Autoimmune hepatitis (AIH) is a chronic inflammatory liver disease characterized by the loss of the body's immunological tolerance to tissue antigens [1, 2].
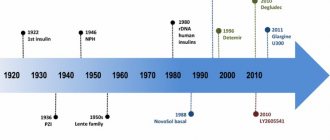
For the first time, information about severe liver damage with severe jaundice and hyperproteinemia appeared in the 30–40s. XX century. In 1950, the Swedish doctor Jan Waldenström observed chronic hepatitis with jaundice, telangiectasia, increased ESR, and hypergammaglobulinemia in 6 young women. Hepatitis responded well to treatment with corticotropin [3]. Due to the similarity of laboratory changes with the picture of systemic lupus erythematosus (the presence of antinuclear antibodies in the serum, positive results of the LE test), one of the names of the pathology became “lupoid hepatitis”.
Currently, autoimmune hepatitis is defined as chronic, predominantly periportal hepatitis with lymphocytic-plasmacytic infiltration and stepwise necrosis (Fig. 1). Characteristic manifestations: hypergammaglobulinemia, the appearance of autoantibodies in the blood.
Classification
Depending on the type of autoantibodies, three types of disease are distinguished:
- Type 1 AIH is the most common and is characterized by the appearance in the blood of antinuclear antibodies (ANA) and/or smooth muscle antibodies (SMA).
- In type 2 AIH, autoantibodies are formed to microsomal antigens of the liver and kidneys (anti-liver kidney microsomal type-1 antibodies, anti-LKM-1).
- Type 3 AIH is associated with the formation of autoantibodies to soluble liver antigen, liver and pancreas tissue (anti-soluble liver antigen/liver-pancreas antibodies, anti-SLA/LP).
- Some authors combine AIH 1 and AIH 3 due to the similarity of clinical and epidemiological features [4]. There are also crossover forms (overlap syndrome) of various autoimmune liver pathologies, including AIH: AIH + PBC (primary biliary cirrhosis), AIH + PSC ( primary sclerosing cholangitis). It is not yet entirely clear whether these diseases should be considered parallel ongoing independent nosologies or parts of a continuous pathological process.
AIH that developed de novo after liver transplantation performed for liver failure associated with other diseases is considered as a separate nosology [1, 5].
Autoimmune hepatitis is found everywhere. The prevalence of AIH in European countries is about 170 cases per 1 million population. Moreover, up to 80% of all cases are type 1 AIH. Type 2 AIH is unevenly distributed - up to 4% in the USA and up to 20% in Europe.
Mostly women are affected (the sex ratio among patients in European countries is 3–4:1). The age of the patients ranges from 1 year to 80 years, the average age is about 40 years [6].
Causes
The cause of autoimmune hepatitis (in other words, the reason why the immune system attacks and destroys healthy liver cells) is still not clear. There is an assumption that inflammatory-necrotic liver damage may be associated with an imbalance of effector and regulatory T cells (cells of the immune system), and may arise as a result of adverse environmental influences or due to genetic predisposition.
Without appropriate treatment, the disease progresses and the following complications may develop: ascites (accumulation of fluid in the abdominal cavity), gastrointestinal bleeding due to impaired blood flow in the esophagus and stomach, cirrhosis of the liver (and liver cancer due to the increased risk associated with cirrhosis) , kidney failure.
Etiopathogenesis
The etiology of AIH is unknown, but the development of the disease is thought to be influenced by both genetic and environmental factors.
An important link in the pathogenesis may be certain alleles of the HLA II genes (human leukocyte antigen type II, Human leucocyte antigen II) and genes associated with the regulation of the immune system [7, 8].
It is worth mentioning separately about AIH, which is part of the clinical picture of autoimmune polyendocrine syndrome (autoimmune polyendocrine syndrome, autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy, APECED). This is a monogenic disease with autosomal recessive inheritance associated with a mutation in the AIRE1 gene. Thus, in this case, genetic determination is a proven fact [4, 9].
The autoimmune process in AIH is a T-cell immune response, accompanied by the formation of antibodies to autoantigens and inflammatory tissue damage.
