Find out more about other pathologies starting with the letter “D”: Debility, Double-wave viral meningoencephalitis, Dementia with Lewy bodies, Depressive neurosis, Dermal sinus, Cerebral palsy, Jacksonian epilepsy, Diastematomyelia (diplomyelia), Discogenic myelopathy, Dystrophic myotonia Rossolimo-Steinert-Kurshman , Diabetic encephalopathy, Dyscirculatory encephalopathy, Diffuse axonal damage to the brain, Benign rolandic epilepsy.
Discirculatory encephalopathy: the danger of pathology and treatment methods
This pathology is a brain lesion that occurs due to constant progressive circulatory disorders of the central nervous system of various etiologies. It affects motor, emotional and cognitive function, and depending on the severity of the symptomatic picture is divided into three stages. To make and confirm the diagnosis, ultrasound, echo-EG, EEG, REG, duplex scanning of cerebral vessels, ophthalmoscopy, MRI are required. Therapy is selected individually and consists of neuroprotective, antiplatelet, antihypertensive, vascular and other drugs.
Causes
Damage to nerve cells can occur due to exposure to various pathological factors.
- previous trauma;
- acute or chronic intoxication with salts of heavy metals, narcotic substances, alcohol;
- blood supply disorders (atherosclerosis, arterial hypertension, amyloidosis, etc.);
- infectious diseases (diphtheria, botulism, tetanus and others);
- disorders of the liver or kidneys, accompanied by the accumulation of toxins in the blood;
- disorders of glucose metabolism;
- lack of vitamins (especially group B);
- water retention, lack of sodium in the blood and resulting swelling;
- immunodeficiency states;
- exposure to ionizing radiation;
- hypoxia: insufficient oxygen supply to brain cells.
Causes
The main reason for its appearance is chronic cerebral ischemia caused by various vascular disorders:
- About 60% of cases of DEP are caused by atherosclerotic changes in the walls of cerebral vessels;
- Arterial hypertension ranks second in the list of causes. It can be observed in a number of pathologies: chronic glomerulonephritis, hypertension, polycystic kidney disease, Itsenko-Cushing's disease, pheochromocytoma, etc.
- Hypertension provokes encephalopathy due to the occurrence of vasospasm of the central nervous system, leading to depletion of blood flow;
- Pathology of the vertebral arteries can also cause the disease, as it is responsible for 30% of cerebral circulation. If the primary disease is instability of the cervical spine of a dysplastic nature, osteochondrosis, Kimerli's anomaly, developmental defects or previous spinal trauma, a symptomatic picture of circulatory disorders in the vertebrobasilar region is observed;
- DEP often occurs as a concomitant disease with diabetic microangiopathy. If, with diabetes, the patient is unable to adjust the blood glucose level to the upper limits of normal.
Also, the causes of dyscirculatory encephalopathy can be:
- Chronic or persistent hypotension;
- Arrhythmia;
- Hereditary angiopathy;
- Traumatic brain injuries;
- Systemic vasculitis.
Examination and treatment
Discirculatory encephalopathy
is a neurological disease with slow progression. It is characterized by a lack of blood supply to the blood vessels of the brain. As a result, its functions are disrupted in the area of the affected lesions. The disease occurs in both elderly and young patients. The sooner treatment is started, the higher the chances of full recovery.
Get diagnosed with disculatory encephalopathy at Clinic No. 1:
- MRI
- Consultation with an ophthalmologist
- EEG, REG
- Ultrasound of vessels
- Duplex scanning
For one-time payment for services - 20% discount
Call
The mechanism of pathology development
The pathogenesis of dyscirculatory encephalopathy includes factors leading to deterioration of cerebral circulation, consequently to hypoxia and disruption of trophism of cells of the central nervous system. This leads to cell death and the appearance of areas of rarefaction of brain tissue, that is, leukoaraiosis or silent infarctions - multiple small lesions.
The subcortical structures and white matter of the deep parts of the brain are most susceptible to destruction during DEP. This is due to their location on the border of the carotid and vertebrobasilar basins. Chronic ischemia provokes the phenomenon of disconnection, that is, disruption of connections between the cerebral cortex and subcortical ganglia. Experts believe that this is the main pathogenetic mechanism. It causes a characteristic symptomatic picture:
- Violation of the emotional sphere;
- Cognitive disorders;
- Pathologies of motor functions.
