Pneumonia in children is a fairly common disease, especially at a young age when the immune system is not yet fully developed. This is a lung infection caused by bacteria, fungi or viruses. It is important to carry out proper infection prevention and be attentive to the first symptoms of the disease that occur in young children. Currently, there is a highly effective treatment for pneumonia, but despite this, serious and dangerous complications are possible.
Bacterial pneumonia is characterized by a sudden onset with fever, respiratory distress, chest pain and deterioration in general condition. Symptoms vary depending on the patient's age. Among respiratory diseases, pneumonia is the leading single cause of childhood mortality worldwide, killing approximately 1.1 million patients before the age of 5 years.
General information about the disease
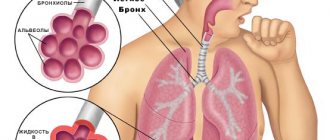
When a child gets sick with ARVI, a lot of mucus is produced in his bronchi. It tends to accumulate, especially in preschoolers, because their chest muscles are not yet developed enough for effective coughing. As a result, some areas of the lungs are deprived of ventilation and become vulnerable to pathogens. Viruses and bacteria settle in them, causing inflammation. In the viral form, the disease goes away in about 5-6 days without treatment, and if it is caused by bacteria, then special therapy is required.
Attention! Treatment must be precisely targeted to the pathogen; individual selection of the drug and dosage is necessary. Self-medication can lead to irreversible consequences.
Pneumonia can occur even in a newborn; it is of aspiration origin in this case, that is, the cause is the baby swallowing amniotic fluid during childbirth.
The disease has an excellent prognosis if treatment is started on time. Complicated cases requiring hospital treatment with intravenous drugs are only 8-10%.
Causes of pneumonia in childhood
- improper therapy for ARVI, self-medication;
- complication of other respiratory diseases;
- infections (in exceptional and very rare cases, a bacterial disease can be contagious);
- weak immunity as a factor that expands the number of causes of pneumonia - even injury.
The nature of the disease may even be toxicological. The mechanism of our body’s work is such that with a huge number of ailments, harmful, toxic – “garbage” – substances filtered by the circulatory system settle in the lungs. Due to this, “weak” areas and local blockages are formed. Infections, viruses, and inflammation then develop in them. Even ailments not directly related to the respiratory system often lead to pneumonia.
Antiviral drugs for pneumonia
Is it necessary to use antiviral drugs for pneumonia? More often, pneumonia has a mixed etiology; in other words, several pathogens can be present in the body at once: viruses, bacteria and sometimes even fungi. That is why doctors more often prescribe complex therapy, which includes both antibacterial and antiviral drugs. Of course, as with any other disease, self-medication and self-prescription of certain drugs is unacceptable, especially when it comes to the health of a child.
Symptoms of the disease
- Shortness of breath, which occurs even at normal body temperature.
- Severe and prolonged cough.
- Lack of spontaneous recovery within 7 days.
- Deterioration of condition after short-term improvement.
- High body temperature, rapidly rising after attempts to reduce it.
- The child cannot take a deep breath, filling the lungs. Attempts to do this lead to an attack of suffocating cough.
- With the bacterial form of the disease, the skin becomes pale, sometimes almost bluish. If the child’s skin is of normal color, then most likely he has viral pneumonia, which is less dangerous. Source: T.A. Kovtun, A.V. Tutelyan, S.V. Shabalina Features of the course of pneumonia in children and principles of therapy Epidemiology and infectious diseases, 2012, No. 3, pp. 52-56
Principles of treatment
When pneumonia is diagnosed in a newborn, treatment should begin as soon as possible. The prognosis for recovery directly depends on how quickly treatment is started. Treatment of pneumonia in newborns is complex and includes the following measures:
- taking antibiotics - in the first case, a broad-spectrum drug is prescribed; after receiving the results of blood biochemistry, the antibiotic can be replaced with another. Intramuscular administration of the drug is more effective. The lack of relief after 2 days indicates the wrong choice of antibiotic. For infants, preference is given to drugs of the penicillin group. However, it is worth noting that infection with pneumonia in a maternity hospital is most difficult to treat due to the extreme resistance of the pathogen to drugs;
- taking medications aimed at restoring intestinal microflora in order to prevent the development of dysbacteriosis;
- immunomodulators and vitamin complexes are prescribed as maintenance drugs after the main treatment;
- intravenous infusions of saline are prescribed for severe forms of the disease to reduce intoxication of the body;
- mucolytics to improve sputum discharge;
- antipyretics provide virtually no relief; they are taken to control the rise in body temperature;
- chest massage using vibration method for better sputum discharge;
- physiotherapy is mainly represented by inhalations, it begins to be used after the acute form of the disease is removed;
- in cases of severe disease, hormonal drugs may be prescribed;
- in case of oxygen starvation, the use of an oxygen mask is recommended.
