Myocardial infarction: symptoms, signs of the need for first aid
Myocardial infarction in medicine is defined as the development of necrotic changes in the heart.
This is one of the most acute clinical forms of IHD (coronary heart disease). The disorder occurs due to acute insufficiency of blood flow due to a failure in the supply of oxygen to the heart muscle. A heart attack may be indicated by sudden sweating, nausea, pain in the sternum, forearm and other parts of the body. Heart attacks in men occur 5 times more often than in women, which is especially noticeable in young and middle-aged people. Heart attacks in women develop on average 10-12 years later than in men. Among the reasons is the later development of atherosclerotic changes, which is facilitated by less widespread bad habits and the protective effect of estrogens in women.
conclusions
More than 15% of cases of heart attack at a young age develop as a result of hormonal disorders, changes in blood clotting, congenital pathology of the heart and blood vessels. In addition to atherosclerosis, the risk of a heart attack increases the risk of an unhealthy lifestyle, alcohol and smoking abuse, and excess weight. Often, a heart attack at the age of 35–45 years occurs with atypical symptoms, which complicates diagnosis and can lead to death if it is delayed to see a doctor. When the first alarming symptoms appear, you should call an ambulance. If a heart attack is confirmed, delivery to the hospital within 2–6 hours will allow stenting, minimizing the risk of consequences and preventing a dangerous outcome.
Causes of myocardial infarction
Myocardial infarction develops for various reasons, some of which are contributed by the person himself, others by his environment. Let us highlight 3 main groups of provoking factors:
- Factors that directly depend on the person - eating large amounts of fatty foods, smoking, excessive alcohol consumption.
- Factors that indirectly depend on a person are obesity, menopause and postmenopause.
- Factors that do not depend on a person - old age, genetic predisposition.
Myocardial infarction develops with atherosclerosis and inflammation in the walls of the arteries resulting from trauma, radiation exposure, vascular embolism, congenital anomalies and disruptions of the hematopoietic apparatus.
Risk factors
Unchangeable factors include:
- age (risk increases with age);
- gender (in men the risk of heart attack is higher, in women it increases and approaches “male” indicators in the postmenopausal period);
- genetic predisposition (heart disease in close relatives);
- race (for example, African Americans have a higher risk).
Modifiable (changeable) risk factors, i.e. factors that a person can influence:
- smoking (if you smoke, it is important to quit this habit);
- limiting the consumption of alcoholic beverages;
- control cholesterol levels, high blood pressure, diabetes (through proper nutrition, exercise, medications);
- playing sports, any physical activity (walking, cycling, cardio exercises);
- maintaining normal weight;
- a healthy diet (fruits, vegetables, whole grains, lean meats and milk, reducing the amount of salt consumed, eliminating fried and processed foods, foods containing saturated and hydrogenated fats, moderate consumption of sweets and baked goods);
- avoiding stress.
Heart attack: symptoms and first signs
- Patients do not always associate symptoms of a heart attack with the manifestation of this pathology. The patient’s feelings depend on what period of its development the disease is at. Common signs of a heart attack:
- severe dizziness, feeling of lack of air, shortness of breath;
- feeling of chronic fatigue, cold sweat on the body;
- uneven heartbeat, severe arrhythmia;
- pain impulses in the arms, forearms, shoulders, side, sternum;
- nausea, unpleasant heaviness in the stomach, loss of consciousness.
The first signs of a heart attack are not always obvious, but they attract attention. There are several periods of development of pathology:
- Pre-infarction stage - the first signs here are increased fatigue, weakness, fatigue, a feeling of squeezing and rapid heartbeat. There is no significant pain yet. In a patient with myocardial infarction, the lips and nail plates turn blue, the pulse becomes erratic and uneven. At this time, the severity of the disease increases, the duration of the period ranges from a couple of hours to a month.