A distinctive feature of DEP is the reversibility of functional disorders at the first stage of the disease with appropriate treatment and the persistent nature of neurological defects leading to disability at later stages.
General information
Encephalopathy occurs due to metabolic disorders in brain cells. Regardless of the cause, the pathology follows a single scenario. First, there is a decrease in the activity of neurons, then their gradual death. Foci of dystrophy are located throughout the brain, which causes a variety of symptoms.
The damage is irreversible, but with timely consultation with a specialist and quality treatment, the patient’s condition can improve. The remaining intact neurons partially take over the function of the dead cells, and brain function is significantly improved. If the disease was caught at an early stage, the patient retains complete clarity of mind.
Make an appointment
Classification of dyscirculatory encephalopathy
DEP is distinguished by etiology:
- Atherosclerotic;
- Hypertensive;
- Venous;
- Mixed.
According to the speed of development, it can be rapidly progressing or galloping and slowly developing, that is, the classic form.
The severity classification is as follows:
- The first stage is accompanied by subjective feelings of ill-being, mild cognitive impairment, and preservation of the neurological status;
- The second stage is characterized by obvious motor and cognitive disorders and increased emotional distress.
- The third stage is considered the most severe, at which mental disorders begin. It represents vascular dementia of varying severity.
Classification
Taking into account the cause of development, the disease can be atherosclerotic, venous, hypertensive and mixed. Depending on the characteristics of the course, classic, galloping (rapidly progressing) and remitting varieties of the disease are distinguished. To clarify the severity of the process, a general three-stage classification is used, where:
- Stage 1 (initial). There are minor disorders of the emotional sphere and cognitive activity, there is no neurological deficit.
- Stage 2 (moderate). Cognitive-emotional dysfunction worsens and is accompanied by motor symptoms.
- Stage 3 (decompensation). The ability to work and the ability to self-care are lost, and dementia develops.
Early symptoms
DEP begins unnoticeably and develops quite slowly. First of all, problems in the emotional sphere are noted. About 65% of patients suffer from depression, which, unlike depressive neurosis, occurs against the background of minor traumatic situations, while patients are not inclined to note depression and low mood. They are fixed on various somatic disorders, like patients with hypochondriacal neurosis. Complaints may include:
- Arthralgia;
- Back pain;
- Neuralgia;
- Noise in the head;
- Tinnitus;
- Pain of various localizations.
Their distinctive feature is that they do not fit into the clinical picture of supposed somatic pathologies. Depression in DEP is difficult to respond to psychocorrection and treatment with antidepressants.
The initial stage of DEP often manifests itself in increased emotional lability, which includes:
- Sudden mood swings;
- Cases of uncontrollable crying for minor reasons;
- Irritability;
- Attacks of aggressive behavior towards others.
In addition, sleep disturbances, fatigue, headaches, and absent-mindedness are noted. The symptomatic picture is similar to neurasthenia, but with dyscirculatory encephalopathy the symptoms are combined with cognitive impairment.
Moreover, in 90% of patients, cognitive impairment occurs at the initial stage of the disease. These include:
- Decreased concentration;
- Memory impairment;
- Reduced speed of thinking;
- Difficulties in planning activities;
- Fatigue with mental effort;
- Problems with speech reproduction of information while maintaining memory.
Movement disturbances, such as dizziness and unsteadiness when walking, may also occur. DEP must be differentiated from vestibular ataxia, since nausea and vomiting may be present, but only during walking.
Symptoms
Stage 1
Characterized by a gradual onset and chronic course. Emotional disturbances are often the most noticeable in the beginning. In 65% of cases, depressive symptoms reminiscent of hypochondriacal neurosis are detected. Complaints of depression and decreased mood are usually absent; unpleasant somatic sensations come to the fore: headache, noise and ringing in the head, pain in the back and joints.
Differences from neurotic depression are the absence of a provoking traumatic situation, the low effectiveness of psychotherapy and antidepressants. In adults, the symptom that determines the picture of the disease is sometimes emotional lability: attacks of aggression or causeless crying, sudden changes in mood, increased irritability. The clinic is complemented by absent-mindedness, deterioration of sleep and fatigue.
In 90% of patients, cognitive impairment occurs at the initial stage. The ability to concentrate and plan actions decreases. Memory deteriorates, thinking slows down. In the motor sphere, dizziness and slight instability when walking are sometimes detected, which are the first signs of vestibulopathy.