Pathogenesis factors of AIH:
- pro-inflammatory factors (cytokines) produced by cells during the immune response. Indirect confirmation may be that autoimmune diseases are often associated with bacterial or viral infections;
- inhibition of the activity of regulatory T cells, which play a critical role in maintaining tolerance to autoantigens;
- dysregulation of apoptosis, normally a mechanism that controls the immune response and its “correctness”;
- molecular mimicry is a phenomenon where the immune response against external pathogens can also affect its own components that are structurally similar to them. Viral agents may play an important role in this. Thus, several studies have shown the presence of a pool of circulating autoantibodies (ANA, SMA, anti-LKM-1) in patients suffering from viral hepatitis B and C [2,4];
- factor of toxic drug effects on the liver. Some researchers associate the manifestation of AIH with the use of antifungal drugs and nonsteroidal anti-inflammatory drugs.
Clinic
In approximately a quarter of patients, AIH begins acutely, and even rare cases of acute liver failure have been described. Acute hepatitis with jaundice is more common in children and young people; in this same group, a fulminant course of the disease is more often observed [6].
It should be noted that some patients with symptoms of acute AIH in the absence of treatment may experience spontaneous improvement and normalization of laboratory parameters. However, a repeat episode of AIH usually occurs within a few months. Histologically, a persistent inflammatory process in the liver is also determined [6].
More often, the clinical picture of AIH corresponds to the clinical picture of chronic hepatitis and includes symptoms such as asthenia, nausea, vomiting, pain or discomfort in the right upper quadrant of the abdomen, jaundice, sometimes accompanied by skin itching, arthralgia, and less commonly, palmar erythema, telangiectasia, hepatomegaly [2, 6]. With developed liver cirrhosis, symptoms of portal hypertension and encephalopathy may prevail.
AIH can be associated with autoimmune diseases of various profiles:
- hematological (thrombocytopenic purpura, autoimmune hemolytic anemia);
- gastroenterological (inflammatory bowel diseases);
- rheumatological (rheumatoid arthritis, Sjogren's syndrome, systemic scleroderma);
- endocrine (autoimmune thyroiditis, diabetes mellitus);
and other profiles (erythema nodosum, proliferative glomerulonephritis) [1, 2].
Diagnosis of AIH
Diagnosis of autoimmune hepatitis is based on:
- research results: clinical, serological and immunological;
- excluding other liver diseases that occur with or without an autoimmune component (chronic viral hepatitis, toxic hepatitis, non-alcoholic steatosis, Wilson's disease, hemochromatosis, and cryptogenic hepatitis).
AIH types 1 and 3 are similar in terms of patient demographics, HLA profile, inflammatory activity, and response to therapy. AIH type 2 has significant differences, affecting more often children and adolescents and usually having an acute onset and a more severe course.
It is important to be aware of the possibility of AIH in patients with elevated liver enzyme levels, as well as in patients with liver cirrhosis. If there are signs of cholestasis, primary biliary cirrhosis and primary sclerosing cholangitis should be included in the range of pathologies for differential diagnosis.
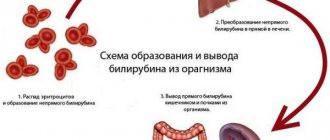
The clinical search includes the determination of such laboratory parameters as the activity of alanine aminotransferase and aspartate aminotransferase (ALT and AST), alkaline phosphatase (ALP), level of albumin, gamma globulin, IgG, bilirubin (bound and unbound). It is also necessary to determine the level of autoantibodies in the blood serum and obtain histological examination data [9].
For patients who failed to achieve remission and stop the development of cirrhosis within 4 years, the method of choice is liver transplantation. The 10-year survival rate in patients who have undergone this operation is quite high (75–85%), however, the rate of relapses reaches 11–41%. The persistence of autoantibodies in the blood is not a sign of relapse of AIH and does not predict its development.
Visual diagnostic methods (ultrasound, CT, MRI) do not make a decisive contribution to the diagnosis of AIH, however, they make it possible to establish the fact of progression of AIH and the outcome in cirrhosis of the liver, as well as exclude the presence of focal pathology. In general, diagnosis is based on 4 points [10]:
- Hypergammaglobulinemia is one of the most accessible tests. An increase in the level of IgG with normal levels of IgA and IgM is indicative. However, there are difficulties when working with patients with initially low IgG levels, as well as with patients (5–10%) with normal IgG levels in AIH. In general, this test is considered useful in monitoring disease activity during treatment [6].
