Pathogenesis
The sexual transmission of syphilis is due to the rapid penetration of Treponema pallidum into the patient’s body through the mucous membrane.
Microscopic abrasions and cuts on the skin can be an excellent source of infection. Within a few hours, the bacterium penetrates the lymphatic system and blood, resulting in a systemic infectious process. The incubation period, which determines the duration of the latent period of the disease, lasts on average from 10 to 90 days. Modern research proves that treponema pallidum is sometimes found in the lymphatic system of an infected organism within 30 minutes after invasion. The infectious agent penetrates the central nervous system already in the early stages of syphilis. This is evidenced by abnormal results of examination of the cerebrospinal fluid of patients. If treatment is not carried out, the bacteria spread in the human body for 5-20 years after invasion and affect various internal structures. In later stages, treponema attacks the central nervous system, causing neurosyphilis. This form of the disease causes severe neurological and psychiatric complications.
The undulating course of syphilis is due to the gradual spread of the bacterium in the body and a change in the immune response. The human immune system does not have innate mechanisms of protection against the disease, so the production of antibodies does not contribute to the complete destruction of Treponema pallidum. As syphilis develops, the body's defense systems weaken, and already at the third stage of the pathology, practically no specific antibodies are detected in the patient's body.
Patient mistakes as a cause of relapse of syphilis
The patient's mistakes begin only after the doctor makes a mistake.
Namely, he will send a patient with syphilis home for treatment.
At home, a person can make many mistakes.
Basically they are the following:
- replacing an expensive drug with a cheap one because the pharmacy said it was “the same thing”
- refusal to use antibiotics due to personal belief that all diseases, including syphilis, can be treated with pickles, pine cones or propolis
- skipping injections due to lack of discipline
- use of incorrect doses (the name of the drug is the same as prescribed by the doctor, but the dose at the pharmacy was given differently)
- incorrect frequency of drug use (either I forgot how to inject, or did not consider it necessary to follow the doctor’s instructions in full)
- not all medications are purchased and used (the patient considers some medications important, but for some reason does not take others)
The most common mistake a patient makes is that he is not treated completely.
He tells the doctor that he continues to inject antibiotics.
But he refuses them because:
- symptoms have passed;
- the person considers himself healthy;
- fears the harm of antibiotics to health;
- the injections are painful, and there is no longer a living place on the “soft spot”;
- does not want to spend any more money on treatment.
All these factors combine.
Of course, if a person considers himself sick, he is ready to spend money on treatment and endure painful injections.
But if he believes that he has already been cured, and the doctor prescribes further injections just to be on the safe side, he can stop using the drugs.
Not in 100% of cases, but sometimes this results in relapses.
They can happen even several years after the end of therapy.
And all because the person was lazy or did not consider it necessary to complete the course, as a result of which a “handful” of bacteria remained in his body.
Causes of infection
In order to understand how you can become infected with syphilis, you need to familiarize yourself with the main signs of the causative agent of the disease. Treponema pallidum cannot remain viable in the environment for long, so the main routes of transmission of syphilis are through infected people. Only in rare cases does the infectious agent remain active in a humid environment while maintaining optimal temperature conditions.
Methods of infection
- Sexual intercourse. Bacteria are present in the patient's mucous membranes and are actively transferred to the tissues of another person. Even the smallest cuts in the genital area contribute to rapid invasion.
- Transfusion transmission is the penetration of an infectious agent into the patient’s body along with blood. This is a rare route of infection, mainly associated with drug addiction.
- Household transmission. In this case, bacteria can enter the new body through personal hygiene items.
- Infection of the fetus during pregnancy.
In addition to the known routes of infection, it is also necessary to take into account certain risk factors that significantly increase the likelihood of transmitting infection. In the case of syphilis, a high risk of infection is associated with promiscuity, drug addiction and pathologies of the immune system.
How does infection occur?
Among syphilidologists, there is an opinion that syphilis infection occurs exclusively through the “entry gate” (tears, wounds, scratches on the mucous membrane or skin), however, spirochetes can infect the body, penetrating even through minor injuries. Therefore, the skin and mucous membranes do not prevent the source of syphilis from entering the body.