Stages 2 and 3
When moving from grade 1 to grade 2, motor and cognitive dysfunction worsens. Due to amnesia, decreased attention and intelligence, usual mental work becomes unbearable. A decrease in criticism and the ability to navigate in place and time arise and gradually worsen. At stage 3, behavior and personality suffer. Due to dementia, patients lose their ability to work, and in severe cases, their ability to self-care.
Apathy prevails. People are not interested in anything, do nothing or do something unproductive, and show indifference to the world around them. Movement disorders become more pronounced and noticeable from the outside. A shuffling gait is formed in small steps without lifting the foot off the floor. Patients with vestibulo-atactic syndrome have progressive balance disorders.
Signs of transition to stage 3 are severe speech problems, paresis, trembling of the limbs, urinary incontinence and pseudobulbar syndrome. Some patients develop symptomatic epilepsy. Due to unsteady gait, people fall, resulting in fractures. Women especially often suffer from injuries, which is due to the prevalence of osteoporosis during menopause.
Clinical picture at stage II-III
In subsequent stages, the clinical picture grows and intensifies: memory deteriorates significantly, attentiveness and intelligence decrease, and difficulties are noted when performing habitual mental work. Patients are unable to adequately assess their own condition and tend to overestimate their performance and intelligence. Over time, the ability to develop a program of action, generalization, and orientation in time and space is lost. At the third stage, disturbances in praxis and thinking are noticeable. Personality and behavior disorder occurs. Dementia is noted, in which patients lose the ability to work, and in more severe cases, self-care skills.
The emotional stage is dominated by apathy, loss of interest in previous hobbies, and lack of motivation. At the third stage, patients do nothing or are engaged in unproductive activities. They are indifferent to themselves and their surroundings.
If at the first stage motor disorders are weakly expressed, then at later stages these disorders are visible to others. Typical manifestations are:
- Slow gait in small steps;
- Shuffling;
- Falls when walking or turning, which are often accompanied by fractures, especially if the patient suffers from osteoporosis;
- Difficulty starting or stopping in time.
Clinical manifestations, especially the characteristic “skier’s gait,” are similar to the symptoms of Parkinson’s disease, but are not accompanied by abnormalities in the arms, so experts call such signs of DEP “vascular parkinsonism” or “lower body parkinsonism.” Also, the last stage is accompanied by:
- Urinary incontinence;
- Pseudobulbar syndrome;
- Paresis;
- Tremor;
- Severe aphasia;
- Symptoms of oral automatism.
Epileptic seizures may occur.
What is encephalopathy and why is it dangerous?
Every person experiences headaches from time to time. Many people do not take into account the reasons for feeling unwell and prefer to take painkillers. However, recurrent headaches can be caused not only by fatigue or changes in blood pressure. Is this often how encephalopathy manifests itself? a common brain disease caused by oxygen starvation and lack of nutrients. We will talk further about whether this pathology can be cured and prevented.
What is encephalopathy?
This is a non-inflammatory disease in which the brain tissue receives insufficient blood and, therefore, oxygen. As a result, nerve cells die, stagnant processes appear, and swelling of the meninges forms in local areas.
Encephalopathy? this is a general concept that unites degenerative processes in the brain. Very often, pathology is not defined as an independent disease, but is detected against the background of other diseases. There are no age restrictions for encephalopathy.
| ! | The optimal rate of blood supply to the brain is 45-50 ml of blood every minute per 100 g of brain matter. Reducing this figure to 18 ml per minute is considered critical. |
Causes of the disease
Encephalopathy can be congenital or acquired. In each case, the causes of the disease are different factors, but they are united by a persistent violation of cerebral circulation.
| Congenital | Acquired |
|
|
In the case of newborn children, the presence of the disease is not always obvious. As a rule, the diagnosis is made closer to a year in the presence of specific symptoms. In adults, pathologies caused by vascular disorders are widespread. For example, with atherosclerosis, the lumen of blood vessels decreases as a result of the deposition of lipids on their walls. Blood flow to the brain decreases, ischemia develops. In difficult cases, the lumen of the vessel is blocked by a blood clot or cholesterol plaque, a stroke occurs, as a result of which brain cells die.
Types of encephalopathy
Two main forms of the disease? perinatal (congenital) and acquired. The first includes a decrease in blood supply to the brain that occurred between 28 weeks of intrauterine development of the fetus and the 7th day of the child’s life. All other types of encephalopathy? acquired.