- Presence of autoantibodies. At the same time, antibodies of the ANA and SMA types are not a specific sign of autoimmune hepatitis, nor are anti-LKM-1 antibodies, which are found in 1/3 of children and a small proportion of adults suffering from AIH. Only anti-SLA/LP antibodies are specific for AIH. Antibodies to double-stranded DNA can also be detected in patients.
- Histological changes are assessed in conjunction with previous indicators. There are no strictly pathognomonic signs of AIH, but many changes are quite typical. The portal fields are infiltrated to varying degrees by T lymphocytes and plasma cells. Inflammatory infiltrates are capable of “cutting off” and destroying individual hepatocytes, penetrating into the liver parenchyma - this phenomenon is described as stepwise (fine-focal necrosis), borderline hepatitis. Balloon degeneration of hepatocytes occurs inside the lobules with their swelling, formation of rosettes and necrosis of individual hepatocytes - Fig. 2. The fulminant course is often characterized by centrilobular necrosis. Bridge-like necrosis connecting adjacent periportal fields may also be observed [2, 6].
- Absence of markers of viral hepatitis.
- The International AIH Research Group has developed a scoring system to assess the reliability of the diagnosis - Table. 1.
Treatment of autoimmune hepatitis
AIH refers to diseases for which treatment can significantly increase patient survival.
Indications for starting treatment are:
- an increase in AST activity in the blood serum by 10 times compared to the norm or 5 times, but in combination with a twofold increase in the level of gamma globulin;
- the presence of bridge-like or multilobular necrosis during histological examination;
- pronounced clinic - general symptoms and symptoms of liver damage.
Less pronounced deviations in laboratory parameters in combination with a less pronounced clinical picture are a relative indication for treatment.
In case of inactive cirrhosis of the liver, the presence of signs of portal hypertension in the absence of signs of active hepatitis, and “mild” hepatitis with stepwise necrosis and without clinical manifestations, treatment is not indicated [1, 9]. The general concept of therapy for AIH involves achieving and maintaining remission. The basic immunosuppressive therapy is glucocorticosteroids (prednisolone) as monotherapy or in combination with azathioprine [2, 6, 9, 11]. Therapy continues until remission is achieved, and it is important to achieve histologically confirmed remission, which may lag behind the normalization of laboratory parameters by 6–12 months. Laboratory remission is described as normalization of the levels of AST, ALT, gamma globulin, IgG [2].
Maintenance therapy with lower doses of immunosuppressive drugs to reduce the likelihood of relapse after achieving remission is carried out for at least 2 years.
In addition, the possibility of using ursodeoxycholic acid (UDCA) drugs for autoimmune hepatitis as concomitant therapy or even monotherapy is being discussed [11]. AIH in patients receiving UDCA drugs in mono- and combination therapy was characterized by a milder course and accelerated normalization of laboratory parameters.
Symptoms
Symptoms of autoimmune hepatitis vary from person to person and may be mild or sudden in the early stages.
Symptoms of AIH include:
- increased fatigue, tiredness;
- discomfort and pain in the abdomen;
- skin rash, itching, formation of arachnoid angiomas;
- yellowness of the skin and visible mucous membranes (jaundice);
- joint pain;
- dark colored urine;
- amenorrhea (cessation of menstruation);
- hepatomegaly;
- splenomegaly.
Response to treatment
The results of treatment with prednisone and azathioprine for AIH may be as follows:
- A complete response is normalization of laboratory parameters, which persists for a year during maintenance therapy. At the same time, the histological picture is normalized (with the exception of small residual changes). The full effectiveness of treatment is also indicated in cases where the severity of clinical markers of autoimmune hepatitis significantly decreases, and during the first months of therapy laboratory parameters improve by at least 50% (and in the next 6 months they do not exceed the normal level by more than 2 times) .
- Partial response—there is an improvement in clinical symptoms and a 50% improvement in laboratory values within the first 2 months. Subsequently, the positive dynamics are maintained, but complete or almost complete normalization of laboratory parameters does not occur during the year.
- Lack of therapeutic effect (ineffectiveness of treatment) - an improvement in laboratory parameters by less than 50% in the first 4 weeks of treatment, and no further decrease (regardless of clinical or histological improvement) occurs.
- An unfavorable outcome of therapy is characterized by a further deterioration in the course of the disease (although in some cases there is an improvement in laboratory parameters).
Disease relapse is said to occur when, after achieving a complete response, clinical symptoms reappear and laboratory parameters deteriorate.
