Causes of pneumonia
Viruses or bacteria are responsible for most cases of pneumonia (in children and adolescents, the infection is often caused by mycoplasma). The disease is also common in people suffering from gastroesophageal reflux. Inflammatory exudate occurs when food enters the lungs. Pneumonia can also be a complication of an upper respiratory tract infection or other infectious disease. Pneumonia can also be caused by fungi (candied pneumonia) and inhalation of allergic or chemical substances.
Features of community-acquired pneumonia
Determining the pathogen is often a difficult task due to the difficulties in obtaining a substrate for diagnostics and often the lack of sufficient time for additional diagnostics. In addition, patients often develop a mixed infection.
The most common causative agent of bacterial infection (30–50% of cases) is the pneumococcus Streptococcus pneumoniae. The so-called atypical strains, undetectable by bacterioscopy and culture on conventional nutrient media, account for up to 30% of cases of the disease (Chlamydophila pneumoniae, Mycoplasma pneumoniae, Legionella pneumophila). 3–5% of cases of bacterial pneumonia are associated with rare pathogens (Haemophilus influenzae, Staphylococcus aureus, Klebsiella pneumoniae, other enterobacteria). Extremely rarely, community-acquired pneumonia can be caused by Pseudomonas aeruginosa (in the presence of bronchiectasis or in patients with cystic fibrosis).
Viral forms of CAP are caused by respiratory viruses: influenza virus, coronaviruses, rhinosyncytial virus, human metapneumovirus, human bocavirus. In most cases, respiratory viruses cause mild pneumonia with a self-limiting nature, however, in elderly and senile people, in the presence of concomitant bronchopulmonary, cardiovascular diseases or secondary immunodeficiency, the development of severe, life-threatening complications is possible.
Secondary bacterial pneumonia can be a complication of a primary viral infection of the lungs or an independent late complication of influenza.
Who gets pneumonia more often?
There are factors that increase your chance of getting pneumonia. These include viral respiratory tract infections, congenital respiratory defects, old age, heart failure, diabetes and immunological problems.
The following groups of people are at high risk of developing pneumonia:
- people suffering from allergies;
- malnourished people;
- people who smoke or are exposed to tobacco smoke;
- people with weakened immune systems;
- people with congenital defects of the respiratory and circulatory systems.
Viral pneumonia COVID-19
All known coronaviruses are characterized by rapid (up to 14 days) development of acute respiratory failure. The virus quickly and aggressively infects the lungs, causing not only extensive inflammation, but also associated complications: swelling of the respiratory organ, fibrosis (scarring of the lungs), acute heart failure, myocarditis.
The first coronavirus type B (SARS-CoV) was reported in 2002 and its primary hosts are believed to be horseshoe bats. In 2012, the world was gripped by an epidemic of coronavirus type C MERS-CoV (Middle East respiratory syndrome). Finally, in 2019, there was an outbreak of the new coronavirus type B COVID-19 (or SARS-Cov2). What they have in common is that new viruses are stable, easily attach to the lung parenchyma with protein spikes, and in a short time provoke extensive acute inflammation. The fatality rate is about 10%.
However, pneumonia is not always the cause of death from these viruses. For example, if the patient's medical history is complicated by atherosclerosis or myocarditis, the virus primarily affects the cardiovascular system. In general, the coronavirus family includes about 46 types of virions.
Read more about pneumonia associated with COVID-19 in our articleWhat does a CT scan of the lungs show for coronavirus?
Types of pneumonia
Doctors divide pneumonia into:
- bacterial;
- fungal;
- viral (often found in children over 5 years of age);
- allergic;
- chemical;
- typical;
- atypical;
- Also worth mentioning is an idiopathic pneumonia called idiopathic interstitial pneumonia. In this case, inflammation turns into fibrosis. Each type of pneumonia occurs differently. In some cases, the disease is asymptomatic, then we are talking about asymptomatic pneumonia.
Another division of pneumonia is distinguished:
- lobar pneumonia (includes one lobe and pleura);
- bronchopneumonia (germs penetrate the bronchi);
- segmental pneumonia.