Treatment of pneumonia in a child using folk methods and recipes is unacceptable. During treatment, it is important to fully care for the little patient around the clock, give him food as often as possible, and avoid overheating and hypothermia. On average, treatment lasts 10-15 days.
What types of pneumonia are there: classification
By localization:
- one-sided (one lung is affected);
- bilateral (both lungs are inflamed).
Based on its origin, pneumonia is divided into three types.
- Fungal (up to 5% of cases) is the rarest type of disease and the most dangerous. In childhood, it most often occurs against the background of improper and/or uncontrolled use of antibiotics.
- Bacterial (about 35% of cases) - occurs either separately or as a complication of a respiratory disease. Requires immediate medical attention for treatment with antibiotics.
- Viral (about 60% of patients) is a mild form of the disease, which in children goes away on its own in about a week, being cured by the body.
Methods of diagnosis and early detection
Even if you find a complete list of symptoms of pneumonia in your child and are almost sure of its origin, you should definitely consult a doctor to clarify the diagnosis and further treatment. Experts use the following methods for detecting pneumonia:
- listening with a stethoscope (wheezing, characteristic “gurgling” may be heard in the lungs);
- collecting anamnesis, visual examination to assess the child’s condition as a whole, listening to complaints;
- X-ray of the chest in two projections - frontal and lateral. Only a frontal image may not be informative in some cases, because it contains a cardiac shadow, which can “cover” the inflamed area;
- clinical blood test (reveals the nature of the disease, in addition to its presence). Source: L.S. Namazova-Baranova, T.V. Kulichenko, A.E. Malakhova, E.V. Starovoitova, M.D. Bakradze, I.L. Chashchina, I.L. Mityushin Pneumococcal pneumonia in children: lessons from everyday practice // Issues of modern pediatrics, 2012, v. 11, no. 4, pp. 65-72
Diagnostics
Only a doctor can correctly diagnose pneumonia in newborns.
Diagnosis of pneumonia in infants is made using the following methods:
- examination of mucous membranes and skin, measurement of body temperature;
- listening to the lungs for the presence of wheezing and hardness of breathing;
- instrumental studies:
- a general blood test to check for increased ESR and leukocytes, indicating the presence of inflammation;
- blood biochemistry is carried out to determine the pathogen;
- sputum culture is carried out to determine the sensitivity of the pathogen to medications;
- X-rays show the inflamed areas and the extent of their damage.
How is pneumonia treated in children?
If the viral form of pneumonia goes away on its own, then treatment of fungal and bacterial forms requires specialist intervention and medications.
- Bacterial pneumonia is treated with antibiotics and only as prescribed by a doctor. Here it is worth addressing parents who do not accept these drugs: before the introduction of antibiotics, more than a third of children died due to pneumonia! Therefore, you should not focus on possible complications, which are minimized in modern drugs (and they are not prescribed in long courses), but focus on guaranteeing a complete cure.
- Pneumomycosis, or a fungal type of pneumonia, requires antifungal medications. Treatment should only be prescribed by a doctor, since this form of the disease is the most dangerous, and the medications are among the most complex.
Parents can additionally take measures such as:
- maintaining the child’s usual lifestyle (albeit on sick leave) whenever possible, because bed rest and low physical activity lead to stagnant processes in the respiratory system;
- providing plenty of fluids to thin mucus in the airways and lungs;
- the temperature in the child’s room should be no higher than 21 degrees, and the humidity should be about 70%, so that the mucus does not stagnate and it is easier for the child to breathe.