Typically, therapy has a good effect, but in 10–15% of patients it does not lead to improvement, although it is well tolerated. The reasons for the ineffectiveness of therapy can be [6]:
- lack of response to the drug;
- lack of compliance and adherence to therapy;
- drug intolerance;
- presence of cross syndromes;
- hepatocellular carcinoma.
Other immunosuppressants are also used as alternative drugs for the treatment of autoimmune hepatitis: budesonide, cyclosporine, cyclophosphamide, mycophenolate mofetil, tacrolimus, methotrexate [1, 2, 6, 11].
Clinical case
An eight-year-old girl was observed for skin rashes (erythematous and nodular elements without any discharge on the lower extremities) that had been bothering her for 5–6 months.
I used topical remedies for eczema for two months, there was no improvement. Later, discomfort in the epigastric region, weakness, and occasional nausea and vomiting arose. The rashes were localized on the legs. Histological examination of a skin biopsy revealed infiltration of subcutaneous fatty tissue with lymphocytes without signs of vasculitis. These phenomena were regarded as erythema nodosum. Upon examination, mild hepatosplenomegaly was revealed, otherwise the somatic status was without pronounced features, the condition was stable.
According to the results of laboratory tests:
- CBC: leukocytes - 4.5×109/l; neutrophils 39%, lymphocytes 55%; signs of hypochromic microcytic anemia (hemoglobin 103 g/l); platelets - 174,000/μl, ESR - 24 mm/h;
- biochemical blood test: creatinine - 0.9 mg/dl (normal 0.3–0.7 mg/dl); total bilirubin - 1.6 mg/dl (normal 0.2-1.2 mg/dl), direct bilirubin - 0.4 mg/dl (normal 0.05-0.2 mg/dl); AST - 348 U/l (normal - up to 40 U/l), ALT - 555 U/l (normal - up to 40 U/l); alkaline phosphatase - 395 U/l (normal - up to 664 U/l), lactate dehydrogenase - 612 U/l (normal - up to 576 U/l).
Indicators of the hemostasis system (prothrombin time, international normalized ratio), the level of total protein, serum albumin, gamma globulin, the level of ferritin, ceruloplasmin, alpha-antitrypsin, gamma-glutamyl transpeptidase are within the reference values.
No HBs antigen, antibodies to HBs, HBc, or antibodies to hepatitis A and C virus were detected in the blood serum. Tests for cytomegalovirus, Epstein-Barr virus, toxoplasma, and brucella were also negative. The ASL-O titer is within the normal range. There is no evidence for diabetes mellitus, thyroiditis, Graves' disease, proliferative glomerulonephritis.
Ultrasound of the abdominal organs visualized an enlarged liver with an altered echostructure, without signs of portal hypertension and ascites. Ophthalmological examination did not reveal the presence of a Kayser-Fleischer ring.
Anti-SMA antibody titer - 1:160, ANA, AMA, anti-LKM-1 antibodies were not detected. The patient is positive for haplotypes HLA DR3, HLA DR4.
Histological examination of the liver biopsy revealed fibrosis, lymphocytic infiltration, formation of hepatocyte rosettes and other signs of chronic autoimmune hepatitis.
The patient was diagnosed with autoimmune hepatitis type 1 associated with erythema nodosum, and therapy with prednisolone and azathioprine was started. The IAIHG score was 19 points before treatment, which is characterized as “definite AIH.”
After 4 weeks of therapy, relief of general clinical symptoms and normalization of laboratory parameters were noted. After 3 months of therapy, the skin rashes completely regressed. 6 months after the end of therapy, the patient’s condition was satisfactory, laboratory parameters were within the reference values.
Adapted from Kavehmanesh Z. et al. Pediatric Autoimmune Hepatitis in a Patient Who Presented With Erythema Nodosum: A Case Report. Hepatitis monthly, 2012. V. 12. - N. 1. - P. 42–45.
Thus, AIH is a fairly rare and relatively treatable disease. With the introduction of modern immunosuppressive therapy protocols, the 10-year survival rate of patients reaches 90%. The prognosis is less favorable in patients with autoimmune hepatitis type 2, especially in children and adolescents, in whom AIH progresses much faster, and the effectiveness of therapy is generally lower. You should also be aware of the risk of developing hepatocellular carcinoma (4–7% within 5 years after diagnosis of liver cirrhosis).
