In TV shows and movies, a man who has a heart attack (heart attack) clutches his chest and falls to the ground. But most heart attacks are not that dramatic. It is necessary to distinguish between type 1 infarction and type 2 infarction. Let's look at their main features and main differences.
In TV shows and movies, a man who has a heart attack (heart attack) clutches his chest and falls to the ground. But most heart attacks are not that dramatic. It is necessary to distinguish between type 1 infarction and type 2 infarction. Let's look at their main features and main differences.
“No two heart attacks are the same,” says cardiologist Krishna Aragam at Massachusetts General Hospital. “Some heart attacks are less noticeable in presentation. But they can be just as serious and even fatal if left untreated.”
Causes
Myocardial infarction develops against the background of a sharp decrease or complete cessation of blood supply to myocardial tissue. Metabolic products accumulate in the cells, hypoxia develops and they die. Therefore, the bulk of the causes of the disease are directly related to the blood vessels supplying the heart.
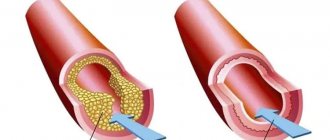
Atherosclerosis
It is atherosclerosis that leads to more than 90% of myocardial infarctions. Sclerotic plaques gradually narrow the lumen of the arteries, and if a blood clot breaks off, small vessels supplying the myocardium can be clogged. The result is impaired blood supply, hypoxia and cell death, and a high risk of mortality.
Hypertension
High pressure stretches the walls of blood vessels, making them fragile, which creates conditions for the formation of blood clots. Sharp fluctuations in blood pressure, and especially hypertensive crises, are often accompanied by insufficient blood supply to internal organs and excessive stress on the heart.
Spasms of heart vessels
Or the limited ability of the coronary arteries to transport the required volumes of blood to the myocardium. Functional problems may be associated with a low level of red blood cells in the blood, too low blood pressure, impaired oxygen saturation, and hypoxia.
Increased myocardial oxygen demand
A number of diseases increase the consumption of oxygen by the heart muscles, which is why the arteries cannot cope with delivering the required volume of blood. In this case, myocardial infarction develops against the background of:
- fever;
- increased heart rate and arrhythmia;
- hyperthyroidism;
- aortic stenosis;
- chronic heart failure;
- arteriovenous shunt;
- obstructive cardiomyopathies.
Cocaine, amphetamines and excessive cardio exercise can provoke an increase in myocardial oxygen demand.
Some inflammatory processes
There are a number of pathologies that cause the formation of arteritis - inflammatory foci on the walls of large vessels that reduce the capacity of the artery. A similar symptom is typical for:
- syphilis;
- systemic lupus erythematosus;
- Takayasu's disease;
- rheumatic diseases of various etiologies.
Mechanical damage
Trauma to the chest, sharp blows to the sternum and sudden compression of the body can lead to mechanical injuries to the myocardium. Within a few days of the episode, blood clots may form directly in the coronary vessels, blocking blood flow. The risk of a heart attack after severe bruises is low, but the patient needs to spend several days in the hospital to avoid a possible heart attack.
Postoperative period
Surgery differs from injury in the area of damage, but the risk of blood clots after surgery is quite serious. Coronography, coronary bypass surgery, and suturing of a cardiac aneurysm can lead to myocardial damage. The risks of myocardial infarction in such cases increase many times due to the presence of damage and the effects of anesthesia.
Risk factors
Myocardial infarction can develop rapidly without any external influences or be the result of a long illness. Some people are more likely to have a heart attack.
At risk:
- smokers;
- hypertensive patients;
- diabetics;
- overweight patients;
- people with lipid metabolism disorders;
- people with physical inactivity and leading a sedentary lifestyle;
- athletes during preparation for competitions;
- patients with depression or those in a state of chronic stress;
- patients with renal failure;
- those suffering from psoriasis and arthritis;
- people who have already had a heart attack before;
- the presence of mental disorders accompanied by mania, anxiety, hyperactivity;
- people over the age of 55 (men) and 65 (women) years.