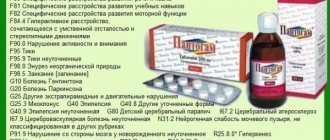
Pneumonia according to ICD-10 classification
In the International Statistical Classification of Diseases and Related Health Problems (ICD-10), pneumonia is designated J12-J18.
- J12 - previously unclassified pneumonia, most often of viral origin;
- J13 - pneumonia caused by streptococci;
- J14 - pneumonia as a result of infection with bacteria H. influenzae;
- J15 - previously unclassified bacterial pneumonia;
- J16 - pneumonia caused by microorganisms not recommended by other types;
- J17 - pneumonia in previously classified diseases;
- J18 - pneumonia caused by unspecified microorganisms.
Symptoms of pneumonia
The symptoms that precede pneumonia are similar to those of other respiratory diseases, so influenza may be diagnosed initially. However, symptoms vary greatly in severity.
The main and most common symptoms of pneumonia:
- fever and chills;
- chest pain;
- labored breathing;
- wheezing;
- cough;
- coughing up mucus;
- muscle pain;
- weakness;
- feeling overwhelmed and weak.
However, depending on the type of pneumonia, symptoms may vary. Thus, with atypical pneumonia, vomiting and diarrhea are also observed, and with bacterial pneumonia, a runny nose usually appears first. Any signs of pneumonia should not be underestimated and consult a doctor as soon as possible. Pneumonia in children has symptoms similar to those in adults, but is usually much more severe.
Viral pneumonia - symptoms and treatment
With influenza , the disease begins acutely: with chills and a sharp rise in temperature to 39-40°C. Muscle, joint and headaches are typical. The typical appearance of the patient is redness of the face, oral mucosa and conjunctiva (white) of the eyes. There is a dry cough and a slight runny nose.
Pneumonia against the background of this infection can develop within a few days, and in the meantime the patient even gets better. Worsening will be indicated by blueness of the skin (cyanosis), increased shortness of breath and a cough that becomes annoying. Sometimes hemoptysis and suffocation are observed, chest pain occurs, and blood pressure decreases [5].
The adenovirus is characterized by an acute onset with high fever, damage to the eyes, nasal mucosa, larynx and pharynx (conjunctivitis and rhinotonsillopharyngitis). All parts of the respiratory system are consistently affected, primarily the nasal mucosa: prolonged rhinitis is observed (up to 4 weeks) with the impossibility of nasal breathing. Also characteristic are redness and pain in the eyes, watery eyes, photophobia, redness and pain when blinking and closing the eyes. The patient is bothered by the feeling of “sand” and pain in the throat when swallowing, sore throat often occurs, the cervical lymph nodes are enlarged, diarrhea and abdominal pain are possible. Associated adenoviral pneumonia is characterized by increasing intoxication, fever, shortness of breath and wet cough [6].
With parainfluenza , symptoms of a runny nose are pronounced; laryngitis is typical - damage to the trachea, which is manifested by hoarseness and a dry, rough cough. A common complication of this condition is pneumonia. With its early onset - on the 3-4th day of illness - a severe course is noted with high fever and severe intoxication (chest pain, shortness of breath, chills, etc.).
Rhinosyncytial infection causes pneumonia in every 6th child under 4-5 years of age; half of the children have an asthmatic reaction. With rhinosyncytial pneumonia, the deterioration of the condition begins with rhinopharyngitis (inflammation of the nose and pharynx). On the 2-3rd day, severe shortness of breath and cough appear, dry or with scanty sputum, which becomes annoying, with wheezing. Body temperature rises, often accompanied by inflammation of the middle ear - otitis media.
It is important that rhinosyncytial virus has an immunosuppressive effect. This creates the preconditions for chronic disease, the formation of asthma in children and repeated episodes of the disease in older people [7].