List of sources
- Viral hepatitis and cholestatic diseases / Eugene R. Schiff, Michael F. Sorrell, Willis S. Maddray; lane from English V. Yu. Khalatova; edited by V. T. Ivashkina, E. A. Klimova, I. G. Nikitina, E. N. Shirokova. - M.: GEOTAR-Media, 2010.
- Kriese S., Heneghan MA Autoimmune hepatitis. Medicine, 2011. V. 39. - N. 10. - P. 580–584.
- Autoimmune hepatitis and its variant forms: classification, diagnosis, clinical manifestations and new treatment options: a manual for doctors. T. N. Lopatkina. - M. 4TE Art, 2011.
- Longhia MS et al. Aethiopathogenesis of autoimmune hepatitis. Journal of Autoimmunity, 2010. N. 34. - P. 7–14.
- Muratori L. et al. Current topics in autoimmune hepatitis. Digestive and Liver Disease, 2010. N. 42. - P. 757–764.
- Lohse AW, Mieli-Vergani G. Autoimmune hepatitis. Journal of Hepatology, 2011. V. 55. - N. 1. - P. 171–182.
- Oliveira LC et al. Autoimmune hepatitis, HLA and extended haplotypes. Autoimmunity Reviews, 2011. V. 10. - N. 4. - P. 189–193.
- Agarwal, K. et al. Cytotoxic T lymphocyte antigen-4 (CTLA-4) gene polymorphisms and susceptibility to type 1 autoimmunehepatitis. Hepatology, 2000. V. 31. - N. 1. - P. 49–53.
- Manns MP et al. Diagnosis and Management of Autoimmune Hepatitis. Hepatology, 2010. V. 51. - N. 6. - P. 2193–2213.
- Lohse AW, Wiegard C. Diagnostic criteria for autoimmune hepatitis. Best Practice & Research Clinical Gastroenterology, 2011. V. 25. - N. 6. - P. 665–671.
- Strassburg CP, Manns MP Therapy of autoimmune hepatitis. Best Practice & Research Clinical Gastroenterology, 2011. V. 25. - N. 6. - P. 673–687.
- Ohira H., Takahashi A. Current trends in the diagnosis and treatment of autoimmune hepatitis in Japan. Hepatology Research, 2012. V. 42. - N. 2. - P. 131–138.
Possibilities of echography in the diagnosis of autoimmune hepatitis in children
Ultrasound scanner RS80
A benchmark for new standards!
Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of advanced ultrasound technologies to solve the most challenging diagnostic problems.
Introduction
Currently, due to the development of high-resolution ultrasound diagnostic equipment, interest in the capabilities of echography in the differential diagnosis of diffuse liver diseases is significantly increasing. The works of a number of authors [l,2] present echo and Doppler criteria for assessing the liver in viral hepatitis and cirrhosis of the liver. However, in Russia, autoimmune hepatitis accounts for 2% of the structure of chronic hepatitis in children, which is a significant amount and attracts the active attention of hepatologists [3].
Autoimmune hepatitis is a progressive hepatocellular inflammation of unknown etiology, characterized by the presence of periportal hepatitis, hypergammaglobulinemia, liver-associated serum autoantibodies and a positive response to immunosuppressive therapy [4]. Girls and women make up 75% of patients [5]. The etiology of autoimmune hepatitis is unknown, and the pathogenesis is not well understood. The role of Epstein-Barr viruses, hepatitis A and C, as well as drugs is discussed as possible triggering factors for the onset of the disease. The possibility of the occurrence of autoimmune hepatitis due to a primarily caused disorder of the immune response cannot be excluded, when the appearance of “forbidden clones” of autoreactive cells occurs without the influence of trigger factors [6]. Mandatory for the diagnosis of autoimmune hepatitis is the presence of autoantibodies in the blood serum: antinuclear (ANA) and/or anti-smooth muscle (SMA) antibodies in autoimmune hepatitis type I; autoantibodies to liver and kidney microsomes (anti-LKM I) in autoimmune hepatitis type II, hypergammaglobulinemia, as well as the absence of signs of viral and metabolic liver diseases [7]. As a result of autoimmune hepatitis, liver cirrhosis often develops in a relatively short time after the first manifestation of the process. In children, liver cirrhosis occurs in 74% of cases with autoimmune hepatitis type I and in 44% of cases with autoimmune hepatitis type II [5]. In adults, the situation is the opposite: with autoimmune hepatitis type II, liver cirrhosis develops more often than with autoimmune hepatitis type I (82% versus 43%, respectively) [6].