Each type of disease has its own specific symptoms and treatment methods. For this reason, it is important to see a doctor in time to undergo diagnosis and treatment. The manifestations of the disorders depend on which area of the brain is affected.
- Vascular encephalopathy.
It occurs as a result of impaired blood supply to the brain and oxygen starvation of cells. The pathology may be atherosclerotic or hypertensive in nature. In the first case, atherosclerotic plaques are present in the blood vessels, and in the second, high blood pressure is observed with a complication in the form of cerebral edema.
- Traumatic.
In this case, encephalopathy develops as a result of a traumatic brain injury. The disease may cause degenerative, dystrophic, and scarring changes in brain tissue. Most often, the pathology is observed in athletes, drivers and passengers of vehicles, as well as newborn children.
- Radial.
The disease can result from exposure of the brain to ionizing radiation. This type of encephalopathy can be observed among specialists involved in eliminating the consequences of radiation accidents, as well as among those who work with related equipment.
- Metabolic (toxic).
Brain damage can be caused by intoxication of the body due to liver failure, diabetes, carbon monoxide poisoning, heavy metal salts, etc. Toxic poisoning also leads to severe neurological disorders.
- Alcoholic.
The breakdown products of ethyl alcohol, entering the brain through the bloodstream, cause irreversible metabolic disorders. Does Wernicke's encephalopathy also belong to this group? damage to the midbrain and hypothalamus due to alcohol abuse, as well as vitamin deficiency and other reasons.
- Inflammatory.
Most often we are talking about inflammatory processes in the walls of blood vessels. The severity and specificity of manifestations depend on the affected area.
- Vaccine.
This is a rare type of neurological disorder that occurs in response to the vaccine. The most common reaction is to whooping cough medications.
- Discirculatory.
Brain dysfunction occurs due to gradually increasing insufficiency of blood supply. Dyscirculatory encephalopathy directly affects cognitive abilities and neurological disorders.
- Residual encephalopathy (residual).
Structural changes in tissue occur in the brain due to previous injuries, ischemic disease, and infections.
- Spongy.
This type of encephalopathy combines severe diseases in which the brain turns into a spongy body. Among them are Getsmann-Straussler-Scheinker syndrome, Creutzfeldt-Jakob disease, etc.
Symptoms of encephalopathy
The disease is characterized by a variety of clinical manifestations, which depend on the causes of brain dysfunction. Encephalopathy can have an acute and chronic course.
In the first case, symptoms appear suddenly and very quickly lead to a deterioration in the patient’s condition. The main cause of acute encephalopathy is toxic damage to the body.
In the second case, signs of brain dysfunction appear gradually in the form of headaches, forgetfulness, and emotional instability.
The disease goes through several stages in its development, which are characterized by the following manifestations:
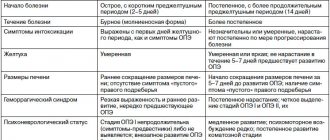
| Stage 1 | Stage 2 | Stage 3 |
|
|
|
| ! | The main manifestations of encephalopathy at the initial stage? headaches, dizziness, tinnitus. Symptoms may occur when the weather changes, physical fatigue, or stress. When they appear, it is necessary to undergo examination. |
Diagnosis of the disease
Modern examination methods make it possible to establish the localization, nature of the pathology, and the mechanism of its occurrence. Diagnostics may include:
Blood tests to determine the levels of hormones, lipids, cholesterol, sugar and other elements that may indicate the development of dyscirculatory encephalopathy.
Rheoencephalography (REG) to measure blood flow in the brain, determine the elasticity and tension of the walls of blood vessels.
Magnetic resonance imaging
to analyze morphological changes in brain tissue. MRI allows you to differentiate encephalography from other diseases of the nervous system: Alzheimer's disease, stroke, tumors, etc.
Doppler ultrasound
to determine the speed of blood flow in an individual blood vessel and clarify the location of the atherosclerotic plaque. Provides information about the state of cerebral circulation.
Ultrasound scanning
to clarify the cause of vessel obstruction? the presence of a spasm, plaque, blood clot, etc. The method has no contraindications and allows you to quickly obtain a reliable result.
Ultrasound monitoring
to determine the cause of blood clot formation? thrombi and emboli. The method also allows you to assess the risk of stroke.
Can encephalopathy be cured?
