also important to consult a specialist if a family member or someone you live or work with has meningitis. You may need to take medicine to prevent infection.
Symptoms
When the incubation period ends, serous meningitis manifests itself with sharp and obvious signs, which are collectively called meningeal syndrome.
A sick child exhibits several symptoms from this list:
- Fever. An indispensable symptom of serous meningitis, occurring in two waves. First, the temperature rises to 39.5-40 degrees and usually lasts for about three days. Then it subsides and returns again in a day or two. In mild cases, the temperature may return in a “truncated” version – 37-38 degrees.
- Severe headache. It starts from the temples and smoothly moves to the back of the head. Bright light and noise increase pain.
- A characteristic symptom of childhood serous meningitis is limb cramps.
- Lack of appetite, nausea, vomiting (without relief), diarrhea, abdominal pain.
- Intoxication, which entails joint pain, general weakness, moodiness and irritability of the child.
- In children, meningitis is often accompanied by standard symptoms of respiratory diseases - runny nose and sore throat. Therefore, parents sometimes mistake it for acute respiratory infections and do not sound the alarm.
- Sick children from three years of age try to take a characteristic position: lying on their side, pressing their hands to their chest and knees to their stomach. The head is thrown back towards the back.
- The acute form of meningitis may be accompanied by impaired motor functions (partial paralysis and paresis).
- Double vision and strabismus are another symptom of the so-called reactive meningitis, which develops over a few hours.
- An attentive parent may notice increased tension in the neck muscles.
- Disorders of consciousness: from stupor and absent-mindedness to coma (in advanced acute form).
These signs can manifest themselves to a greater or lesser extent, singly, in groups or complexly.
For an accurate diagnosis, we check for the presence of certain types of meningeal syndromes:
- Kernig syndrome, when a child cannot straighten a leg bent at an angle of 90 degrees.
- Brudzinski syndrome is a reflex flexion of one leg while bending the other (or flexion of the legs simultaneously with flexion of the head).
- Lesage syndrome (for infants): when you hold a baby by the armpits, he bends his legs and pulls them towards his stomach. Swelling of the fontanelle is also observed.
- Mondonesi syndrome is a severe headache with light pressure on the eyeballs covered by the eyelids.
Some of the symptoms of serous meningitis are similar to those of the meningeal form of tick-borne encephalitis. Because this parasite is active during the summer (as are meningitis outbreaks), the diseases can be confused.
Diagnostics
To make a diagnosis of meningitis and determine its causative agent, it is necessary:
- Collect anamnesis. It is important to understand whether the patient has had contact with people infected with meningitis, has traveled to areas where meningitis is endemic, and whether he or she has specific immune status—possibly suffering from HIV or other immunodeficiencies, or taking medications that suppress the immune system.
- Assess the general condition. The doctor conducts a clinical examination of the patient, assesses the severity of his condition, and checks for the presence of specific symptoms.
- Carry out the necessary laboratory tests. This includes classic laboratory tests, such as a general urine test, a complete blood count, a biochemical blood test, and most importantly, a lumbar puncture.
Lumbar puncture is a procedure during which, under local anesthesia, the doctor inserts a special needle into the spinal cord (directly into its subarachnoid space) between the III and IV lumbar vertebrae and collects cerebrospinal fluid. Next, it is examined and the color, the presence of sediment, the predominance of certain cells, the presence of bacteria, the amount of protein and glucose are assessed. Based on the results of the study, it is possible to determine the type of meningitis, draw a conclusion about the nature of the inflammatory process, isolate the pathogen, and determine the necessary treatment.
It is worth noting that if bacterial meningitis is suspected, antibacterial therapy is prescribed immediately, before test results are obtained. This is done with the aim of starting treatment as early as possible, since in the case of meningococcal infection, the clock is ticking. Further, based on the test results, treatment can be adjusted and other antibiotics may be prescribed.