Considering the relevance of the problem and the lack of data in the available literature on the capabilities of ultrasound diagnostics in recognizing autoimmune hepatitis, the purpose of the work was to determine echographic changes in the liver in autoimmune hepatitis in children.
Materials and methods
We observed 36 children (31 girls and 5 boys) aged 7 to 15 years with a diagnosis of autoimmune hepatitis. The average follow-up duration was 31.4±19.8 months. At the time of admission, the duration of the disease ranged from 1 month to 8 years.
All children underwent a laboratory examination, including a general blood test, a biochemical blood test, determination of the content of immunoglobulins (Ig) classes A, M, G, markers of viral hepatitis A, B, C (anti-HAV IgM, HbsAg, anti-HBc, anti -HBe, anti-HBs, anti-HCV) by ELISA, hepatitis B virus DNA and hepatitis C virus RNA by polymerase chain reaction (PCR). Disorders of pigment metabolism, signs of cytolysis and changes in immunological activity were identified. 33 patients (91.7%) were diagnosed with autoimmune hepatitis type I, characterized by the presence of ANA and SMA, but the absence of anti-LKM I in the blood serum, and in 3 (8.3%) children - autoimmune hepatitis type II.
Liver puncture biopsy was performed in 27 of 36 patients. Morphological examination of liver tissue indicated the presence of chronic hepatitis in 8 patients; signs of liver cirrhosis were identified in 19 patients. In 9 patients, due to refusal to perform a puncture biopsy of the liver, the formation of liver cirrhosis was established on the basis of clinical and laboratory data. Thus, 28 of 36 children with autoimmune hepatitis had liver cirrhosis. An endoscopic examination upon admission to the clinic revealed grade 12 varicose veins of the esophagus in 19 patients with liver cirrhosis and in another 6 patients 1-1.5 years after the start of observation.
The control group consisted of 25 healthy peers. As a comparison group, 56 children with viral hepatitis B and 42 children with viral hepatitis C aged 7 to 15 years were examined. All patients underwent ultrasound examination of the abdominal organs and retroperitoneal space. Sensors with a frequency of 3.5-5.0 MHz were used. A generally accepted technique for echographic assessment of the liver and blood flow in color and pulse modes was performed. The liver examination included measurement of the left lobe (antero-posterior, medial-lateral and superior-inferior dimensions), the right lobe (superior-inferior dimension).
Doppler examination of the vessels of the portal system and the celiac trunk was carried out along the portal vein - in the area of the trunk, along the hepatic and splenic arteries - at the point of their exit from the celiac trunk, along the splenic vein - in the area of the hilum of the spleen, along the middle hepatic vein - retreating 2-3 cm from the place of its confluence with the inferior vena cava. The main criteria for assessing blood flow were indicators of volumetric blood flow, resistance index in the arteries and pulse index in the hepatic vein. The results obtained were processed statistically using generally accepted methods of variation statistics. The reliability of the differences in the studied indicators was determined using the Student's test.
Research results
All children with autoimmune hepatitis at the stage of chronic hepatitis had diffuse enlargement of the liver. There was no clear dependence on the activity of the process or the duration of the disease. The increase in the right lobe averaged 20%, and the left lobe - 8% in the superior-inferior and 20% in the medial-lateral dimensions compared with normal age-related indicators. The contour of the liver was smooth, but with pronounced lobulation. The angles of the lobes corresponded to the normal contour of the liver. Hyperechogenicity of the parenchyma was noted. Its heterogeneity was due to hyper- and hypoechoic areas of medium size (3-5 mm), hyperechoic heaviness along the branches of the portal vein, which created the impression of a reticulated hepatic pattern (Fig. 1 a). Single hepatic veins were visualized with a small extent from the point of confluence with the inferior venous vein, thin, horizontally directed, with an even contour (oblique section of the liver). No ultrasound attenuation was observed, and the liver parenchyma was well traced to the posterior contour. The diameter of the portal vein trunk remained within acceptable values. There was hyperechogenicity of the walls of both the trunk and small branches of the portal vein. One child had a small opening of the umbilical vein (up to 2 mm) without signs of blood flow in it.