Since the source of syphilis infection is its carrier, infection often occurs through interaction with it. For syphilis, the typical methods of infection are: sexual, household, blood transfusion, occupational and transplacental. At birth, a child can become infected with syphilis from the mother while passing through the birth canal. Breastfeeding also carries risks. Milk is infected even when patients have hidden symptoms of syphilis; it affects the child’s body from the first feeding. There is no innate immunity to syphilis. Almost any type of infection leads to the development of syphilis and damage to all vital systems of the body.
Periods of flow
As already mentioned, syphilis is characterized by a progressive course. Each stage of the disease has its own distinctive signs, so it is important for the doctor to take into account all external and laboratory signs of infection during diagnosis. Syphilis can develop over many years, so not all characteristic symptoms of the disease occur in individual patients. Late clinical manifestations of the pathology, characterized by severe damage to internal organs, are practically not diagnosed today, but even the early stages of infection can be dangerous.
Primary syphilis
The first stage of the disease develops immediately after the incubation period. Within a few weeks of infection, patients begin to show outward signs of syphilis. Hard ulcerations can form in the external genitalia, anus and oropharynx. In rare cases, chancre occurs in the area of the fingers and nipples. The ulceration itself is a dense, round formation ranging in size from 5 millimeters to several centimeters. Due to the lack of pain, chancre does not attract attention, but the formation of ulcers in the area of the lymphatic tissues of the nasopharynx can cause unpleasant sensations reminiscent of acute tonsillitis.
Possible symptoms:
- headache;
- discomfort in the oropharynx;
- periodic increase in body temperature;
- pain in joints and muscles;
- decreased mood.
Already at the first stage of the disease, bacteria begin to actively multiply in the lymph nodes, resulting in lymphadenitis in the patient. First of all, the lymph nodes located next to the chancroid become inflamed and enlarged, but gradually treponema pallidum spreads to distant lymph nodes. All of these changes, characteristic of primary syphilis, develop over two months.
Secondary syphilis
The second stage of the disease develops on average 3 months after infection and continues for several years. Secondary syphilis is characterized by damage to internal organs, tissues and individual systems of the body. The main external manifestations of this period of the disease are skin and mucous rashes. The undulating course of secondary syphilis causes periodic exacerbations. In this case, the stage of severe symptoms is replaced by a latent period, when the main manifestations of the infection disappear.
Possible symptoms:
- the appearance of pathological formations on the skin and mucous membranes (bright roseola, papules, plaques and ulcers);
- hair loss;
- headache;
- nausea and vomiting;
- lack of appetite;
- muscle weakness;
- increase in body temperature;
- weight loss;
- visual and hearing impairment.
Excessive rashes at this stage of the disease are caused by damage to small blood vessels. In patients suffering from HIV infection, a more severe form of secondary syphilis occurs, characterized by intoxication of the body, skin ulcers and a significant decrease in body weight.
Tertiary syphilis
In rare cases, patients are diagnosed with a terminal form of the disease, characterized by irreversible damage to internal organs and the central nervous system. The tertiary period of syphilis occurs many years after infection if the patient has not received the necessary treatment. At this stage of the disease, the immune system is no longer able to resist infection. Particularly characteristic signs of terminal syphilis are external deformities caused by the disintegration of skin nodules and mucous membranes.
Possible clinical manifestations and symptoms:
- Severe neurological disorders: paresthesia, irreversible hearing and vision impairment.
- Cognitive changes resembling complications of dementia. Primarily these are dementia and psychotic disorders.
- Pain in the chest and back, indicating the formation of an aortic aneurysm.
- Difficulty swallowing food and breathing.
- Speech disorder.
- Internal bleeding.
- Deformation of joints and soft tissues.
The terminal form of infection is preceded by a many-year latent period, during which there may be virtually no symptoms of the disease. In this regard, doctors must monitor the effectiveness of treatment for syphilis at all stages and prescribe laboratory tests for patients after undergoing therapy.