The disease requires long-term course therapy and observation by a neurologist. For successful treatment and elimination of the symptoms of the disease, diagnosing the causes of its occurrence is of paramount importance.
Acute encephalopathy is an indication for urgent hospitalization and detoxification therapy in a hospital setting. The chronic form of the pathology requires following a certain diet and taking medications as prescribed by a doctor 2–3 times a year.
For hypertension (high blood pressure), the doctor may prescribe Enalapril, Captopril, Lisinopril, Fosinopril and other drugs.
Medicines for hypertension require strict adherence to the dosage schedule, usually 2–3 times a day. Many patients require lifelong use of medications to normalize blood pressure. The dosage and type of medication should be prescribed by the attending physician, since each of them acts with different intensity and is excreted from the body differently.
Modern antihypertensive drugs are divided into the following groups:
- ACE inhibitors (angiotensin-converting enzyme);
- diuretics;
- beta blockers;
- calcium antagonists;
- direct renin inhibitors;
- combination and other drugs.
To improve brain metabolism, Cavinton, Vasobral, Corinfar, Tseliprol, Nikoshpan, Picamilon and other drugs of various groups are prescribed.
Medicines help restore cerebral circulation and thereby eliminate symptoms such as:
- headache and dizziness;
- increased fatigue;
- impaired coordination of movements;
- memory problems;
- insomnia;
- mood swings, etc.
The main groups of drugs to improve cerebral circulation:
- vasodilators;
- blood thinners;
- nootropic;
- vascular strengthening;
- blood microcirculation correctors, etc.
Do free radicals accumulate in the human body during life? reactive oxygen species that destroy cells and lead to diseases of the nervous and cardiovascular systems. To protect tissues from their effects, are antioxidants prescribed? “Actovegin”, “Tiogamma”, “Emoxipin”, “Quertin”, “Riboxin”, “Mexidol”, “Cerakson”, etc. The drugs improve capillary blood flow, strengthen the walls of blood vessels, prevent or slow down atherosclerotic changes, reduce the risk of stroke and heart attack.
| For encephalopathy, the treatment regimen is developed individually for each patient, taking into account data from laboratory and instrumental studies. Almost all drugs for the treatment of chronic forms of the disease are available in pharmacies with a doctor’s prescription. In addition to the listed groups of drugs, the patient may be prescribed anticonvulsants, antidepressants, antiplatelet agents and other drugs. |
Consequences and complications of encephalopathy
Delaying treatment for a long time leads to extensive brain damage. As the disease worsens, the patient may experience:
- constant headaches;
- disorder of consciousness;
- deterioration of vision and hearing;
- facial expression disorders;
- movement coordination disorders;
- tremor of limbs, tic, convulsions;
- sexual function disorder;
- vegetative-vascular dystonia and much more, depending on the area of brain damage.
Prevention of encephalopathy
For successful treatment, elimination of symptoms of the disease and prevention of degenerative processes in the brain, the patient is recommended:
- adjust your diet? give up foods high in cholesterol and fast carbohydrates in favor of vegetables, fruits, and herbs;
- to refuse from bad habits ? smoking and drinking alcohol;
- Exercise regularly to keep your body in good shape.
If you consult a doctor in a timely manner and detect encephalopathy in the early stages, the prognosis is positive. The effectiveness of treatment will largely depend on the causes of the pathology. Severe cardiovascular (ischemia, stroke, heart attack) and neurological (osteochondrosis, traumatic brain injury) diseases may require lifelong course therapy. In each case, the treatment and prevention program should be drawn up by the attending physician.
Methods for diagnosing DEP
It is very important to make a diagnosis as early as possible in order to promptly begin vascular therapy to compensate for neurological disorders. Therefore, all patients at risk for discirculatory encephalopathy must be regularly examined by a neurologist. The risk group includes:
- People suffering from atherosclerosis;
- Diabetics;
- Hypertensive patients;
- Aged people.
To identify cognitive impairment, special tests are required. Tasks may include the need to remember and repeat a list of words named by the doctor, draw a dial with a given time, or repeat certain words.
In addition, consultation with an ophthalmologist and ophthalmoscopy, determination of visual fields, will be required. The following hardware diagnostic methods are shown:
- Echo-EG;
- EEG;
- REG;
- ECG and daily ECG monitoring;
- Doppler ultrasound of head and neck vessels;
- MRA of cerebral vessels;
- Duplex scanning;
- MRI of the brain.