The difference between age-related risks for men and women is explained by significant differences in lifestyle, physical activity and health habits. As a rule, men who undergo medical examination and lead a healthy lifestyle reduce their risk indicators to those of women.
Moreover, for men, the risk of an early heart attack is several times higher, and a woman is protected at the hormonal level before menopause - estrogens provide high elasticity of blood vessels and reduce the risk of fatal myocardial damage.
Why choose us
- high efficiency;
- full cycle of treatment;
- individual approach depending on the stage of development of the disease;
- the competencies of our specialists are recognized in the professional community;
- The center’s employees conduct educational conferences and master classes on diseases of the cardiovascular system. Our doctors regularly receive invitations from federal television channels with offers to participate in various health programs.
We treat not only the symptoms, but also the cause that led to the heart attack!
Mechanism of development of myocardial infarction
Poor circulation in the myocardium leads to cell hypoxia and subsequent death. Lack of oxygen leads to tissue necrosis within 10-15 minutes.
Any area of the heart can be affected: in the ventricles, interventricular septum, on the surface of the atria. The severity of a heart attack and its consequences depends directly on the location, area and depth of the lesion, as well as the size of the area of necrosis:
- Left ventricular myocardial infarction. The most common and at the same time the most dangerous. The most negative prognosis is for damage to the anterior wall of the left ventricle - the more extensive the damage, the higher the risks of complications and death.
- Transmural infarction, in which the entire thickness of the myocardium is subject to necrosis, can spread to neighboring parts of the heart. In the intramural form, necrosis affects only the inner surface of the myocardium.
- Small-focal infarction is characterized by the formation of several small zones of necrosis and blurred general symptoms. Usually. the lesion is shallow. One large lesion is formed in 30% of cases, and wave-like deterioration of the condition means the growth of the damage zone. As a rule, large-focal infarction is associated with damage to the coronary arteries.
- Subepicardial, or superficial, infarction affects the outer lining of the heart. often with rupture of blood vessels, hemorrhage and usually with death.
- Septal infarction affects the septum between the ventricles.
- Right ventricular myocardial infarction is rarely diagnosed, but gives the most favorable prognosis.
First aid
For the patient, the manifestation of these symptoms may seem like an extremely intolerable period; it is then that everything must be done to prevent the stress of a loved one.
You can give the patient a sedative tablet and urgently call an ambulance. Important! In the first half hour of noticeable symptoms, the future fate of the patient is decided, from which it follows that the provision of qualified medical care cannot be delayed even for a minute. After timely hospitalization, you should strictly adhere to the regimen prescribed by the doctor.
Symptoms and stages of development of myocardial infarction
The typical course of myocardial infarction begins long before the onset of acute symptoms and ends much later than the period of hospitalization. Precursors of a heart attack are united by the term pre-infarction state or prodromal period, which lasts up to 30 days and allows you to take measures to prevent myocardial necrosis.
Signs of the prodromal period:
- tachycardia and angina;
- recurring pain in the heart area;
- the number of endothelial cells in the blood increases approximately 4 times;
- homocysteine levels jump by 25-30% of the age norm;
- shortness of breath, dizziness and swelling of the limbs in the evenings.
Contact a cardiologist with any complaints of discomfort in the chest, shortness of breath, or dizziness. a sharp increase in heart rate and lightheadedness allows you to diagnose a pre-infarction condition and avoid a heart attack.