CLINICAL MANIFESTATIONS OF PRIMARY AND SECONDARY SYPHILIS
The paper provides a detailed account of the clinical manifestations of primary and secondary syphilis, such as hard chancre, scleradenitis, secondary syphilids. It briefly characterizes visceral abnormalities, osteoarticular and nervous changes. Particular emphasis is laid on rare forms of hard chancre, which have recently occurred, and on the clinical features of primary and secondary syphilis of today and in the presence of HIV infection.
A.V. Samtsov - prof., doctor of medicine. sciences, head Department of Skin and Sexually Transmitted Diseases, Military Medical Academy, St. Petersburg.
AV Samtsov - prof., MD, Head of Dermatology and Venerology Department, MMA, S.-Petersburg.
Primary syphilis
The primary period of syphilis is characterized by the development of chancre, regional scleradenitis and polyadenitis. The duration of the primary period is approximately 7 weeks. Its first half (the so-called primary seronegative syphilis) is characterized by negative results of the Wasserman reaction. After 3–4 weeks, the reaction becomes positive, and syphilis becomes seropositive. At the same time, polyadenitis develops, but in recent years in some patients it has been slightly expressed. The primary period of syphilis begins with the formation of chancre at the site of inoculation of pale treponema. In 90–95% of cases, genital localization is noted, but currently the frequency of extragenital chancre is increasing. The founder of syphilidology A. Fournier identified 9 signs of chancroid, the most typical of which are the following: manifestation in the form of painless erosions or ulcers with a smooth, even bottom the color of raw meat or spoiled lard, the absence of inflammatory phenomena, the presence of compaction at the base upon palpation. Hard chancre usually has a diameter of 10–20 mm, but so-called dwarf chancre (2–5 mm) and giant chancre (40–50 mm) are also found. Dwarf chancre is observed somewhat more often in women. Giant chancres are usually localized on the pubis, abdomen, scrotum, inner thighs, chin, and forearms. At the present stage, hard chancrees often occur as erosive balanoposthitis or balanitis, sometimes in the form of small scratches with mild infiltration, dwarf chancrees and giant chancrees with gangrenization, phagedenism are relatively common (see below), often there is no infiltrate at the base, more often steel there are multiple chancres. In addition, even in classical cases, chancre has features depending on the location: on the frenulum of the penis they take on an elongated shape and bleed easily during erection; on the sides of the frenulum they are poorly visible and have practically no compaction; The chancre of the urethral opening is always hard and bleeds easily; when the chancre is localized in the urethra, slight pain is noted, especially during palpation, which should be carried out from front to back, since induration cannot be felt from the sides. In women, the chancres in the area of the opening of the urethra are always dense, while in the chancres of the vulvovaginal fold the compaction is not pronounced. Vaginal chancre is extremely rare. With extragenital localization, in 75% of cases, chancre occurs in the head area: in the oral cavity, on the face, and very rarely on the scalp. The second place among extragenital chancres is occupied by chancres of the upper extremities (7%), the third place is taken by chancres in the anus area (6.8%), the fourth place is in the area of the mammary glands (5%). Chancres of the lips, localized, as a rule, on the red border, in 95% of cases are single and covered with a crust; The lower lip is most often affected. The chancre of the tongue is represented by erosion or ulceration, but rare forms are found - slit-like or stellate (along the fissure of the tongue). The tonsil chancre was first described by Diday (1861) and then studied in detail by Legendre (1884). Chancres of the tonsils are represented by erosions or ulcers; in rare cases, chancre amygdalitis occurs, characterized by thickening and enlargement of the palatine tonsil without the formation of erosion and ulcers, but accompanied by pain and difficulty swallowing. Chancres of the gums, hard and soft palate, and pharynx are extremely rare. The first description of eye chancre was made by Ricor in 1850, highlighting chancre of the ciliary margin, eyelid and conjunctiva. Of the extragenital chancres, chancres of the hands deserve special attention. They are observed more often in men, mainly on the right hand; in 84% the process is localized on the fingers - index, middle and thumb. Chancre-felon is found; the finger becomes bluish-red, swollen, club-shaped, swollen, patients experience sharp, “shooting” pains, on the dorsal