MRI of the brain will help distinguish DEP from other pathologies: Alzheimer's disease, Creutzfeldt-Jakob disease, disseminated encephalomyelitis. Magnetic resonance imaging makes it possible to visualize foci of silent infarctions, while areas of leukoaraiosis and cerebral atrophy also occur in other neurodegenerative pathologies.
To detect etiological factors, consultation with a cardiologist and nephrologist, blood pressure monitoring, a coagulogram, determination of lipoproteins and cholesterol in the blood, and a blood sugar test are required.
Which doctor should I contact?
Discirculatory encephalopathy refers to neurological disorders. If alarming symptoms appear, you should consult a neurologist as soon as possible. The specialist will conduct an examination, make an accurate diagnosis and prescribe adequate treatment. The sooner help is provided, the more optimistic the prognosis for the patient
Get diagnosed with disculatory encephalopathy at Clinic No. 1:
- MRI
- Consultation with an ophthalmologist
- EEG, REG
- Ultrasound of vessels
- Duplex scanning
For one-time payment for services - 20% discount
Call
Therapy
The therapeutic approach to the treatment of encephalopathy should have an etiopathogenetic direction and be comprehensive. It is necessary to compensate for the primary disease, enhance microcirculation and cerebral circulation, and also protect the cells of the central nervous system from ischemia and hypoxia.
Etiotropic treatment of DEP includes the selection of hypoglycemic and antihypertensive drugs, which should be prescribed individually. An anti-sclerotic diet is also indicated. If cholesterol levels do not decrease even with dietary correction, appropriate medications are prescribed, such as gemfibrozil, lovastatin, probucol.
The basis of pathogenetic therapy is drugs that improve cerebral hemodynamics. It is important that they do not lead to the effect of stealing. These are calcium channel blockers such as flunarizine, nifedipine, nimodipine, as well as α2-adrenergic receptor antagonists, such as nicergoline or pyrobedil, and phosphodiesterase inhibitors: ginkgo biloba, pentoxifylline. Since DEP is often accompanied by increased platelet production, the patient needs lifelong use of antiplatelet agents, which include ticlopidine or acetylsalicylic acid. If the patient has contraindications, such as gastrointestinal bleeding or stomach ulcers, dipyridamole may be prescribed.
It is very important to take drugs with a neuroprotective effect, which allow neurons to function under conditions of chronic hypoxia. These include:
- Piracetam;
- GABA derivatives: gamma-aminobutyric acid, aminophenylbutyric acid, N-nicotinoyl-gamma-aminobutyric acid;
- Membrane stabilizing drugs: choline alfoscerate;
- Cofactors;
- Medicines of animal origin: porcine cerebral hydrolysate, hemodialysate from the blood of dairy calves, cortexin;
- Vitamin and mineral complexes.
If discirculatory encephalopathy is caused by a narrowing of the lumen of the internal carotid artery reaching seventy percent, it usually progresses very quickly and is accompanied by small strokes or episodes of PNMK. In such a situation, surgical intervention is indicated. It could be:
- Carotid endarterectomy for stenosis;
- Extra-intracranial anastomosis with complete occlusion;
- Reconstruction of the vertebral artery in case of damage.
Treatment
When treating pathology, complex etiopathogenetic therapy is used. It is aimed at compensating for the disease, normalizing blood circulation, protecting nerve cells from oxygen starvation and ischemia. Drugs are used to lower blood sugar levels, normalize blood pressure and cholesterol. Nutrition is adjusted and the patient is prescribed a special diet.
Surgery may be prescribed when the pathology is caused by a narrowing of the lumen of the artery, progresses quickly and is accompanied by serious complications.
Normalization of lipid metabolism is used as a preventive measure. Violation of this process leads to deposits on the inner surface of the vessels, which narrow the lumen and interfere with normal blood circulation. It is also important to fight atherosclerosis and maintain normal sugar levels in patients with diabetes.
Doctor's forecasts
With effective and timely therapy, the development of DEP at the first or second stage in most cases slows down. Occasionally, rapid development of the disease is observed, in which case each stage takes about two years. When dyscirculatory encephalopathy is combined with degenerative changes in the central nervous system, the prognosis is most often unfavorable. Hypertensive crises, ischemic or hemorrhagic strokes, TIA and other cerebrovascular accidents, and uncontrolled hypoglycemia that accompany the disease have a negative impact on the recovery process.
