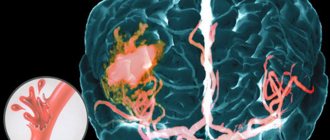
Ischemic stroke is a pathological condition that is not a separate or independent disease, but an episode that develops as part of a progressive general or local vascular lesion in various diseases of the cardiovascular system. Often, ischemic stroke is accompanied by the following diseases: arterial hypertension, atherosclerosis, rheumatic heart disease, coronary heart disease, diabetes mellitus and other forms of pathology with vascular damage. The clinical picture of ischemic stroke consists of general cerebral and focal symptoms, depending on the location of vascular disorders. The most important method for instrumental diagnosis of ischemic stroke, as well as its differentiation from hemorrhagic stroke, is CT and MRI of the brain.
ICD-10
I63 Cerebral infarction
- Causes
- Pathogenesis
- Classification
- Symptoms of ischemic stroke Brain infarction in the MCA basin
- Cerebral infarction in the ACA basin
- Cerebral infarction in the PCA basin
- Cerebral infarction in the vertebrobasilar region
- Differential diagnosis
- Therapy in the acute period
Causes
Since ischemic stroke is not considered as a separate disease, it is impossible to determine a single etiological factor for it. However, there are risk factors associated with an increased incidence of ischemic stroke, which can be divided into two groups:
1. Modifiable.
- myocardial infarction
- arterial hypertension
- atrial fibrillation
- diabetes
- dyslipoproteinemia
- asymptomatic lesions of the carotid arteries.
2. Unmodifiable.
- hereditary predisposition
- age
In addition, there are risk factors associated with lifestyle: low level of physical activity, acute stress or prolonged psycho-emotional stress, excess body weight, smoking.
General information
Brainstem stroke is a common neurological disease, accounting for 18–20% of all acute cerebrovascular accidents. In this case, the ratio of ischemic and hemorrhagic types is 3:1. The likelihood of developing pathology increases with age - people over 50–55 years of age suffer 1.8–2 times more often with each subsequent decade, but there is a steady trend towards younger age of the disease. The gender structure of vertebrobasilar strokes is usually dominated by men, although some forms are more common in women. Representatives of the Negroid race get sick more often than Europeans; the lowest risk was recorded in Asians.
Brainstem stroke
Pathogenesis
A certain sequence of molecular biochemical changes in the brain substance, caused by acute focal cerebral ischemia, can lead to tissue damage, resulting in cell death (cerebral infarction). The nature of the changes depends on the level of decrease in cerebral blood flow, the duration of this decrease and the sensitivity of the brain substance to ischemia. The degree of reversibility of tissue changes at each stage of the pathological process is determined by the level of decrease in cerebral blood flow and its duration in combination with factors that determine the sensitivity of the brain to hypoxic damage.
The term “infarction core” refers to a zone of irreversible damage, and the term “ischemic penumbra” (penumbra) refers to a zone of reversible ischemic damage. The duration of the penumbra's existence is the most important point, since over time, reversible changes become irreversible. The oligemic zone is a zone in which a balance is maintained between tissue needs and the processes that provide these needs, despite the decrease in cerebral blood flow. It is capable of existing for an indefinitely long time without passing into the core of the infarction, therefore it is not classified as a penumbra.
Classification
Ischemic stroke can be a consequence of one or another disease of the cardiovascular system. There are several pathogenetic variants of ischemic stroke. The TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification, which is most widely used, distinguishes the following types of ischemic stroke:
- cardioembolic - ischemic stroke caused by arrhythmia, valvular heart disease, myocardial infarction;
- atherothrombotic - ischemic stroke that occurred due to atherosclerosis of the large arteries, which resulted in arterio-arterial embolism;
- lacunar - ischemic stroke caused by occlusion of small arteries;
- ischemic stroke associated with other, more rare causes: blood hypercoagulation, arterial wall dissection, non-atherosclerotic vasculopathies;
- ischemic stroke of unknown origin - a stroke with an unknown cause or with the presence of two or more possible causes, when it is not possible to establish an accurate diagnosis.
In addition, a minor stroke is distinguished when the existing symptoms regress during the first three weeks of the disease.
There are also several periods of ischemic stroke:
- The most acute period is the first 3 days. Of these, the first three hours were defined as a “therapeutic window”, when it is possible to use thrombolytic drugs for systemic administration. In case of regression of symptoms during the first day, a transient ischemic attack is diagnosed;
- acute period - up to 4 weeks;
- early recovery period - up to six months;
- late recovery period - up to 2 years;
- period of residual effects - after 2 years.
Kinds
The disease is divided into several types:
- Depending on the location of the outbreak:
- right-sided;
- left-handed.