Treatment of meningitis
Treatment of meningitis must be carried out in a hospital setting and depends on its type. Until the results of the study are received, the patient is prescribed Cefotaxime and Ceftriaxox. This is the so-called starting antibiotic therapy. After receiving the tests, targeted antibiotic therapy is prescribed, depending on the bacteria detected and their sensitivity to the drug.
Symptomatic treatment may include infusion therapy, enteral or parenteral nutrition, rehabilitation exercises, which are recommended after relieving cerebral edema, treatment of complications and their prevention.
Treatment
Because acute bacterial meningitis can cause permanent brain damage, nerve damage, or death within hours, treatment should begin as quickly as possible without waiting for the results of diagnostic tests.
Mild meningitis with minor symptoms is usually caused by viruses and, with symptomatic treatment, goes away on its own within 7-10 days. For moderate and severe meningitis, the patient is hospitalized and antibiotics are prescribed. The drugs of choice at the first stage are penicillins and cephalosporins. If the results of the study reveal a bacteria resistant to the antibiotic, the drug is changed. If a herpes simplex virus is detected, an antiviral drug is prescribed. For other viruses, etiological (that is, directly affecting the pathogen) treatment has not been developed.
The antibiotic is discontinued when:
- clinical recovery;
- normalization of general blood count and cerebrospinal fluid indicators7.
In addition to antibiotics, the patient also receives corticosteroids (dexamethasone) to reduce cerebral edema and intracranial pressure, infusion and symptomatic therapy.
Serodiagnosis
The diagnosis can also be made based on the results of serodiagnosis. However, in most cases, such a study is carried out only to clarify the disease, and not to diagnose it. Using PCR (polymerase chain reaction), DNA of the herpes simplex virus can be detected in the cerebrospinal fluid.
In addition to specific studies, the patient must also undergo a number of general studies:
- general blood analysis;
- determination of ESR;
- hematocrit;
- plasma glucose;
- KFK;
- creatinine.
Usually, when diagnosing viral meningitis, you can do without instrumental studies such as EMG, CT, MRI, EEG. Research is carried out exclusively in case of a questionable or atypical diagnosis.
Complications of meningitis
Meningitis can cause persistent complications that remain with a person for life. There may also be complications that appear immediately and affect the prognosis.
Early
Early, especially dangerous complications of meningitis mainly concern acute bacterial forms. These include:
- Brain swelling. Within a short time, intoxication sharply increases, cerebral disorders increase, loss of consciousness and convulsions occur. Shortness of breath, tachycardia increases, and death can occur from paralysis of the respiratory center, which is located in the brain.
- Infectious-toxic shock. There is a rapid increase in body temperature and an increase in hemorrhagic syndrome. The pulse becomes rapid and thread-like, cold sticky sweat appears, shortness of breath, convulsions, and blood pressure decreases.
- Acute adrenal insufficiency or Watterhouse-Friderichsen syndrome. As a result of hemorrhage in the adrenal cortex, the latter cease to secrete vital hormones, incl. adrenaline and norepinephrine, necessary to maintain vascular tone. There is a sharp drop in blood pressure.
- Infection of other organs and systems (myocarditis, arthritis, epilepsy, paralysis, bleeding, etc.).
Late
According to one large-scale study, the average risk of complications after discharge from hospital is about 20%8.
The most common consequences of meningitis are:
- hearing loss and vision impairment;
- behavioral and cognitive problems;
- impaired coordination of movements;
- seizure disorder.
What is meningitis
Meningitis can affect any layers of the meninges.
In practice, doctors more often encounter lesions of the soft layer. Meningitis occurs with typical symptoms, but the disease must be properly diagnosed. Typically, patients complain of severe headaches and increased body temperature, but the decisive factor for diagnosing the pathology remains tension in the muscles of the back of the head, as a result of which tilting the head becomes problematic for the patient. Nonspecific symptoms in children are supplemented by weakness, loss of appetite, and irritability. The disease is caused by pathogenic microorganisms, viruses, fungi or protozoa. The danger of the disease is that the inflammatory process occurs in close proximity to the brain tissue, so it becomes a cause of death if left untreated. It is important to diagnose the pathology in a timely manner in order to provide first aid to the patient as soon as possible.