Diagnostics
A neurologist is involved in the diagnosis and treatment of encephalopathy. Patient examination includes:
- survey: collection of complaints and anamnesis; it is mandatory to clarify information about previous diseases, injuries, risk factors, the time of the first violations, the rate of development, etc.;
- neurological examination: assessment of reflexes, sensitivity, muscle strength, motor function;
- electroencephalography (EEG): assessment of electrical impulses arising during brain function; allows you to identify signs of epilepsy, inflammation, the presence of tumors, etc.;
- Doppler ultrasound of the vessels of the brain and neck: assesses the quality of blood flow in large vessels, identifies areas of narrowing, assesses the volume of incoming blood;
- rheoencephalography: complements ultrasound, allows you to assess the tone and elasticity of blood vessels, detect blood clots;
- angiography: X-ray examination of blood vessels by introducing a contrast agent into them;
- CT and MRI: allow you to detect foci of sclerosis, tumors, inflammatory foci, consequences of stroke and other structural changes;
- blood tests (general, biochemical): make it possible to evaluate the functioning of the kidneys, liver, pancreas, and identify toxins that can affect the condition of the brain.
If necessary, other tests and examinations may be prescribed, as well as specialist consultations to accurately determine the cause of encephalopathy.
Make an appointment
What aggravates the course and stimulates the progression of dyscirculatory encephalopathy?
The condition worsens when exposed to the following factors:
- Chronic and/or acute psycho-emotional stress (frequent stress at work or in the family, insufficient time to sleep, working without rest or at night).
- Hypokinesia (lack of dosed exercise and walks in the air).
- Obesity or overweight.
- Alcohol abuse and smoking.
- Diabetes mellitus, which causes inflammation of the inner walls of blood vessels.
- Dysfunction of the thyroid gland, causing disruption of metabolic processes in the body.
- Diseases of the cervical spine that impair blood flow in the vertebrobasilar region.
Predisposing factors that worsen the condition also include blood diseases (increased platelet levels or hematocrit), heart disease (rhythm disturbances) and vasculitis (vascular inflammation). Also to this list should be added congenital hypoplasia (narrowed diameter) of the cerebral arteries.
Symptoms and initial manifestations
Clinical symptoms have certain characteristics depending on the type of dyscirculatory encephalopathy. The development of vestibular-atactic, pseudobulbar, cephalic, and psychopathological syndromes is characteristic.
On examination, mild incoordination and symptoms of anisoreflexia are revealed, indicating a small focal brain lesion. This stage, in addition to diffuse, unexpressed neurological symptoms, is characterized by the presence of a syndrome reminiscent of the asthenic form of neurasthenia.
The main symptoms of the initial stage of DEP progression include:
- insomnia;
- unstable attention;
- increased fatigue;
- irritability;
- memory impairment;
- slight change in gait (instability, shortening of stride);
- decreased productivity of intellectual work.
Patients at stage I of dyscirculatory encephalopathy of the brain often complain of headaches and noise in the head, they are tearful, and their mood is often depressed. To diagnose the disease, complaints must appear at least once a week for three months, that is, last for a long time.
Treatment of DEP in the clinical hospital on Yauza
Comprehensive diagnostics allows specialists to prescribe adequate drug treatment. It should be aimed primarily at normalizing blood supply to the brain and blood pressure, correcting symptoms and preventing further damage to blood vessels and brain tissue. It is also important to use drugs that normalize the metabolism of brain cells and increase vascular tone.
In addition, neurologists at the Yauza Clinical Hospital offer each patient an individual complex of non-drug therapy, which includes reducing alcohol consumption, quitting smoking, and regular dynamic physical activity. It is also important to follow nutritional recommendations: limiting the consumption of table salt, saturated fats, sufficient consumption of potassium, magnesium and calcium salts, eating foods that improve the functioning of the circulatory system.
You can see prices for services in the price list or check by calling the phone number listed on the website.
Impact on key risk factors
Due to the high importance of recurrent strokes for the progression of motor and cognitive disorders in patients with DEP, a higher priority is the prevention of vascular complications. Correction of existing symptoms is secondary. In such patients, “aggressive” prophylaxis is necessary.