- In relation to the brain substance itself and the membranes, hemorrhage is divided into:
- parenchymal;
- subarachnoid.
- Parenchymal hemorrhage can be located in various parts of the brain:
- hemispheric;
- subcortical;
- cerebellar;
- stem;
- pavement.
- Subarachnoid hemorrhage, in turn, is divided into:
- basal;
- convexital;
- ventricular;
- mixed, combining the characteristics of several species.
There are several stages during a hemorrhagic stroke:
- Acute, characterizing the period of the disease from the moment of rupture of the vessel to the beginning of the formation of a hemorrhage focus.
- Acute, characterized by the continued release of blood from the damaged vessel with an increase in the volume of the hemorrhage.
- Subacute, in which the increase in the volume of hemorrhage stops.
- Chronic, caused by changes in the structure of the shed blood and the volume of hemorrhage.
Symptoms of ischemic stroke
The clinical symptom complex of ischemic stroke is varied and depends on the location and volume of the brain lesion. The most common localization of the lesion is in the carotid region (up to 85%), less often in the vertebral-basilar region.
Cerebral infarction in the MCA basin
A feature of a heart attack in the blood supply of the middle cerebral artery is the presence of a pronounced collateral blood supply system. Occlusion of the proximal middle cerebral artery can cause a subcortical infarction, while the cortical area of the blood supply remains unaffected. In the absence of these collaterals, an extensive infarction may develop in the area of the blood supply to the middle cerebral artery.
For a heart attack in the area of blood supply to the superficial branches of the middle cerebral artery, deviation of the eyeballs and head towards the affected hemisphere is typical. In this case, in case of damage to the dominant hemisphere, ipsilateral ideomotor apraxia and total aphasia develop, and in case of damage to the subdominant hemisphere, anosognosia, dysarthria, aprosody and contralateral neglect of space develop.
The main clinical manifestation of cerebral infarction in the region of the branches of the middle cerebral artery is contralateral hemiparesis and contralateral hemianesthesia. In the case of extensive lesions, concomitant abduction of the eyeballs and gaze fixation towards the affected hemisphere may occur. With infarctions of the subdominant hemisphere, emotional disturbances and spatial neglect develop.
The spread of paresis during a heart attack in the blood supply of the striatocapsular arteries depends on the location and size of the lesion (upper limb, face or the entire contralateral part of the body). In the case of extensive striatocapsular infarction, typical manifestations of middle cerebral artery occlusion (aphasia, homonymous lateral hemianopia) usually develop. Lacunar infarction is clinically manifested by the development of lacunar syndromes (isolated hemiparesis and hemihypesthesia or their combination).
Cerebral infarction in the ACA basin
The most common clinical manifestation of a heart attack in the blood supply of the anterior cerebral artery is motor disturbances. In most cases of occlusion of the cortical branches, motor deficits develop in the foot and entire lower limb, as well as mild paresis of the upper limb with extensive damage to the tongue and face.
Cerebral infarction in the PCA basin
As a result of occlusion of the posterior cerebral artery, infarctions of the occipital temporal lobe, as well as the mediobasal parts of the temporal lobe, develop. In such cases, clinical manifestations are visual field defects (contralateral homonymous hemianopsia). It is also possible that they may be combined with visual hallucinations and photopsia.
Cerebral infarction in the vertebrobasilar region
Stroke in the vertebrobasilar blood supply occurs as a result of occlusion of the only perforating branch of the basilar artery and is usually accompanied by symptoms of damage to the cranial nerves on the ipsilateral side. Occlusion of the vertebral artery or its main penetrating branches arising from the distal parts leads to the development of Wallenberg syndrome (lateral medullary syndrome).
Diagnostics
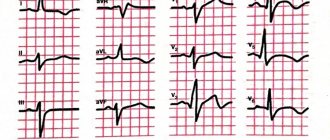
When collecting anamnesis, it is necessary to determine the onset of cerebrovascular accidents, establish the sequence and rate of progression of certain symptoms. Ischemic stroke is characterized by the sudden onset of neurological symptoms. In addition, attention should be paid to possible risk factors for ischemic stroke (diabetes mellitus, arterial hypertension, atrial fibrillation, atherosclerosis, hypercholesterolemia, etc.).
A physical examination of a patient with a possible diagnosis of ischemic stroke is carried out according to generally accepted rules for organ systems. When assessing the neurological status, pay attention to the presence and severity of cerebral symptoms (headache, impaired level of consciousness, generalized convulsions, etc.), focal neurological symptoms and meningeal symptoms. Laboratory tests should include general and biochemical blood tests, coagulogram, and urinalysis.