The role of antiviral therapy in pneumonia
It is known that inflammation of the respiratory tract is usually a complication caused by a viral or bacterial infection. Even an experienced doctor cannot determine whether pneumonia is viral or of another nature and make a final diagnosis regarding the cause of the disease during the first examination of a small patient. To do this, it is necessary to do a number of clinical and laboratory tests, for example, conduct a sputum, blood test, and take an X-ray of the lungs. All this takes time, which, as a rule, is not much. Therefore, most often the doctor is prompted to the viral nature of pneumonia by a characteristic sound when listening to the respiratory tract. Thus, doctors can rightfully prescribe antiviral drugs. Such drugs include Viferon Suppositories. It contains interferon protein, which prevents the proliferation of viruses, as well as vitamins C and E, which are antioxidants and contribute to the better functioning of interferon in the human body. Thanks to its dosage form (rectal suppositories), Viferon, when introduced into the patient’s rectum, begins to act very quickly, without creating additional stress on the baby’s digestive system. The drug is indicated for children from the first days of life, and even for premature babies. The use of the drug VIFERON® as part of complex therapy makes it possible to reduce therapeutic doses of antibacterial and hormonal drugs, as well as reduce the toxic effects of this therapy.
Methods for effective prevention
Proper prevention does not include drug therapy. To prevent the disease you need:
- vaccinate your child in a timely manner;
- provide hardening, introduce physical education;
- breastfeed the baby in the first six months of life;
- do not smoke near the child;
- purify the air in the apartment;
- Consult a doctor in a timely manner if signs of unwellness occur. Source: https://www.ncbi.nlm.nih.gov/pubmed/31518547 Nascimento-Carvalho CM Community-acquired pneumonia among children: the latest evidence for an updated management // J Pediatr ( Rio J). 2019 Sep 10. pii: S0021-7557(19)30493-0. doi: 10.1016/j.jped.2019.08.003
Should I give my child antibiotics to prevent pneumonia?
If you find signs of ARVI in a child, then you should not give him antibiotics in advance, “for prevention.” Especially if you are going to do it yourself or on the recommendation of a pharmacist from your nearest pharmacy. According to the latest data, this measure will not only fail, but will also increase the likelihood of pneumonia for your child by almost 10 times.
Advantages of SM-Clinic
The children's department of our medical center employs some of the best pediatricians, pulmonologists and other specialists in the Northern capital.
Make an appointment at the first sign of a respiratory disease or its complications - we will help quickly and effectively.
If a child has a severe form of pneumonia and requires hospitalization, we will offer a comfortable and cozy room. The patient will be monitored around the clock by responsible medical personnel, and effective therapy will be provided.
Sources:
- T.A. Kovtun, A.V. Tutelyan, S.V. Shabalina. Features of the course of pneumonia in children and principles of therapy // Epidemiology and infectious diseases, 2012, No. 3, pp. 52-56.
- L.S. Namazova-Baranova, T.V. Kulichenko, A.E. Malakhova, E.V. Starovoitova, M.D. Bakradze, I.L. Chashchina, I.L. Mityushin. Pneumococcal pneumonia in children: lessons from everyday practice // Issues of modern pediatrics, 2012, vol. 11, no. 4, pp. 65-72.
- https://www.ncbi.nlm.nih.gov/pubmed/31518547 Nascimento-Carvalho C.M. Community-acquired pneumonia among children: the latest evidence for an updated management // J Pediatr (Rio J). 2022 Sep 10. pii: S0021-7557(19)30493-0. doi: 10.1016/j.jped.2019.08.003.
Pneumonia among all pulmonary pathologies in young children is almost 80%. Even with the introduction of progressive technologies in medicine - the discovery of antibiotics, improved diagnostic and treatment methods - this disease is still one of the ten most common causes of death. According to statistical data in various regions of our country, the incidence of pneumonia in children is 0.4-1.7%.
- Improper treatment of influenza and ARVI can lead to pneumonia in a child
- Pneumonia in children - differential diagnosis of ARVI, acute bronchitis and bronchiolitis
- Signs of pneumonia in a child. Symptoms of pneumonia in infants, children under one year old
- Chlamydial, mycoplasma pneumonia in a child
- Indications for hospitalization
- Treatment of pneumonia in a child
When and why can pneumonia occur in a child?
The lungs perform several important functions in the human body. The main function of the lungs is gas exchange between the alveoli and the capillaries that envelop them.
Simply put, oxygen from the air in the alveoli is transported into the blood, and carbon dioxide from the blood enters the alveoli.