- The most acute stage of heart attacks is pain. The patient begins to feel as if his chest is being squeezed in a vice. Behind the sternum there is a burning sensation, fiery heat, pulsating pain. With the development of an extensive heart attack, the pain is severe and prolonged. Strong and abrupt impulses are observed in young patients. Muffled pain, indicating myocardial infarction, is more often observed in patients with diabetes mellitus. The duration of the period is from half an hour to 2-4 hours. Complications that pose a direct threat to life are possible.
- Acute stage of a heart attack - among the first symptoms, the final formation of a focus of dead tissue and the occurrence of life-threatening conditions are noted. The duration of the period is 2-14 days.
- Subacute period - dead areas are replaced by connective tissue. The duration of the stage is 6-8 weeks.
- The post-infarction period lasts from two months to six months. During this time, the body adapts to new conditions.
If there are signs of a heart attack, you should not self-medicate; you should urgently consult a doctor, undergo an examination and get specialist recommendations.
Case from practice
A 54-year-old woman came to the clinic with complaints of weakness and nausea.
The problem was associated with malnutrition. During the interview, it turned out that she had been experiencing angina pectoris for 10 years; attacks occurred several times a month and were relieved with Nitroglycerin. The ECG shows signs of acute ischemia along the lower wall of the left ventricle, without the formation of a Q wave. Diagnosis: Small focal infarction.
The woman completed a full course of treatment in hospital, her condition improved, and she was discharged under the supervision of a local cardiologist. Recommended: following a diet, taking Aspirin Cardio, Metoprolol, Atrovastatin.
Where is the pain hidden during myocardial infarction?
Pain during myocardial infarction is localized in the chest area, spreading mainly to the left side of the chest space or being fixed in the central zone. The patient’s appearance also attracts attention: the skin is pale, moist, blue discoloration is visible in the area of the nasolabial triangle.
Myocardial infarction is often characterized by pain spreading to the left or right arm. Patients often talk about unpleasant sensations in their wrists, so similar to being put on squeezing handcuffs. The pain can go to the left shoulder blade and spread around the neck. The abundance of such places often complicates diagnosis, especially since pain symptoms are cyclical, increase and disappear in waves, and then everything repeats again.
Sometimes symptoms are observed for several days, and people do not rush to see a doctor because they are not aware of the development of signs of a dangerous disease. Another interesting symptom of a heart attack is known, when a person experiences hallucinations against the background of acute intense pain.
Atypical forms of the disease attract attention when the symptoms and first signs of a heart attack are manifested not by pain, but by shortness of breath, a feeling of lack of air and an irregular heartbeat. Acute infarction develops when a focus of necrotic tissue is finally formed. At this time, the pain disappears, the pressure drops, and the pulse quickens. The pain may persist if the affected area during a heart attack expands.
Expert advice
If there is a risk of developing myocardial ischemia, I recommend:
- spend time outdoors, walk, move more;
- switch to a low-calorie diet rich in vitamins and minerals;
- regularly check your heart function using an ECG and donate blood for cholesterol levels;
- give up bad habits (especially smoking);
- after establishing a diagnosis of angina, take medications that prevent the development of necrosis;
- at the slightest symptoms that may be harbingers of an acute condition, do not waste time, but immediately call a doctor.
Scheme of development of myocardial infarction
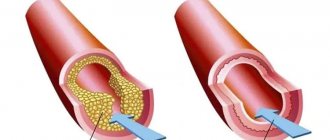
The atherosclerotic plaque loses its integrity and undergoes rupture. Its surface is corroded by erosion, which provokes inflammation. Plaque rupture is possible under the following circumstances: increased blood pressure, serious and exhausting physical activity, smoking, etc.
A blood clot forms that blocks the lumen of the coronary artery (thrombosis). The blockage occurs due to the clumping of platelets. A thrombus forms inside the plaque when its membrane ruptures, and only then comes out, closing the lumen of the coronary artery. If the blockage is sudden, a through myocardial infarction develops with necrotization of the entire thickness of the heart muscle. This is one of the most severe forms of the disease due to the high risk of death.