Instrumental diagnosis of ischemic stroke:
- MRI of the brain. The effectiveness of a new MRI mode, which produces diffusion-weighted images, has been proven. As a result of cytotoxic edema during ischemic stroke, water molecules move from the extracellular space to the intracellular space, which leads to a decrease in the rate of their diffusion. These changes appear on diffusion-weighted MRI images as an increase in signal, which indicates the development of irreversible structural damage to the brain substance.
MRI of the brain. Area of diffusion restriction in the cerebellum and brainstem on the left (acute ischemic stroke)
- CT scan of the brain. One of the early CT signs of ischemic damage in the MCA system is the lack of visualization of the lenticular nucleus or insular cortex (due to cytotoxic edema developing in the affected area). In some cases, with ischemic stroke, hyperdensity of sections of the middle and, much less frequently, posterior cerebral artery on the affected side is determined as early changes (a sign of thrombosis or embolism of these vessels). Already at the end of the first week, in the zone of ischemic damage in the gray matter, an increase in density to an isodense and even slightly hyperdense state is observed, which indicates the development of neovasogenesis and restoration of blood flow. This phenomenon has a “fogging effect”, because Difficulties arise in identifying the boundaries of the ischemic lesion zone in the subacute period of cerebral infarction.
CT scan of the brain. Extensive ischemic stroke in the temporal and parietal lobes on the right
Differential diagnosis
MRI and CT of the brain are also used to differentiate ischemic stroke from other forms of intracranial pathology and dynamic monitoring of tissue changes during the treatment of ischemic stroke. First of all, ischemic stroke must be differentiated from hemorrhagic stroke. Neuroimaging research methods will play a decisive role in this issue. In addition, in some cases there is a need to differentiate ischemic stroke from acute hypertensive encephalopathy, metabolic or toxic encephalopathy, brain tumor, as well as infectious brain lesions (abscess, encephalitis).
Bibliography
- Arkhipov S.L. Neuroimaging diagnostics and modern features of the treatment of hemorrhagic stroke. Diss. doc. honey. Sciences, Moscow, 1999, 248 p.
- Gabashvili V.M., Shakarishvili P.P., Dzhanelidze M.T., Dzhandzhagva T.V. Maruashvili M.G. Pathogenetic therapy of hemorrhagic strokes. Journal of Neurology and Psychiatry named after S.S. Korsakov. 1990; 5: 19-21.
- Shmyrev V.I., Arkhipov S.L., Kuznetsova S.E., Ternovoy S.K. Neuroimaging diagnostics and features of treatment of hemorrhagic stroke. Journal of Neurology and Psychiatry. S.S. Korsakov. 2001; 1:27-31
- Barnes JP, Karin M. Nuclear factor-kappa B: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1996;336:1066-1071
- Popova L.M. Respiratory support for hemorrhagic stroke. Journal of Neurology and Psychiatry named after S.S. Korsakov. 1977; 6: 842-50.
Treatment of ischemic stroke
If an ischemic stroke is suspected, the patient should be hospitalized in specialized departments. If the illness is less than 6 hours old, go to the intensive care unit of the same departments. Transportation should only be carried out with the patient's head elevated to 30 degrees. Relative restrictions to hospitalization are considered to be terminal coma, terminal stage of cancer, as well as a history of dementia with severe disability.
Non-drug treatment of ischemic stroke should include measures to care for the patient, correction of swallowing function, prevention and treatment of infectious complications (pneumonia, urinary tract infections, etc.). A coordinated multidisciplinary approach to it should be applied in a specialized vascular department with an intensive care unit (ward) with the ability to perform ECG, CT, clinical and biochemical blood tests, and ultrasound examinations around the clock.
Therapy in the acute period
Drug treatment of ischemic stroke is most effective at the very beginning of the disease (3-6 hours after the first signs of the disease appear). For thrombotic etiology of stroke, selective or systemic thrombolysis is performed; for cardioembolic origin, anticoagulant therapy is performed.
In the first 48 hours of the disease, it is necessary to periodically determine the oxygen saturation of hemoglobin in arterial blood. If this figure reaches 92%, oxygen therapy should be carried out, starting from 2-4 liters per minute. A decrease in the patient’s level of consciousness to 8 points or less (Glasgow Coma Scale) is an absolute indicator of tracheal incubation. The decision on the issue in favor of mechanical ventilation or against it is made based on the basic general resuscitation principles.
If there is a reduced level of wakefulness, if there are clinical or neuroimaging signs of cerebral edema or increased intracranial pressure, it is necessary to maintain the patient's head in an elevated state of 30 degrees (without flexing the neck!). It is necessary to minimize (and if possible eliminate) cough, epileptic seizures and motor agitation. Infusions of hypoosmolal solutions are contraindicated.