They also regulate body temperature, regulate blood clotting, are one of the filters in the body, promote cleansing, the removal of toxins, breakdown products that occur during various injuries, and infectious inflammatory processes. And in the event of food poisoning, burns, fractures, surgical interventions, or any serious injury or illness, a general decrease in immunity occurs, and it is more difficult for the lungs to cope with the load of filtering toxins.
That is why very often a child develops pneumonia after suffering or against the background of injuries or poisoning.
Most often, the causative agent of the disease is pathogenic bacteria - pneumococci, streptococci and staphylococci, and recently cases of the development of pneumonia from pathogens such as pathogenic fungi, legionella (usually after staying in airports with artificial ventilation), mycoplasma, chlamydia, which are not They are rarely mixed or associated.
Pneumonia in a child, as an independent disease that occurs after serious, severe, prolonged hypothermia, is extremely rare, since parents try to prevent such situations.
As a rule, in most children, pneumonia does not occur as a primary disease, but as a complication after ARVI or influenza, less often than other diseases.
Why is this happening?
Many of us believe that acute viral respiratory diseases have become more aggressive and dangerous due to their complications in recent decades. This may be due to the fact that both viruses and infections have become more resistant to antibiotics and antiviral drugs, which is why they are so severe in children and cause complications.
One of the factors in the increase in the incidence of pneumonia in children in recent years has been the general poor health of the younger generation - how many children today are born with congenital pathologies, developmental defects, and lesions of the central nervous system.
A particularly severe course of pneumonia occurs in premature or newborn babies, when the disease develops against the background of an intrauterine infection with an insufficiently formed, immature respiratory system.
In congenital pneumonia, the causative agents are often herpes simplex virus, cytomegalovirus, mycoplasma, and when infected during childbirth - chlamydia, group B streptococci, opportunistic fungi, Escherichia coli, Klebsiella, anaerobic flora; when infected with hospital infections, pneumonia begins on the 6th day or 2 weeks after birth.
Naturally, pneumonia most often occurs in cold times, when the body already undergoes a seasonal adjustment from heat to cold and vice versa, overloads occur for the immune system, at this time there is a lack of natural vitamins in foods, temperature changes, damp, frosty, windy weather contribute to hypothermia of children and their infection.
In addition, if a child suffers from any chronic diseases - tonsillitis, adenoids in children, sinusitis, dystrophy, rickets (see rickets in an infant), cardiovascular disease, any severe chronic pathologies, such as congenital lesions of the central nervous system, developmental defects, immunodeficiency states - significantly increase the risk of developing pneumonia and aggravate its course.
The severity of the disease depends on:
- Extensiveness of the process (focal, focal-confluent, segmental, lobar, interstitial pneumonia).
- The age of the child, the younger the baby, the narrower and thinner the airways, the less intense gas exchange in the child’s body and the more severe the course of pneumonia.
- Places where and for what reason pneumonia occurred:
— community-acquired: most often have a milder course
— hospital: more severe, since infection with bacteria resistant to antibiotics is possible
- aspiration: when foreign objects, mixture or milk enter the respiratory tract.
The most important role is played by the general health of the child, that is, his immunity.
Improper treatment of influenza and ARVI can lead to pneumonia in a child
When a child gets sick with a common cold, acute respiratory viral infection, or influenza, the inflammatory process is localized only in the nasopharynx, trachea and larynx.
If the immune response is weak, and also if the pathogen is very active and aggressive, and the child is treated incorrectly, the process of bacterial reproduction descends from the upper respiratory tract to the bronchi, then bronchitis may occur. Further, inflammation can also affect lung tissue, causing pneumonia.
What happens in a child’s body during a viral disease?
In most adults and children, various opportunistic microorganisms - streptococci, staphylococci - are always present in the nasopharynx, without causing harm to health, since local immunity inhibits their growth.
However, any acute respiratory disease leads to their active reproduction, and if the parents act correctly during the child’s illness, the immune system does not allow their intensive growth.
What should not be done during ARVI in a child to avoid complications:
Antitussives should not be used.
Coughing is a natural reflex that helps the body clear the trachea, bronchi and lungs of mucus, bacteria, and toxins. If, to treat a child, in order to reduce the intensity of a dry cough, you use antitussives that affect the cough center in the brain, such as Stoptusin, Bronholitin, Libexin, Paxeladin, then an accumulation of sputum and bacteria in the lower respiratory tract may occur, which ultimately leads to pneumonia.