Rice. 1.
Echograms of the liver in autoimmune hepatitis at different stages.
A)
For chronic hepatitis.
b)
For cirrhosis of the liver.
V)
With viral hepatitis C.
No changes in the size of the spleen, its parenchyma and the trunk of the splenic vein were observed. There were no sonographic signs of portal hypertension in this group of patients.
According to Doppler ultrasound data (Table 1), there was an increase in volumetric blood flow through the portal vein due to an increase in its speed. The diameter of the vessel was within the normal range. Two-phase blood flow was determined through the middle hepatic vein, in contrast to three-phase blood flow in healthy children. In 2 patients, the Doppler curve was linear. There was a trend toward an increase in the hepatic artery blood flow resistance index. Blood flow through the vessels of the spleen was practically no different from that in children from the control group.
Table 1.
Indicators of hemodynamics of portal blood flow in children with autoimmune hepatitis (M±m).
| Vessel | Control group (n = 25) | Autoimmune hepatitis | ||||
Chronic hepatitis (n =  | Liver cirrhosis (n = 28) | |||||
| Q | IR | Q | IR | Q | IR | |
| Portal vein | 0,47±0,02 | 0,59±0,03* | 0,76±0,05* | |||
| Hepatic artery | 0,73±0,03 | 0,78±0,04 | 0,81±0,06* | |||
| Splenic vein | 0,39±0,02 | 0,41±0,05 | 0,50±0,02* | |||
| Splenic artery | 0,59±0,02 | 0,70±0,04 | 0,75±0,04* | |||
Q - volumetric blood flow in l/min; IR—resistance index. * Significant differences compared to the control group (p
Ultrasound of patients with cirrhosis of the liver as a result of autoimmune hepatitis revealed an increase in the right lobe by 30-40%, the left lobe by 10-20% in the upper-inferior and by 40% in the medial-lateral dimensions compared with the age norm, and remained so until the onset of signs of decompensation of the process. In half of the children, the liver contour was uneven or clearly lumpy; corners are rounded. There was an increase in the echogenicity of the parenchyma. The echostructure of the liver was heterogeneous due to nodes of various sizes and numbers, with a clear contour, homogeneous in structure, often isoechoic, less often - moderately hypoechoic without clear localization. So-called “radial clefts” were also observed, which were visualized as hypoechoic strands throughout the liver parenchyma, vertically directed with an uneven contour (Fig. 1b). In 18% of patients, ultrasound weakened by 1/4-1/3 in anteroposterior dimension. The vascular pattern was depleted. Single hepatic veins were visualized, vertically directed, with a convoluted contour. Ultrasound signs of portal hypertension came to the fore. The portal vein trunk was dilated to 10-14 mm. Hyperechoic strands were noted along the trunk of the portal vein and its dilated branches, as well as along the intersegmental septa. There were multiple additional branches of the portal vein, recanalization of the umbilical vein with blood flow through it. The spleen was significantly enlarged: in 13 children by 15%, in 10 children by 20-25% and 5 children by 30-40% compared to the age norm. Its parenchyma was heterogeneous, hyperechoic with many intraorgan branches and anastomoses between the splenic artery and vein in the hilum area. The trunk of the splenic vein was dilated to 8-14 mm and tortuous.
Doppler examination revealed a decrease in blood flow velocity through the portal and splenic veins. However, due to the significant expansion of the diameter of these vessels, the volumetric blood flow was increased. The resistance index in the hepatic and splenic arteries increased (see table). In all patients with liver cirrhosis, the linear nature of blood flow through the middle hepatic vein was determined.
In patients with autoimmune hepatitis, various deformations of the gallbladder (kinks in the fundus or body) and an increase in its size were detected with the same frequency both in chronic hepatitis and in cirrhosis of the liver. Consolidation or slight thickening of the bladder walls (up to 2 mm) was typical for patients with chronic hepatitis, while in patients with liver cirrhosis, more significant thickening up to (2-4 mm) often occurred. In 9 children, varicose veins of the gallbladder walls were determined (one of the signs of portal hypertension), which was combined with varicose veins of the esophagus and vasculopathy of the gastric mucosa according to endoscopic examination.