Due to the widespread practice of refusing vaccination, there are frequent cases of measles infection , as well as its complications, including pneumonia. Conjunctivitis and a rough cough are typical for measles. Against the background of high fever (up to 39°C), a rash appears on days 2-3. First, rashes appear in the mouth - whitish spots with a reddish rim (they are called Belsky-Filatov-Koplik spots). On days 3-4, the rash on the buccal mucosa gives way to rashes on the skin of the body.
A distinctive feature of measles rashes is their staged nature: first they appear on the face, on another day on the body, on the third on the legs and feet. The elements of the rash merge with each other. Their extinction occurs in the same order as their appearance.
In unvaccinated patients, measles is severe; bloody rashes and a painful cough with difficulty breathing may appear.
Pneumonia with measles can occur even before the rash appears. It is manifested by shortness of breath, severe intoxication, and sometimes hemoptysis. This type of primary viral pneumonia is a serious disease.
Secondary bacterial pneumonia with measles can develop on the 7-10th day of illness. It is accompanied by a cough with shortness of breath and purulent sputum.
Coronavirus infection often begins gradually, with a low temperature (up to 37.5°C), sore throat and minor conjunctivitis. On the 8th-9th day of illness, viral pneumonia may develop with the appearance of severe shortness of breath, chest pain and dry cough.
Sometimes fever occurs in the first days of illness, and on days 5-6 lung damage occurs. Some patients experience gastrointestinal dysfunction, accompanied by diarrhea, nausea and vomiting. According to modern research, such symptoms are observed in less severe cases of the disease [8].
If the disease progresses, some patients develop acute respiratory distress syndrome (usually on days 3-5 of the disease, but can also occur on days 2). It is characterized by very high temperature, low blood pressure, tachycardia and progression of respiratory failure.
On X-rays and computed tomography of the lungs, changes in the lungs caused by the virus are observed: signs of bilateral damage, rounded darkening, merging with each other and resembling frosted glass. After suffering from coronavirus pneumonia, massive fibrous scars form in necrotic (dead) areas of the lungs.
The disease is also characterized by damage to the vascular wall with impaired blood clotting, which results in the occurrence of thrombosis and thromboembolism.
The duration of viral pneumonia depends on the virus that caused it, the severity of the disease and its complications. On average, it ranges from 10-14 days to 4-6 weeks.
Hantavirus pneumonia , or hantavirus cardiopulmonary syndrome, is caused by a group of similar hantaviruses. Transmitted to humans from rodents. In Russia, a similar disease is called hemorrhagic fever with renal syndrome.
Today, outbreaks of hantavirus pneumonia are being detected [9]. The initial symptoms are no different from any ARVI: muscle pain, fever, weakness. However, quickly (after 2-3 days) a severe cough and shortness of breath develop, turning into suffocation.
Considering all the listed signs of viral infections, we can highlight the main symptoms of viral pneumonia :
- cough - first dry, then wet, can be purulent, with sputum difficult to separate;
- shortness of breath - it can be so severe that the muscles of the back, abdomen and neck are involved in the breathing process;
- pain in the chest - often occurs when the pleura (the membrane that covers the lungs) is involved in the process; pain can intensify during movement and coughing;
- heat;
- severe weakness, sweating (especially night sweating).
In children, pneumonia can occur with severe intoxication, fever, lethargy and loss of appetite.
IMPORTANT: do not forget about the abortive, hidden course of pneumonia. It is characterized by scanty symptoms, low fever and a slight cough. Only laboratory diagnostic methods and chest radiography can detect the disease.
Diagnosis of pneumonia
Pneumonia is not easy to diagnose. Lung noises may not be heard even by the most qualified doctors. In this case, it is worth taking a chest x-ray to assess the degree of inflammation. The doctor also diagnoses the disease after conducting a blood test (complete blood count, PCT, ESR and CRP).
Respiratory cultures for microbiological tests and blood cultures are also performed to diagnose pneumonia. Inpatients are also prescribed computed tomography and bronchoscopy.
Treatment of pneumonia
Pneumonia, diagnosed at an early stage, is easily treatable. Doctors usually prescribe drugs that help cough up secretions, antipyretics, and strong antibiotics.