surface of the phalanx there is an ulcer with a bottom covered with necrotic-purulent discharge. The chancre around the anus looks like a “gathered” chancre or chancre in the form of a crack. Chancres of the rectum are manifested by pain in the rectum shortly before and some time after defecation, as well as glassy stool. Special varieties of hard chancre include: 1) burn (combustioform), which is an erosion prone to pronounced peripheral growth with weak compaction at the base; as erosion grows, its boundaries lose their correct outlines, the bottom becomes red and granular; 2) Vollmann's balanitis is a rare type of primary syphiloma, characterized by many small, partially merging, sharply limited erosions without noticeable compaction at the base of the glans penis or on the external genitalia in women; 3) herpetiform chancroid, reminiscent of genital herpes. Complications of chancre are represented by balanitis, balanoposthitis, inflammatory phimosis, paraphimosis, gangrenization and phagedenism. Inflammatory phenomena usually occur due to poor hygiene. Gangrenization develops mainly with the addition of fusospirillosis infection. In this case, necrosis is observed and a black scab forms on the surface of the chancre. General phenomena are often observed. Phagedenism is characterized by the spread of necrosis deep into and beyond the chancre (according to Ricor, the chancre devours itself). Necrosis can lead to rejection of the glans penis, severe bleeding, perforation and destruction of the urethra. Regional scleradenitis, as Ricor puts it, “is a faithful companion of chancre, accompanies it invariably and follows it like a shadow.” A. Fournier did not detect regional scleradenitis in only 3 out of 5000 patients. Scleradenitis develops on the 5th – 7th day after the appearance of chancroid and is characterized by painlessness, absence of inflammatory phenomena, and woody density. Usually a group of lymph nodes enlarges at once, but one of them is larger. However, it should be noted that recently the simultaneous appearance of scleradenitis with chancre has sometimes been noted. Differential diagnosis of chancroid is carried out with the following diseases: balanitis and balanoposthitis, genital herpes, chancriform pyoderma, gonococcal and trichomonas ulcers, soft chancroid, scabies ecthyma, tuberculous ulcer, diphtheria ulcers, acute vulvar ulcer, fixed toxicerma, lymphogranulomatosis venereum, Keir's erythroderma, plasmacytic balanoposthitis, squamous cell skin cancer. Differential diagnosis is based on the characteristics of the clinical picture, medical history, detection of Treponema pallidum and the results of serological reactions. Prodromal phenomena occur in some patients 7–10 days before the end of the primary period and are characterized by weakness, malaise, headache, pain in muscles, joints, bones, fever, however, even at high temperatures, patients feel quite satisfactory. These phenomena are associated with massive dissemination of Treponema pallidum through the thoracic lymphatic duct into the subclavian vein, which leads to septicemia. It should be emphasized that the primary period ends with the occurrence of secondary syphilides, and not with the resolution of chancre.
Secondary syphilis
Clinical manifestations of the secondary period of syphilis are characterized mainly by damage to the skin and visible mucous membranes and, to a lesser extent, changes in internal organs, the musculoskeletal system and the nervous system. Skin manifestations of the secondary period (secondary syphilides) are varied: spotted, papular, vesicular, pustular. There is no area on the skin and mucous membranes where secondary syphilides could not appear. All secondary syphilides have the following common features: 1. A peculiar color. Only at the very beginning do they have a bright pink color. Subsequently, their color acquires a stagnant or brownish tint and becomes faded (“boring,” in the figurative expression of French syphilidologists). It can also be red, cherry, copper-red, yellowish-red, bluish-red, pink, pale pink, yellowish-pink, depending on the location. 2. Focus. Without a pronounced tendency towards peripheral growth, the elements of syphilitic rashes usually do not merge with each other and do not look like a continuous lesion, but remain delimited from each other. 3. Polymorphism. There is often a simultaneous eruption of various secondary syphilids, for example, macular and papular or papular and pustular (true polymorphism), or there is a variegation of the rash due to the gradual appearance of elements at different stages of development (evolutionary or false polymorphism). 