Changes in the pancreas were more often of the nature of reactive changes, which was manifested either by a diffuse increase in the entire gland, or an increase in any of its parts (head or tail), without changes in the parenchyma. In this case, multiple linear parallel hyperechoic signals were noted, more often in the area of the tail or head of the gland, which was regarded as thickening of the vascular walls. The Wirsung duct was visualized mainly in the area of the gland body and was within normal age values (1-2 mm). In 8 children (28%) with liver cirrhosis, diffuse enlargement of the pancreas was combined with a decrease in the echogenicity of its parenchyma, that is, there were ultrasound signs of pancreatitis.
Upon admission to the clinic, all children were prescribed immunosuppressive therapy (prednisolone and azathioprine). Repeated ultrasounds showed that, mainly during therapy, there was a slight decrease in the size of both the liver and spleen, as well as the diameters of the portal and splenic veins. The structure and echogenicity of the liver parenchyma did not change. There was a trend towards a decrease in volumetric blood flow in the portal vein and a decrease in the resistance index in the hepatic artery.
In 9 children with liver cirrhosis, as a result of autoimmune hepatitis, signs of decompensation of the process were revealed (severe portal hypertension, the threat of bleeding from esophageal varices, hepatic encephalopathy), which necessitated the need to raise the question of performing orthotopic liver transplantation in them.
Discussion
An ultrasound often begins the examination of a child if liver disease is suspected, so the question arises about the primary differential diagnosis of liver disease. Hyperechogenicity and heterogeneity of its parenchyma in the absence of signs of portal hypertension build a differential series, in the first place in which are viral and then metabolic liver diseases.
The echographic picture of the liver parenchyma in patients with autoimmune hepatitis at the stage of chronic hepatitis was characterized by heterogeneity due to hyper- and hypoechoic areas of medium size, hyperechoic heaviness along the branches of the portal vein and depletion of the vascular pattern. This picture differed from the finely diffuse heterogeneous liver parenchyma observed with hepatitis B and C in the comparison group. Differences were also revealed in the characteristics of the vascular bed: an abundance of hepatic veins with an even contour, horizontally directed, traced throughout the entire section of the liver parenchyma. There was no pronounced hyperechoic heaviness along the branches of the portal vein (Fig. 1c). Sometimes parallel linear signals of average echogenicity were noted along the small branches of the portal vein, but, as a rule, this was combined with an enlargement of the gallbladder, its deformations and a decrease in contractile function. The combination of these signs was regarded as biliary dyskinesia with symptoms of cholestasis.
In the area of the porta hepatis, in 80% of patients with viral hepatitis B and C, one or two oval-shaped lymph nodes with a clear, even contour, hypoechoic and homogeneous in structure were visualized. Their size was in the range of 8 x 5 - 10 x 5 mm. This symptom has never been recorded in autoimmune hepatitis.
There were no significant differences in portal blood flow hemodynamics in patients with viral hepatitis and autoimmune hepatitis. There was only a tendency to increase the resistance index in the hepatic artery in children with autoimmune hepatitis.
Thus, a comprehensive ultrasound of the liver in children with autoimmune hepatitis reveals characteristic diagnostic signs that can be used in differential diagnosis with other diffuse liver diseases.
Literature
- Abbas N.M. The state of central and peripheral hemodynamics in children with chronic liver diseases: Dis. ...cand. honey. Sci. M., 1996. 160 p.
- Mitkov V.V. Quantitative ultrasound assessment of splanchnic hemodynamics in non-tumor diseases of the hepatobilipancreatic zone: Dis. ...Dr. med. Sci. M., 2001. 278 p.
- Terminology of Chronic Hepatitis. International Working Party Report //Am. J. Gastroenterol. 1995. Vol. 90, N 2. R. 181-189.
- Nisevich N.I., Uchaikin V.F. The evolution of infectious diseases of children in the 20th century and problems of the 21st century / Medical Forum. 1999. N 1 (13). C. 17-20.
- Autoimmune hepatitis in childhood: 20-Year Experience / GVGregorio, B. Portmann, F. Reid et al. // Hepatology. 1997. Vol. 25. P. 541547.
- Czaja AJ Autoimmune hepatitis. Evolving concepts and treatment strategies // Dig. Dis. Sci. 1995. Vol. 40. R.435-456.
- International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis // Hepatol. 1999. Vol. 31. P. 929-938.
Ultrasound scanner RS80
A benchmark for new standards!
Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of advanced ultrasound technologies to solve the most challenging diagnostic problems.
« previous article
next article »