The coronary artery narrows sharply. With spontaneous or drug-induced dissolution of a blood clot and incomplete blockage of the artery, non-through infarctions are formed.
What it is
Signs of impending acute myocardial necrosis occur in 50–65% of cases. Scientists who have studied this phenomenon associate this condition with the gradual blocking of the lumen of the coronary vessel, while the heart attack itself represents a complete stop of blood circulation in a certain area. Wherein:
- The general excitability of the body changes, which ultimately leads to spasm of the coronary arteries.
- Atherosclerotic deposits cause contraction of smooth muscle fibers of blood vessels, increasing the likelihood of thrombosis and internal bleeding.
The narrowing of the coronary lumen against the background of spasm leads to necrosis. But it is preceded by an acute attack of angina, which can be seen on the ECG and is accompanied by vegetative manifestations.
Diagnosis and treatment for heart attack
An experienced doctor makes an accurate diagnosis at the first signs of illness. To help him - characteristic symptoms, a detailed clinical picture of a heart attack, electrocardiography indicators and identification of blood biomarkers indicating necrotic changes in the heart area. The first examinations upon treatment include a general blood test, biochemistry, echocardiography, and emergency selective coronary angiography.
Cardiologists deal with heart attacks; treatment depends on the severity of the pathology and how severe the symptoms are. The first signs of a heart attack in a woman or man indicate the need for urgent medical attention. The first and main tasks of doctors are to stop the development of necrosis of cardiac tissue, eliminate pain and associated complications.
In therapy, priority is given to the administration of painkillers, thrombolytic therapy, antiplatelet agents, and intravenous anticoagulants. In case of heart attacks, surgery of the heart muscle is possible - stenting and coronary artery bypass grafting.
Characteristics of the pathology
Fine-focal damage to myocardial cells followed by necrosis occurs as a result of:
- incomplete closure of the lumen of the vessel;
- the presence of collateral blood flow pathways;
- complete blockage of small arteries.
All these factors lead to subtle changes that rarely lead to complications. But with a repeated attack or disruption of the patency of several small-caliber vessels at once, the pathology can develop into a large-focal process with severe symptoms and serious consequences.
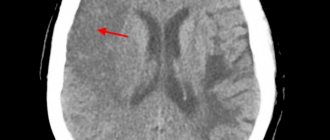
There are two types of microinfarction: intramural (located deep in the myocardium and does not affect the inner and outer layers) and subendocardial (on the inner lining of the heart). In the first case, a negative T wave is recorded on the ECG in the area of the disorder. In the second, the ST segment shifts below the isoline, as can be seen in the photo:
Prognosis after heart attacks
In case of heart attacks, you should be observed by a specialized specialist. After an illness, the situation may be complicated by cardiac arrhythmias, acute heart failure, cardiogenic shock, pericarditis, mental disorders and other pathologies. A professional doctor will help reduce the risks of exacerbations after myocardial infarction.
Our clinic provides services to patients with all types of cardiac pathologies, including those who have suffered a cerebral infarction (ischemic stroke). It is these complications of brain damage that are considered one of the main causes of increased mortality throughout the world. Despite this, our doctors do everything possible to maintain and improve the quality of life of their patients.
What diagnostic methods can be used to make a correct diagnosis?
The main method for diagnosing microinfarction is electrocardiography (ECG). Changes are characterized by the presence of:
- coronary negative T wave;
- downward shifted ST interval;
- absence of disturbances of the ventricular QRS complex.
It is possible to establish the localization of the focus of necrosis by the ratio of changes in standard and chest leads, the depth of the lesion (usually subendocardial location). Transmural necrosis is not possible for small lesions.
When scars are identified after a microinfarction, bundle branch blocks and signs of metabolic disorders are detected.
Laboratory indicators are less typical and therefore are not very informative in diagnosis:
- moderate leukocytosis is found in half of the patients;
- acceleration of ESR up to 15-40 mm/hour;
- a slight increase in fibrinogen concentration;
- enzymes indicating myocardial necrosis may be normal.