4. Benign course. As a rule, secondary syphilides, excluding rare cases of malignant syphilis, resolve without leaving scars or any other permanent traces; their rash is not accompanied by disturbances in the general condition and subjective disorders, in particular itching, a common symptom in various skin diseases. 5. Absence of acute inflammatory phenomena. The skin and mucous membranes around the syphilides are usually not hyperemic or swollen. 6. Rapid disappearance and resorption of syphilides under the influence of specific therapy. 7. Extremely high infectiousness of secondary syphilides, especially eroded and ulcerated ones. The first rash of the secondary period (secondary fresh syphilis) is characterized by an abundance of rash, symmetry, small size of elements, brightness of color, remnants of the primary affect, regional adenitis and polyadenitis. With secondary recurrent syphilis, the rashes are often limited to individual areas of the skin, tend to group, form arcs, rings, garlands, the number of elements decreases with each subsequent relapse. However, in recent years, secondary syphilis often develops in the absence of chancre, and in these cases there are often no reliable clinical criteria for distinguishing fresh and recurrent syphilis. In this regard, many authors consider it inappropriate to divide the secondary period into fresh and recurrent. Spotted syphilide is represented by syphilitic roseola and occurs in 75–80% of patients in the secondary period. “Fresh” roseola appears after the end of the primary period, approximately 10 weeks after infection or 6–8 weeks after the appearance of chancre. Roseola is a hyperemic spot, the color of which ranges from barely noticeable pink (peach color) to rich red, morbilliform, but most often it is pale pink, “faded.” Due to evolutionary polymorphism, roseola may have a different pink hue in the same patient. When pressure is applied, roseola completely disappears, but when the pressure stops, it appears again. Diascopy of roseola, which has existed for about 1.5 weeks, reveals a brownish color caused by the breakdown of red blood cells and the formation of hemosiderin. The outlines of roseola are round or oval, indistinct, as if finely torn. The spots are located isolated from each other, focally, and are not prone to merging and peeling, however, cases of scaly roseola have been described. Roseola does not differ from the surrounding skin in either relief or consistency; there is no peeling even during resolution (which distinguishes it from the inflammatory elements of most other dermatoses). The size of roseola ranges from 2 to 10 – 15 mm. Roseola becomes more pronounced when the human body is cooled with air, as well as at the beginning of treatment of the patient with penicillin (in this case, roseola may appear in places where they were not present before the injection) and when the patient is given 3–5 ml of a 1% solution of nicotinic acid (the “inflammation” reaction) ). It is clearly visible when the skin is irradiated with Wood's rays in a dark room. Recurrent roseola appears within a period of 4–6 months from the moment of infection to 1–3 years. Roseola is rarely observed on the genitals and is hardly noticeable. It occurs very often in the oral cavity; the spots are located isolated or merge into continuous areas in the area of the soft palate and tonsils. Such syphilitic erythematous anginal (angina syphilitica erythematosa) rashes, red in color with a bluish tinge, appear sharply demarcated from the normal mucous membrane; the lesion does not cause subjective sensations or they are very insignificant, is not accompanied, with rare exceptions, by general phenomena and an increase in temperature, and can be either unilateral or bilateral. Often papular, erosive-ulcerative syphilides appear simultaneously in the oral cavity, on the mucous membrane of the larynx and vocal cords. As a result of swelling of the mucous membrane in these cases, the glottis narrows and hoarseness appears. The following clinical varieties of roseola are also relatively rare: rising (elevation) roseola (roseola elevata), synonym – urticarial roseola (roseola urticata); papular roseola (roseola papulosa); exudative roseola (roseola exudata), it differs from a blister in the absence of itching and the duration of its existence. This roseola is typical only for the fresh form. Ordinary roseola acquires an elevated character after the first injections of the antibiotic, which is regarded as a positive Herxheimer reaction. Follicular, or granular, roseola (roseola granulata, roseola follicularis) is distinguished by the presence of small dotted granularity on the surface of the spot, due to the severity of the follicular pattern. Exists for a long time (from 2 weeks to 2 months), resolves without leaving a trace. Confluent roseola (roseola confluens) is formed due to the fusion of individual spots with a