A person with typical pneumonia recovers in 7–10 days. Bacterial pneumonia lasts longer - up to 21 days. In addition to taking medications, it is also important to drink plenty of water. With pneumonia (when the patient does not have a fever), there is no need to lie in bed. Doctors even recommend doing sports, especially outdoors. Medicines are prescribed to improve ventilation and remove residual secretions.
In some cases, a doctor may refer a person with pneumonia to the hospital. In severe cases of the disease, the child requires hospitalization. The hospital prescribes intravenous antibiotic therapy. Fortunately, these are not common cases.
Aspiration pneumonia
Aspiration pneumonia was first described by Hippocrates, and until the 19th century it was called “chest disease,” which was accompanied by fever. For palliative patients, aspiration pneumonia is a terrible diagnosis. It kills up to 40% of patients. But fortunately, aspiration pneumonia is preventable.
Interestingly, aspiration of nasopharyngeal contents often occurs in healthy people, for example, at night. But this does not always cause pneumonia, including in palliative patients.
This happens because for the development of aspiration pneumonia certain conditions must exist:
- Pathological nature of the aspiration material (increased acidity, decreased acidity while taking H2 blockers and proton pump inhibitors, a large number of microorganisms and their virulence);
- Large volume and special nature of the aspirated material (more than 25 ml, large particles in the aspirate);
- Reduced factors of local respiratory tract protection.
Important
The diagnosis of “aspiration pneumonia” is made when there is an episode of massive aspiration documented by a bronchoscopy protocol, as well as in patients with risk factors for the development of aspiration.
Aspiration pneumonia does not always have a fulminant course. The rate of its development and the variability of clinical manifestations depend on the nature of the material aspirated into the respiratory tract.
The main consequences that develop in patients against the background of aspiration pneumonia:
- Mechanical obstruction of the airways;
- Chemical (aspiration) pneumonitis: non-infectious lung damage associated with the “direct” action of gastric juice;
- Bacterial pneumonia.
Complications of aspiration pneumonia:
- Necrotizing pneumonia. Formation of foci of destruction less than 1 cm in size, without fluid levels;
- Lung abscess. Single or multiple cavities larger than 2 cm;
- Empyema of the pleura.
Features of the treatment of aspiration pneumonia:
- The recommended duration of therapy without infectious complications is 14 days;
- Parenteral administration of antibacterial drugs is preferable;
- In the presence of purulent complications, fever persists for a long time (5-10 days), despite adequately selected empirical antibacterial therapy;
- Efficiency assessment should be carried out not after 72 hours, but later - on days 5-10. Therapy continues throughout this time;
- When a clinical effect is achieved, transfer to oral forms is possible (step therapy).
Methods for assessing dysphagia and preventing aspiration in palliative patients. What nuances should be taken into account when conducting the “three sips test” in palliative patients, what are the predictors of dysphagia, how to assess and prevent the risk of aspiration
Varvara Brusnitsyna
Symptomatic treatment
Prevention of aspiration pneumonia
- Minimize the “lying on your back” position;
- Change body position more often, give the patient a semi-sitting position;
- Planned rather than emergency gastrostomy (for dysphagia): the moment of gastrostomy placement is determined individually;
- Correction of sedative therapy if it leads to impaired consciousness;
- Careful oral hygiene;
- Compliance with feeding rules in patients with dysphagia:
- The head of the bed should be raised 45 degrees when feeding;
- Slow, drip administration of the mixture, rather than a bolus;
- Compliance with the rules of care when a nasogastric tube is installed.
Important What needs to be taught to relatives of patients with dysphagia:
- Follow feeding rules;
- Monitor the position of the person’s body in bed during eating and sleeping;
- Carry out oral hygiene regularly and thoroughly;
- Monitor swallowing function, pay attention to choking, difficulty swallowing, and promptly contact medical personnel.
Clinical example 1
From the anamnesis:
A 54-year-old woman has been suffering from multiple sclerosis for about 20 years with gradual progression of the disease - with limitation of motor activity, loss of self-care skills, increasing cognitive impairment, decreased self-criticism, and the appearance of dysphagia over the last year.