Planned therapy
An important component of the treatment of ischemic stroke is the correction of vital functions and the maintenance of homeostasis. This requires constant monitoring of basic physiological indicators, correction and maintenance of hemodynamics, water-electrolyte balance, respiration, correction of increased intracranial pressure and cerebral edema, prevention and control of complications.
- Infusion therapy. Routine use of glucose-containing solutions is inappropriate due to the risk of developing hyperglycemia; therefore, the main infusion solution in the treatment of ischemic stroke is sodium chloride solution (0.9%). With concomitant diabetes mellitus, patients are transferred to subcutaneous injections of short-acting insulin, except in cases where adequate glycemic control is carried out, and the patient is in clear consciousness and without impaired swallowing function.
- Providing food. Regardless of the location of the patient (intensive care unit, intensive care unit or neurological department), the daily task of basic therapy for ischemic stroke is adequate nutrition of the patient, as well as control and replenishment of water and electrolyte losses. An indicator for enteral tube feeding is considered to be the progression of certain swallowing disorders. In this case, the calculation of nutrient doses should be carried out taking into account the metabolic needs and physiological losses of the body. When administering food orally or through a tube, the patient should be in a semi-sitting position for 30 minutes after feeding.
- Prevention of thrombosis. In order to prevent deep vein thrombosis in ischemic stroke, wearing compression stockings or appropriate bandaging is recommended. For these purposes, as well as to prevent pulmonary embolism, direct anticoagulants (low molecular weight heparins) are used.
- Neuroprotection. Its main direction is the use of drugs with neuromodulatory and neurotrophic effects. The currently best-known neurotrophic drug is a hydrolyzate from pig brain. The brain and spinal cord do not have storage properties, and cessation of blood flow for 5-8 minutes causes the death of neurons. Therefore, the introduction of neuroprotective drugs must be carried out already in the first minutes of an ischemic stroke.
Thus, early rehabilitation against the background of basic therapy, as well as a combination of reperfusion and neuroprotection, can achieve certain successes in the drug treatment of ischemic stroke.
Surgery
Surgical treatment of ischemic stroke involves surgical decompression - reducing intracranial pressure, increasing perfusion pressure, and maintaining cerebral blood flow. Statistics indicate a decrease in the mortality rate for ischemic stroke from 80 to 30%.
Rehabilitation
During the rehabilitation period after an ischemic stroke, all efforts of neurologists are aimed at restoring the patient’s lost motor and speech functions. Electromyostimulation and massage of paretic limbs, exercise therapy, and mechanotherapy are performed. To correct speech disorders (aphasia, dysarthria), as well as swallowing disorders, consultation with a speech therapist is necessary.
Prognosis and prevention
The prognosis for ischemic stroke depends, first of all, on the location and volume of brain damage, the age of the patient, and the severity of concomitant diseases. The most severe condition of the patient occurs in the first 3-5 days of the disease, when cerebral edema increases in the area of the lesion. Next comes a period of stabilization or improvement with the possible restoration of impaired functions. Currently, the percentage of deaths from ischemic stroke is 15-20%.
The basis for the prevention of ischemic stroke is the prevention of thrombosis of blood vessels, which occurs when “cholesterol plaques” form in the blood. This requires maintaining a healthy lifestyle, adequate body weight, and abstaining from smoking and other bad habits. Patients suffering from various diseases of the cardiovascular system, arterial hypertension, hypercholesterolemia and diabetes are also at risk.
Secondary prevention of ischemic stroke is a comprehensive program that includes four areas: antihypertensive therapy (angiotensin-converting enzyme inhibitors and diuretics); antithrombotic therapy (indirect anticoagulants and antiplatelet agents); lipid-lowering therapy (statins); surgical treatment of carotid arteries (carotid endatherectomy).
You can share your medical history of what helped you in the treatment of ischemic stroke.
Complications
The pathology poses a serious danger to the patient's life. Extensive hemorrhages in the medulla oblongata threaten to disrupt vital functions - respiratory arrest, cardiac activity. Frequent complications of brainstem stroke are swelling, occlusive hydrocephalus, and convulsions. After the formation of a hematoma, dislocation of cerebral structures with tentorial herniation may develop, sharply aggravating the patient’s condition and worsening the prognosis.
In conditions of damage to the stem centers, multiple organ failure quickly develops, which is manifested by respiratory distress syndrome, decreased myocardial contractility, deep vein thrombosis and pulmonary embolism. A quarter of stroke patients experience falls, and some result in serious injury, including a hip fracture. Long-term immobilization is accompanied by bedsores; delayed complications include depression and epilepsy.