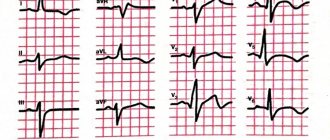
Anginal or acute stage
A patient who has not consulted a doctor with complaints at the pre-infarction stage almost always encounters this stage; 60% of patients have a chance to survive the most acute period of a heart attack. In fact, the beginning of myocardial infarction is called precisely this period, lasting from 15 minutes to 3-6 hours. Signs of the onset of a heart attack:
- intense pain lasting longer than 15 minutes, more severe than with angina pectoris and radiating to the left side - to the arm, chest, under the shoulder blade, to the teeth;
- increased heart rate, the appearance of extrasystoles - random, extraordinary contractions of the heart;
- lump in throat, panic, fear of death;
- pale skin, blue nasolabial triangle, sticky cold sweat;
- shortness of breath and dry cough, slight fever, chills;
- with a right ventricular infarction, the jugular veins swell;
- A sharp increase or decrease in blood pressure and fainting are possible.
Any attack of angina can develop into a myocardial infarction, so calling an ambulance at the first sign significantly increases the chances of recovery. The severity and duration of the symptoms indicate an increase in the affected area.
Atypical course of myocardial infarction
In addition to the typical signs of the anginal phase of a heart attack, characteristic of men, there are a number of atypical scenarios that are more often observed in women:
- Anginal form, in which the symptoms are very similar to an attack of angina, but are not associated with physical or nervous stress. The pain can last up to several hours; taking nitroglycerin does not alleviate the condition. The similarity with intercostal neuralgia is also quite pronounced, but there is no pain in the intercostal spaces.
- Gastralgic form. It is quite rare and is accompanied by localized pain in the upper abdomen, belching, and vomiting. Often the gastralgic variant of a heart attack is mistaken for an acute attack of pancreatitis, perforation of a stomach ulcer or peritonitis. A characteristic sign of a heart attack in this case is a soft abdomen without tension in the anterior abdominal wall.
- Asthmatic myocardial infarction quite reliably imitates an asthma attack: difficulty inhaling, severe shortness of breath, hoarse exhalation. Anti-asthma drugs are ineffective.
- Painless small-focal infarction - often occurs in diabetics, and is accompanied by weakness, shortness of breath and rapid heartbeat. Often the symptoms disappear after some time, but the patient requires hospitalization.
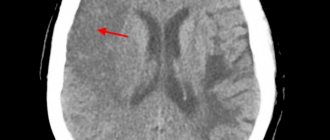
- The cerebral form occurs in the scenario of an ischemic stroke: the head hurts severely, speech becomes slurred. disorientation occurs and fainting is possible.
An urgent blood test helps determine myocardial infarction in atypical forms.
Acute period of heart attack
It comes after the most acute period: a focus of necrotic tissue damage is formed, and with it the resorption-necrotic syndrome begins. The general reaction of body tissues to the entry of dead myocardial cells into the bloodstream is accompanied by impaired cardiovascular activity. In general, if myocardial infarction proceeds without complications, this phase takes 7-10 days.
It is in the first ten days after the acute phase that a recurrent infarction with a high mortality rate is possible.
Subacute period
A scar gradually forms at the site of tissue necrosis. The timing of its formation depends, first of all, on the area of the lesion and the condition of the adjacent myocardial tissue. On average, the stage lasts up to one and a half months in the absence of complications and relapses.
Post-infarction period
The formed scar becomes denser, and the body begins to adapt to the new condition, launching compensatory mechanisms. Rehabilitation begins. which takes six months to a year.
What should a patient do during a heart attack?
Unfortunately, during an attack there are not always people nearby who could help. Therefore, it is important to know what to do if the disease strikes a person at a time when no one is nearby. The first rule is don't panic. Panic can make the situation worse. A person must understand that first aid for a heart attack can be provided to oneself. Naturally, first of all, you need to call a doctor, explain how to get into the house or apartment and leave the front door open just in case. Next, it is necessary to ensure the presence of fresh air in the room. To do this, you can open the windows or turn on the air conditioner. Nitroglycerin should be placed under the tongue, which, once it penetrates into the blood, will relieve painful sensations. Aspirin can also help in the first minutes of an attack. The drug helps thin the blood and alleviates the symptoms of the disease. For faster action of the drug, the tablet must be chewed.