You cannot carry out any preventive antibiotic therapy for colds or viral infections.
Antibiotics are powerless against the virus, but the immune system must cope with opportunistic bacteria, and their use is indicated only if complications arise as prescribed by a doctor.
The same applies to the use of various nasal vasoconstrictors; their use promotes faster penetration of the virus into the lower respiratory tract, therefore Galazolin, Naphthyzin, Sanorin are not safe to use for a viral infection.
Drinking plenty of fluids - one of the most effective methods of relieving intoxication, thinning mucus and quickly clearing the airways is drinking plenty of fluids, even if the child refuses to drink, parents should be very persistent.
If you do not insist that the child drinks a sufficiently large amount of liquid, there will also be dry air in the room - this will help dry out the mucous membrane, which can lead to a longer course of the disease or a complication - bronchitis or pneumonia.
Constant ventilation, the absence of carpets and rugs, daily wet cleaning of the room in which the child is located, humidification and purification of the air using a humidifier and air purifier will help to quickly cope with the virus and prevent pneumonia from developing. Because clean, cool, moist air helps to thin sputum, quickly eliminate toxins through sweat, cough, and wet breath, which allows the child to recover faster.
Acute bronchitis and bronchiolitis - differences from pneumonia
ARVI usually has the following symptoms:
- High temperature in the first 2-3 days of illness (see antipyretics for children)
- Headache, chills, intoxication, weakness
- Qatar of the upper respiratory tract, runny nose, cough, sneezing, sore throat (not always the case).
In case of acute bronchitis against the background of acute respiratory viral infection, the following symptoms may occur:
- Slight increase in body temperature, usually up to 38C.
- At first the cough is dry, then it becomes wet, there is no shortness of breath, unlike pneumonia.
- Breathing becomes harsh, various scattered wheezes appear on both sides, which change or disappear after coughing.
- The radiograph shows an increase in the pulmonary pattern, and the structure of the roots of the lungs decreases.
- There are no local changes in the lungs.
Bronchiolitis occurs most often in children under one year of age:
- The difference between bronchiolitis and pneumonia can only be determined by X-ray examination, based on the absence of local changes in the lungs. According to the clinical picture, acute symptoms of intoxication and an increase in respiratory failure, the appearance of shortness of breath - are very similar to pneumonia.
- With bronchiolitis, the child’s breathing is weakened, shortness of breath with the participation of auxiliary muscles, the nasolabial triangle becomes bluish, general cyanosis and severe pulmonary heart failure are possible. When listening, a boxy sound and a mass of scattered fine-bubble rales are detected.
Signs of pneumonia in a child
When the infectious agent is highly active, or when the body’s immune response to it is weak, when even the most effective preventive treatment measures do not stop the inflammatory process and the child’s condition worsens, parents can guess from some symptoms that the child needs more serious treatment and urgent medical examination.
At the same time, under no circumstances should you start treatment with any traditional method. If it really is pneumonia, not only will this not help, but the condition may worsen and time will be lost for adequate examination and treatment.
Symptoms of pneumonia in a child 2 - 3 years old and older
How can attentive parents determine if they have a cold or viral illness that they should urgently call a doctor and suspect pneumonia in their child?
Symptoms that require x-ray diagnostics:
- After an acute respiratory infection or flu, there is no improvement in the condition for 3-5 days, or after a slight improvement, a jump in temperature and increased intoxication and cough reappear.
- Lack of appetite, lethargy of the child, sleep disturbances, and moodiness persist for a week after the onset of the illness.
- The main symptom of the disease remains a severe cough.
- The body temperature is not high, but the child has shortness of breath. At the same time, the number of breaths per minute in a child increases, the norm of breaths per minute in children aged 1-3 years is 25-30 breaths, in children 4-6 years old - the norm is 25 breaths per minute, if the child is in a relaxed, calm state. With pneumonia, the number of breaths becomes greater than these numbers.
- With other symptoms of a viral infection - cough, fever, runny nose - pronounced pallor of the skin is observed.
- If the temperature is high for more than 4 days and antipyretics such as Paracetamol, Efferalgan, Panadol, Tylenol are not effective.