very heavy rash or with irritation of individual areas of the skin. Differential diagnosis of roseola syphilide is carried out with the following dermatoses: spotted toxicerma, pityriasis rosea, “marbled” skin, pityriasis versicolor, spots from plodder bites, rubella, measles. Papular syphilide is represented by a dermal papule, formed due to the accumulation of cellular infiltrate in the upper parts of the dermis. Papules are clearly demarcated from the surrounding skin, their outlines are round or oval. The shape of the papules is hemispherical or pointed. They have a dense consistency, are located, as a rule, in isolation, but when localized in folds and irritation, they tend to grow peripherally and merge. In some cases, growing peripherally, papules dissolve in the center, which leads to the formation of various shapes. The surface of fresh papules is smooth with a smoothed skin pattern, shiny. Their color ranges from soft pink to brownish-red (copper) and bluish-red. As the papules resolve, they may become covered with scales. Under unfavorable conditions, they are subject to erosion and ulceration; sometimes they vegetate and hypertrophy (condylomas lata). Papular syphilides exist for 1–2 months, gradually resolve, leaving behind brownish pigmentation. Depending on the size of the papules, miliary, lenticular, nummular, and plaque-like papular syphilides are distinguished. In addition, syphilitic papules differ in the nature of their surface and location. Lenticular (lenticular) papular syphilide (Syphilis papulosa lenticularis) is the most common type of papular syphilide, which occurs both in the secondary fresh and in the secondary recurrent period of syphilis. A lenticular papule is a rounded nodule with a truncated apex (“plateau”), with a diameter of 0.3 to 0.5 cm, red in color. The surface of the papule is smooth, shiny at first, then covered with thin transparent scales, characteristic peeling of the “Biette collar” type, while the scales frame the papule along its circumference like a delicate fringe. But peeling can be wafer-type, as with parapsoriasis. With secondary fresh syphilis, a large number of papules are found on any part of the body, often on the forehead (corona veneris). On the face, in the presence of seborrhea, they are covered with greasy scales (papulae seborrhoicae). With secondary recurrent syphilis, papules are grouped and form bizarre garlands, arcs, rings (syphilis papulosa gyrata, syphilis papulosa orbicularis). Differential diagnosis of lenticular syphilide is carried out with the following dermatoses: guttate parapsoriasis, lichen planus, vulgar psoriasis, papulo-necrotic tuberculosis of the skin. Miliary papular syphilide (Syphilis papulosa milliaris seu lichen syphiliticum) is characterized by dermal papules, 1–2 mm in diameter, located at the mouth of the hair follicles. The nodules have a round or cone-shaped shape, a dense consistency, and are covered with scales or horny spines. The color of the papules is pale pink, they stand out faintly against the background of healthy skin, and are localized on the trunk and limbs (extensor surfaces) in the area of the hair follicles. Often, after resolution, a scar remains, especially in people with reduced body resistance. Some patients are bothered by itching; Elements resolve very slowly, even under the influence of treatment. Miliary syphilide is considered a rare manifestation of secondary syphilis. Differential diagnosis must be carried out with lichen scrofuls and trichophytids. Monetoid (nummular) papular syphilide (Syphilis papulosa nummularis, discoides) manifests itself as a somewhat flattened hemispherical dermal papule measuring 2 - 2.5 cm or more. The color of the papules is brownish or bluish-red, round in outline. Coin-shaped papules usually appear in small numbers in patients with secondary recurrent syphilis, often grouped and combined with other secondary syphilides (most often with lenticular papules, less often with roseola and pustular syphilides). When coin-shaped papules dissolve, pronounced pigmentation remains, and sometimes cicatricial atrophy of the skin. There are cases in which there are many small papules around one coin-shaped papule, which resembles an exploding shell - blasting syphilide, corymbiform syphilide (syphilis papulosa corimbiphormis). Even less common is the so-called cockade syphilide (syphilis papulosa en cocarde), in which a large coin-shaped papule is located in the center of a ring-shaped one or is surrounded by a rim of infiltrate from fused small papular elements. In this case, a small strip of normal skin remains between the central papule and the rim of the infiltrate, as a result of which the element resembles a cockade. Very rarely, papules merge into plaques (syphilis papulosa en