Prognosis and prevention
The prognosis of the disease depends on many factors: the type and form of meningitis, the age of the patient, his immunological status and chronic diseases, and the timeliness of medical care.
Important! When treated early, most patients recover. The longer treatment is delayed, the higher the likelihood of death and irreversible brain damage with the development of late neurological complications.
How to prevent the development of meningitis?
Prevention of meningitis can be divided into nonspecific and specific. Non-specific prevention includes general safety measures: regular hand washing, use of individual personal hygiene items, compliance with protective measures when in contact with infected people, as well as general measures to strengthen the body’s immune system, which relate to sleep and rest patterns, healthy eating, regular physical activity .
Specific preventive measures include vaccination.
Despite the fact that there are a large number of meningitis pathogens, the risk of the disease can be significantly reduced, since vaccines have been developed against the most dangerous bacterial pathogens (vaccine against Haemophilus influenzae, meningococcus, pneumococcus).
Vaccines against Haemophilus influenzae and pneumococcus are included in the Russian preventive vaccination calendar. This means that vaccination of children against these pathogens is free, available to the entire population and carried out according to a specific schedule:
- Haemophilus influenzae: 3, 4, 5, 6 months and revaccination at 18 months. Children from risk groups are vaccinated (presence of neurological diseases, intestinal pathologies, immunodeficiency; children in orphanages).
- Pneumococcus: 2, 4, 5 months and revaccination at 15 months.
If a person was not vaccinated against these infections in childhood, he can always go to a medical facility and get vaccinated as an adult.
Vaccination against meningococcus is not yet included in the calendar, but is provided for risk groups and for epidemiological reasons. The vaccine is also available for those wishing to vaccinate themselves, but on a paid basis. The Russian Union of Pediatricians recommends not to neglect this opportunity and to vaccinate the child to protect against a dangerous infection. From 2022, the vaccine is planned to be included in the national calendar of preventive vaccinations along with the vaccine against rotavirus and chickenpox.
Meningitis: which doctor treats it?
Since meningitis is most often an infectious disease, treatment is prescribed by infectious disease doctors . They also carry out diagnostics. Moreover, all this is done after the patient is hospitalized, i.e. in the infectious diseases department. Additionally, observation by a neurologist is necessary, since the infection affects the nervous system.
Even suspicion of meningitis requires immediate hospitalization until the causes are clarified . This disease has a very high mortality rate and an even higher rate of neurological complications. For prevention, you need to get vaccinated, maintain hygiene, and eat right. Be healthy!
Sources
- Global, regional, and national burden of meningitis, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 [Electronic resource] // The Lancet. Neurology, 2022.
- Epidemiology of Meningitis Caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenza [Electronic resource] // cdc.gov, 2016.
- Rebecca M. Cantu; Joe M Das. Viral Meningitis [Electronic resource] // NCBI, 2022.
- Meningitis [Electronic resource] // who.int
- What Do You Want to Know About Meningitis? [Electronic resource] // healthline.com, 2022.
- YouTube. Research and assessment of meningeal symptoms in a child.
- Clinical protocol for diagnosis and treatment. Meningitis in children and adults [Electronic resource] // rcrz.kz, 2016.
- Kenadeed Hersi; Francisco J. Gonzalez; Noah P. Kondamudi. Meningitis [Electronic resource] // NCBI, 2022.
Diagnosis of meningitis
The main methods for diagnosing meningitis include:
- Cerebrospinal fluid examination. Cerebrospinal fluid is obtained using a lumbar puncture. When diagnosing meningitis, various fluid characteristics are determined (transparency and color, number and composition of cells, amounts of protein, glucose, and the presence of microflora), which make it possible to identify changes characteristic of meningitis.
- X-ray of the skull.
- Fundus examination.
- Computer and nuclear magnetic resonance tomography.
- Electroencephalography.
The diagnosis of meningitis is established based on a combination of 3 signs:
- Presence of symptoms of meningitis.
- Signs of infection.
- The presence of characteristic changes in the cerebrospinal fluid.