Symptoms of pneumonia in infants, children under one year old
The mother can notice the onset of the disease by changes in the baby’s behavior. If a child constantly wants to sleep, becomes lethargic, apathetic, or vice versa, is capricious a lot, cries, refuses to eat, and the temperature may rise slightly, the mother should immediately consult a pediatrician.
Body temperature
In the first year of life, pneumonia in a child, the symptom of which is considered to be a high, unbroken temperature, is distinguished by the fact that at this age it is not high, does not reach 37.5 or even 37.1-37.3.
However, temperature is not an indicator of the severity of the condition.
The first symptoms of pneumonia in an infant
This is causeless anxiety, lethargy, loss of appetite, the baby refuses to breastfeed, sleep becomes restless, short, loose stools appear, there may be vomiting or regurgitation, runny nose and paroxysmal cough, which intensifies while the baby is crying or feeding.
Baby's breathing
Chest pain when breathing and coughing.
Sputum - with a wet cough, purulent or mucopurulent sputum (yellow or green) is released.
Shortness of breath or an increase in the number of breathing movements in young children is a clear sign of pneumonia in a child. Shortness of breath in infants may be accompanied by nodding of the head in time with breathing, and the baby also puffs out his cheeks and stretches out his lips, sometimes foamy discharge appears from the mouth and nose.
A symptom of pneumonia is considered to be exceeding the normal number of breaths per minute:
- In children under 2 months, the norm is up to 50 breaths per minute; over 60 is considered a high frequency.
- In children from 2 months to a year, the norm is 25-40 breaths, if 50 or more, then this is exceeding the norm.
- In children older than one year, the number of breaths exceeding 40 is considered shortness of breath.
Skin texture changes when breathing
Attentive parents may also notice retraction of the skin when breathing, usually on one side of the diseased lung.
To notice this, you should undress the baby and observe the skin between the ribs; it retracts when breathing. With extensive lesions, one side of the lung may lag behind during deep breathing.
Sometimes you can notice periodic stops in breathing, disturbances in the rhythm, depth, frequency of breathing, and the child’s desire to lie on one side.
Cyanosis of the nasolabial triangle
This is the most important symptom of pneumonia, when blue skin appears between the baby’s lips and nose. This sign is especially pronounced when the baby is breastfeeding.
With severe respiratory failure, slight blue discoloration may appear not only on the face, but also on the body.
Chlamydial, mycoplasma pneumonia in a child
Among pneumonias, the causative agents of which are not common bacteria, but various atypical representatives, mycoplasma and chlamydial pneumonia are distinguished.
In children, the symptoms of such pneumonia are somewhat different from the course of ordinary pneumonia. Sometimes they are characterized by a hidden, sluggish course.
Signs of atypical pneumonia in a child may be as follows:
- The onset of the disease is characterized by a sharp rise in body temperature to 39.5 C, then a persistent low-grade fever forms -37.2-37.5 or even normalization of temperature occurs.
- It is also possible that the disease begins with the usual signs of ARVI - sneezing, sore throat, severe runny nose.
- Persistent dry debilitating cough, shortness of breath may not be constant. This cough usually occurs with acute bronchitis, not pneumonia, which complicates the diagnosis.
- When listening, the doctor is most often presented with scant data: rare wheezing of various sizes, pulmonary percussion sound. Therefore, it is difficult for a doctor to determine atypical pneumonia based on the nature of wheezing, since there are no traditional signs, which greatly complicates the diagnosis.
- There may be no significant changes in the blood test for SARS. But usually there is an increased ESR, neutrophilic leukocytosis, combination with anemia, leukopenia, eosinophilia.
- A chest x-ray reveals a pronounced increase in the pulmonary pattern and heterogeneous focal infiltration of the pulmonary fields.
- Both chlamydia and mycoplasma have the ability to exist for a long time in the epithelial cells of the bronchi and lungs, so most often pneumonia is of a protracted, recurrent nature.
- Treatment of atypical pneumonia in a child is carried out with macrolides (azithromycin, josamycin, clarithromycin), since the pathogens are most sensitive to them (to tetracyclines and fluoroquinolones, too, but they are contraindicated for children).
Indications for hospitalization
The decision about where to treat a child with pneumonia - in a hospital or at home - is made by the doctor, and he takes into account several factors:
The severity of the condition and the presence of complications - respiratory failure, pleurisy, acute disturbances of consciousness, heart failure, drop in blood pressure, lung abscess, pleural empyema, infectious-toxic shock, sepsis.