Antihypertensive therapy
Maintaining normal blood pressure levels can help prevent or slow the progression of DEP. Most often, in the presence of chronic cerebral circulatory failure, doctors recommend the use of drugs belonging to the groups of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. These medications are believed to have protective properties against the brain, blood vessels, heart and kidneys.
If these drugs are not enough to control blood pressure, they are combined with other drugs - diuretics, beta blockers, calcium channel blockers. Only a doctor can prescribe medications suitable for patients with DEP.
Correction of carbohydrate metabolism
There are no doubts about the cause-and-effect relationship between dysfunction of carbohydrate metabolism and the development of circulatory disorders in the brain. To correct the pathological process, an appropriate diet and medications that lower blood sugar levels are prescribed.
Lipid-lowering therapy - statins
Since the other main cause of DEP is cerebral atherosclerosis, patients with this disease are often prescribed drugs that lower blood cholesterol levels. The most commonly used drugs are statins, which in addition to lowering cholesterol levels also improve the condition of the inner layer of blood vessels (endothelium), reduce blood viscosity, stop or slow down the progression of atherosclerosis and have an antioxidant effect.
Antithrombotic therapy
One of the mandatory components of the treatment plan for patients with DEP. Antiplatelet agents affect platelets, preventing them from sticking together (aggregation), which improves cerebral circulation. Low-dose aspirin is most often prescribed.
Reduced homocysteine levels
Elevated levels of homocysteine (a sulfur-containing amino acid) are a risk factor for the development of vascular disease and dementia. To correct indicators, folic acid and B vitamins (B12, B2 and B6) are prescribed.
Healthy lifestyle and exercises for memory development
Bad habits, lack of physical activity and poor nutrition have an impact on the deterioration of cognitive functions over the years. This confirms the benefits of a healthy lifestyle in preventing the development of mixed and vascular dementia.
Thanks to the conducted research, it was possible to confirm the relevance of the concept of “cognitive reserve”. According to this concept, a healthy lifestyle significantly reduces the likelihood of developing dementia. Receiving higher education does not have any effect on the prognosis of the disease.
Dementia drugs
To reduce the severity of clinical symptoms in dementia, drugs are prescribed whose action is aimed at improving the transmission of signals between neurons through synapses. Active substances prevent neuron death: glutamate NMDA receptor antagonists and acetylcholinesterase inhibitors.
Antidementia drugs reduce the severity of behavioral (aggression, agitation) and cognitive (problems of attention, speech and memory) disorders. Medicines do not improve the general condition of the patient, but significantly slow down the rate of deterioration of symptoms.
Nootropic and vasoactive drugs
The use of vascular drugs to combat vascular lesions is unjustified. The effectiveness of the use of Ginkgo Biloba, ergot alkaloids and methylxanthines is controversial.
Physiotherapy
Complex therapy, which combines drug and non-drug methods of combating the disease, is more effective. Among the effective physiotherapeutic methods for treating DEP, the following should be highlighted:
- Exercise therapy (a set of exercises is prescribed individually by a doctor);
- transcranial magnetic stimulation;
- acupuncture;
- massage of the collar area;
- vortex fields;
- electromyostimulation.
Surgery
The need for surgery arises if the pathological process develops against the background of rapid progression of narrowing of the lumen. Surgery is also necessary if serious complications develop.
The following types of operations are widespread:
- Stenting. It involves inserting a special dilator into the vessel to improve blood flow in the part of the artery that has been narrowed.
- Carotid endarterectomy. It is carried out for atherosclerosis in order to cleanse the internal walls of the carotid artery.
Surgical intervention does not completely eliminate the disease, but it makes it possible to improve the patient’s condition and slow down the progression of the disease.
Spa treatment
With progressive organic changes in brain tissue that occur as a result of chronic vascular insufficiency, sanatorium treatment is recommended. This approach to therapy is possible only in the absence of pronounced changes in the psyche and deterioration of cerebral circulation. Such patients are sent to balneotherapeutic and climatic resorts with hydrogen sulfide and radon waters.
TREATMENT OF DISCIRCULATORY ENCEPHALOPATHY IS AVAILABLE IN THE BRANCHES:
Treatment of dyscirculatory encephalopathy in the Primorsky region
Address: St. Petersburg , Primorsky district, st. Repisheva, 13
Treatment of discirculatory encephalopathy in the Petrograd region
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
Treatment of dyscirculatory encephalopathy in Vsevolozhsk
Address: Vsevolozhsk , Oktyabrsky Prospekt, 96 A