Basic principles of management
They try to normalize body temperature, reduce headaches, and reduce the patient’s tension. For these purposes, non-narcotic analgesics, sedative therapy, and anti-nausea medications are used. Indications and implementation of artificial pulmonary ventilation follow the same principles as for patients with TBI.
In severe cases, due to impaired consciousness, vomiting, enteral food intake is often difficult. On the first day, less often, in the first 2 days, an infusion of saline solutions is used to replenish the loss of fluids and electrolytes. They try to make do with the minimum possible volumes - 1.5-2.5 liters per day. At the same time, hypotension must be corrected without delay. It is not recommended to use glucose solutions (if there is no hypoglycemia) derived from hydroxyethyl starch. For unstable hemodynamics, doctors use vasopressor infusions. It is better to give preference to norepinephrine (Norepinephrine) or phenylephrine (Mezaton).
Hyponatremia occurs in approximately 30% of patients with meningitis and can lead to increased cerebral edema. It must be eliminated immediately. As soon as the patient’s condition becomes stable, they switch to enteral feeding with nutritional mixtures. Any hyperglycemia that occurs should be promptly corrected. Seizures can dramatically increase intracranial pressure. In most patients with severe meningitis, the level of intracranial pressure is elevated.
With meningitis, an increase in ICP is often caused not so much by cerebral edema, but by excess production of cerebrospinal fluid. Therefore, lumbar punctures and furosemide injections are often effective when it comes to reducing ICP. If these actions fail to reduce ICP, cerebral herniation may occur; osmotherapy with mannitol or 3-7.5% sodium chloride solution should be used. In general, ICP quickly normalizes when antibacterial treatment is given. If the temperature drops, consciousness is clear, and focal neurological symptoms are not observed, then there is no need for decongestant therapy.
Personnel protection and patient isolation
To prevent airborne spread of infection, patients with meningococcal infection or meningitis of unknown etiology are isolated during the first 24 hours of antibiotic therapy. Infection of personnel can occur during tracheal intubation, CPR, and artificial ventilation. Standard precautions must be taken.
The need for prophylactic antibiotics should be considered for ICU staff if a patient is diagnosed with meningococcal meningitis. The likelihood of infection remains for 24 hours after antibiotics are prescribed. The chance of infection is higher among younger employees and people over 60 years old.
Use any of the following schemes:
1. Ciprofloxacin tablets, 500 mg twice a day. per day for 2 days;
2. Rifampicin tablets, 600 mg every 12 hours for 2 days.
Symptoms
Almost all patients have at least 2 of the typical four symptoms:
- Fever;
- Headache;
- Stiff neck;
- Impaired consciousness with a score of less than 14 points on the Glasgow scale.
A hemorrhagic rash is typical for meningococcal infection (rarely for pneumococcal, staphylococcal) and is localized on the torso, arms, legs, and butt. A rash on the face, and especially the earlobe and conjunctiva, is an unfavorable prognostic sign.
Forms of meningitis
The incubation period lasts from two to five days (rarely – up to 10 days). Doctors distinguish several forms of the infectious process - bacterial carriage (asymptomatic), meningococcal nasopharyngitis, meningitis, meningococcemia, combined form.
Bacterial carriage is an asymptomatic form characterized by the presence of a virus in the body that does not manifest itself in any way. There is no drug treatment for meningitis in adults.
Meningococcal nasopharyngitis. Local manifestations such as runny nose, nasal congestion, and sore throat are typical. Low-grade fever and general weakness are possible. After a week, the person either recovers or becomes a carrier of the bacteria.
Meningitis is a severe form of the disease with characteristic symptoms. The clinical manifestations and consequences of infectious meningitis will be discussed in more detail below.
Meningococcemia (the pathogen enters the blood) is a clinical form with typical and atypical symptoms. A characteristic symptom is a rash with bacterial meningitis.
Combined – the most severe form, combining the clinical manifestations of meningitis and meningococcemia.
On our website you can learn about the prevention of meningitis through vaccinations and make an appointment with a specialist.