Damage to several lobes of the lung. Treatment of focal pneumonia in a child at home is quite possible, but for lobar pneumonia it is better to treat it in a hospital setting.
Social indications are poor living conditions, inability to carry out care and doctor’s orders.
Age of the child - if an infant falls ill, this is grounds for hospitalization, since pneumonia in an infant poses a serious threat to life. If pneumonia develops in a child under 3 years of age, treatment depends on the severity of the condition and most often doctors insist on hospitalization. Older children can be treated at home, provided that the pneumonia is not severe.
General health - in the presence of chronic diseases, weakened general health of the child, regardless of age, the doctor may insist on hospitalization.
Treatment of pneumonia in a child
Antibiotics are the mainstay of treatment for pneumonia. At a time when doctors did not have antibiotics in their arsenal for bronchitis and pneumonia, pneumonia was a very common cause of death in adults and children, so in no case should you refuse to use them; no folk remedies are effective for pneumonia.
Parents are required to strictly follow all the doctor’s recommendations, provide proper care for the child, adhere to the drinking regime, nutrition:
Taking antibiotics must be carried out strictly on time; if the drug is prescribed 2 times a day, this means that there should be a break of 12 hours between doses, if 3 times a day, then a break of 8 hours. Antibiotics are prescribed - penicillins, cephalosporins for 7 days, macrolides (azithromycin, josamycin, clarithromycin) - 5 days. The effectiveness of the drug is assessed within 72 hours - improvement in appetite, decrease in temperature, shortness of breath.
Antipyretics are used if the temperature is above 39C , in infants above 38C. At first, antipyretic antibiotics are not prescribed, since it is difficult to assess the effectiveness of therapy. It should be remembered that during high temperatures the body produces the maximum amount of antibodies against the pathogen, so if a child can tolerate a temperature of 38C, it is better not to knock it down. This way the body can quickly cope with the microbe that caused pneumonia in the baby. If a child has had at least one episode of febrile convulsions, the temperature should be brought down already at 37.5C.
Feeding a child with pneumonia - lack of appetite in children during illness is considered natural and the child’s refusal to eat is explained by the increased load on the liver when fighting the infection, so you cannot force feed the child. If possible, you should prepare light food for the patient, exclude any ready-made chemicalized foods, fried and fatty, try to feed the child simple, easily digestible food - porridge, soups with a weak broth, steamed cutlets from lean meat, boiled potatoes, various vegetables, fruits.
Oral hydration - in water, natural freshly squeezed diluted juices - carrot, apple, weakly brewed tea with raspberries, rosehip infusion, water-electrolyte solutions are added (Rehydron, etc.).
Ventilation, daily wet cleaning, and the use of air humidifiers alleviate the baby’s condition, and the love and care of parents works wonders.
No general tonic (synthetic vitamins), antihistamines, or immunomodulators are used, since they often lead to side effects and do not improve the course and outcome of pneumonia.
Taking antibiotics for pneumonia in a child (uncomplicated) usually does not exceed 7 days (macrolides 5 days), and if you follow bed rest, follow all the doctor’s recommendations, in the absence of complications, the child will quickly recover, but within a month there will still be residual effects in the form cough, slight weakness.
With atypical pneumonia, treatment may take longer. P
When treated with antibiotics, the intestinal microflora in the body is disrupted, so the doctor prescribes probiotics - RioFlora Immuno, Acipol, Bifiform, Bifidumbacterin, Normobact, Lactobacterin.
To remove toxins after completion of therapy, the doctor may prescribe sorbents such as Polysorb, Enterosgel, Filtrum.
If the treatment is effective, the child can be transferred to a general regimen and walks from the 6-10th day of illness, and hardening can be resumed after 2-3 weeks.
In case of mild pneumonia, heavy physical activity (sports) is allowed after 6 weeks, in case of complicated pneumonia after 12 weeks.
Source: https://zdravotvet.ru/
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a pulmonologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Professor consultation | 4500 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Study of external respiratory function (RPF) with drug tests | 1800 rub. |
| X-ray of the chest organs (survey) | 1900 rub. |
| X-ray of the chest organs in 2 projections | 2900 rub. |