A person should sit down or lie down so that the upper part of the body is slightly higher than the lower part. Legs should be bent at the knees. It is this position of the body that maximizes blood supply. Next, you need to wait for emergency medical attention.
Treatment
If you consult a doctor in the early stages of a heart attack, you can avoid surgical intervention: modern drugs restore blood circulation and myocardial function. limit the area of necrosis and reduce the risks of complications.
Surgery is indicated in acute conditions. Typically carried out:
- coronary artery bypass surgery, which creates a path for blood to bypass the blocked section of the artery;
- coronary artery angioplasty, in which the site of blockage or narrowing is expanded and additionally stented - a frame is placed inside the aorta to prevent re-blockage.
Consequences and complications
Compliance with all medical prescriptions during the rehabilitation period and after allows you to minimize complications that arise in the long term. In the first hours and days the patient is threatened with:
- sudden cardiac arrest;
- rupture of the interventricular wall;
- thromboembolism;
- psychosis, increased anxiety, increased psychomotor activity;
- arrhythmia;
- acute left ventricular failure;
- acute right ventricular failure;
- cardiogenic shock;
- early cardiac aneurysm.
The listed complications have a catastrophic mortality rate, therefore, within 10-15 days from the onset of the acute phase of a heart attack, the patient must be under the supervision of doctors in a hospital.
Late complications arise already during the rehabilitation period and can be corrected:
- chronic heart failure;
- late cardiac aneurysm in the scar area;
- post-infarction syndrome;
- parietal thromboendocarditis with the formation of blood clots in the heart chambers;
- cardiosclerosis with subsequent cardiac dysfunction.
Late consequences of a heart attack
At the end of the acute period of the disease, so-called late consequences may develop. These include complications that appear 10 days after the manifestation of MI and later:
- post-infarction Dressler syndrome occurs 2-6 weeks after the manifestation of myocardial infarction and is manifested by inflammation of the pericardium, pleura, alveoli, joints and other pathological changes;
- thromboendocarditis with thromboembolic syndrome (the appearance of a wall thrombus in the heart cavity, on the heart valves);
- late post-infarction angina, which is characterized by the occurrence or increase in frequency of angina attacks. Its frequency ranges from 20 to 60%.
Some patients who have suffered an acute myocardial infarction are at high risk for developing repeated complications of coronary heart disease and, above all, recurrent myocardial infarction and unstable angina. This is due to the fact that in patients with acute coronary syndrome, along with the presence of an atherosclerotic plaque, which was complicated by a rupture and blocked the lumen of the coronary artery, there are plaques in other arteries. They can be the cause of repeated episodes of cardiovascular events, the probability of which is very high.
Rehabilitation and prevention of recurrent heart attack
After stabilization of the condition and restoration of cardiac activity, a long and difficult period of rehabilitation begins. Over time, the patient will need to take a number of maintenance medications. Antiplatelet drugs, for example, Fazostabil, will need to be taken for life.
Motor activity must be restored to prevent a recurrent heart attack, but this must be done gradually. In the absence of negative symptoms, the ban on walking is lifted already on the 2-3rd day of hospital stay, but high intensity walking, running, dancing and any sports hobbies are prohibited for the patient, if not forever, then at least until complete rehabilitation.
The diet will have to be changed - after a myocardial infarction, all fast food, fatty meat, spicy seasonings, marinades, and sauces are prohibited. Excessively salty foods provoke swelling, fried foods and smoked foods accelerate the development of atherosclerosis. Lean meat and fish, almost all fruits and vegetables, most cereals, and dairy products remain permitted. The number of meals will have to be increased to at least 4-5 per day.
Social activity is not prohibited for the patient, but should have a positive connotation: a minimum of stressful situations, strong feelings, and worries. Communication with animals and friendly people will be beneficial.