December 2022 - hospitalization for symptomatic therapy. The patient is fed by medical staff and relatives.
Before planned discharge, there was a progressive deterioration of the patient’s condition with an increase in respiratory symptoms, low-grade fever.
Prescription of antibacterial therapy (3rd generation cephalosporin). Increasing respiratory failure, febrile fever, pulmonary edema. Calling the resuscitation team, intubation, transfer to the intensive care unit of City Clinical Hospital No. 40.
Upon admission to the hospital of City Clinical Hospital No. 40, the condition was extremely severe, depression of consciousness to the point of coma, respiratory failure, intoxication, increasing neurological deficit.
In the hospital, the patient underwent fiberoptic bronchoscopy, purulent endotracheobronchitis of the 2nd degree was detected, the tracheobronchial tree was sanitized and food masses were aspirated. X-ray examination and CT scan of the chest revealed bilateral pneumonia: lower lobe pneumonia on the right, polysegmental pneumonia on the left, and minimal right-sided hydrothorax.
Complete blood count Leukocytes 20 x10⁹, neutrophil shift 85%
Treatment
- Sanitation bronchoscopy;
- Antibacterial therapy (meropenem, vancomycin);
- Anticoagulant therapy.
Features of the clinical case
- Rapid development of severe pneumonia with pulmonary edema;
- Clinical and radiological resolution of severe bilateral aspiration pneumonia in a short time;
- No purulent complications.
In February 2022, a planned gastrostomy was performed
. The patient continues to be monitored by the palliative care service.
Conclusions:
- The rules of feeding a patient with dysphagia were violated;
- The doctor on duty made the right decision to call the resuscitation team and urgently transfer the patient with a good life prognosis to the intensive care unit of a multidisciplinary hospital;
- The resuscitation team and the doctor on duty provided emergency medical care in a timely manner;
- Adequate initial empirical antibacterial therapy was prescribed.
It is necessary to discuss the issue of timely gastrostomy placement with the patient and his relatives as early as possible!
Clinical example 2
From the anamnesis:
Male 45 years old . He has been suffering from multiple sclerosis for about 15 years with gradual progression of the disease and disability.
From 2022 - complete loss of self-care skills , weight loss, increase in cognitive impairment.
In October 2022, difficulties appeared when swallowing solid food, frequent choking, and periodic coughing.
On November 25, 2022, he was hospitalized at the Palliative Care Center of the Moscow Health Department, and already on the third day there was an episode of aspiration while eating.
On November 29, one day after the episode of aspiration, negative dynamics with the appearance of respiratory symptoms, shortness of breath, hyperthermia, intoxication symptoms, a decrease in saturation to 88% and hypotension.
An X-ray examination of the chest organs revealed polysegmental pneumonia in the lower lobe of the right lung.
A clinical blood test revealed leukocytosis with a neutrophil shift and an increase in ESR.
A diagnosis of aspiration pneumonia was made.
Treatment
- Initial empirical antibacterial therapy (cefepime + metronidazole);
- Mucolytics;
- Oxygen therapy;
- The OVD diet is pureed with strict adherence to the rules of feeding patients with dysphagia;
Conversation with relatives about compliance with feeding rules and planned gastrostomy.
Features of this clinical case
- Rapid development of pneumonia with severe intoxication syndrome and respiratory failure;
- Persistence of fever (6 days) with positive clinical dynamics during antibacterial therapy;
- Without purulent complications;
- The duration of antibacterial therapy is 14 days.
conclusions
- The rules for feeding a patient with dysphagia were violated;
- Adequate initial empirical antibacterial therapy was prescribed;
- The duration of antibacterial therapy is 14 days;
- No infectious complications;
- It is necessary to inform and discuss with the patient and his relatives the possibility of developing dysphagia and its symptoms against the background of the underlying disease;
- It is necessary to teach relatives the rules of feeding for dysphagia;
- It is important to promptly decide on the need for elective gastrostomy.