nappe). Papules in areas of the skin with increased humidity and sweating (genital organs of men and women, perineum, anus, between the toes, armpits, under the mammary glands in women, on the neck in obese subjects) change their appearance: their surface is macerated, becomes wet, the color becomes whitish - weeping papular syphilide (syphilis papulosa madidans) appears. This is the most contagious type of papular syphilide. As a result of friction, the stratum corneum is torn away, which leads to the formation of an erosive papule (syphilis papulosa erosiva); in the case of a secondary infection, an ulcerative papule (syphilis papulosa erosiva ulcerosa) is formed. In places of friction, especially in the anus, perineum, on the genitals, weeping papules increase in size, hypertrophy, vegetate and turn into vegetative papules or condylomas lata (syphilis papulosa vegetans, condilomata lata). The presence of vaginal discharge may also contribute to this. Some papules, growing along the periphery, form plaque-like syphilide. Its outlines are scalloped and repeat the outlines of fused papules. Palmar and plantar syphilides have a unique clinical picture. In these cases, the papules are only visible through the skin in the form of red-brown, if resolved - yellowish, clearly defined spots, surrounded by a Biette's collar. Sometimes horny papules are observed on the palms and soles, which are very reminiscent of calluses, sharply demarcated from healthy skin. Papular syphilide of the mucous membranes. Papular syphilide, as a rule, does not occur on the mucous membranes of the vagina and cervix. Syphilitic papules on the mucous membrane of the oral cavity, especially along the line of closure of the teeth and nose, appear in the form of dense, round, painless elements, sharply delimited from the normal mucous membrane and slightly rising above it. Their surface is smooth and whitish in color. Rarely, papules merge into plaques, become eroded, and are complicated by secondary infection. When papules are localized on the vocal cords or larynx, syphilitic dysphonia (rausedo) occurs, which in rare cases turns into complete aphonia. Pustular syphilides are a rare manifestation of secondary syphilis. According to various authors, the frequency of pustular syphilides ranges from 2 to 10%, and they occur in weakened patients. The following clinical manifestations of pustular syphilides are distinguished: acne (acne syphilitica), impetigo (impetigo syphilitica), smallpox (varicella syphilitica), syphilitic ecthyma (ecthyma syphiliticum), syphilitic rupee (rupia syphilitica). In differential diagnosis with dermatoses, with which pustular syphilides are similar, an important criterion is the presence of a clearly demarcated ridge of copper-red infiltrate along the periphery of pustular syphilides. Herpetiform (vesicular) syphilide (Herpes syphiliticus, syphilis vesiculosa) is an extremely rare manifestation of severe secondary fresh syphilis, in its pathogenesis close to pustular syphilide, and in its histological changes in the skin - to tubercular syphilide of tertiary syphilis. Vesicular syphilide indicates an unfavorable course of syphilis and is often combined with a disturbance in the general condition of the patient; its development is facilitated by the presence of concomitant chronic diseases or alcoholism. Syphilitic alopecia is represented by the following varieties: diffuse (alopecia syphilitica diffusa), small focal (alopecia syphilitica areolaris) and mixed (alopecia syphilitica mixta). The skin with small focal alopecia is not inflamed, does not peel, does not itch, and the follicular apparatus is preserved. Eyebrows and eyelashes are affected. Hair loss on the eyebrows in the form of small patches of baldness is so typical of syphilis and an incomparable symptom that this gave rise to calling it “omnibus” (Fournier), and then “tram” (P.S. Grigoriev) syphilide. The damage to the eyelashes is characterized by gradual loss and successive regrowth, as a result of which the eyelashes are of unequal length: next to normal eyelashes you can see short ones (stepped eyelashes - Pincus sign). Fine focal alopecia is figuratively compared to “moth-eaten fur.” Differential diagnosis of alopecia must be carried out with alopecia of seborrheic origin, alopecia after infectious diseases, alopecia areata, superficial trichophytosis, microsporia, favus, early baldness, discoid and disseminated lupus erythematosus, lichen planus. Syphilitic leukoderma was first described by Hardy (1854) under the name “pigmented syphilide”. In 1883 Neisser gave the modern name. Leucoderma is a characteristic symptom of secondary recurrent syphilis, so characteristic that old syphilidologists called leucoderma “the protocol of a positive Wasserman reaction, inscribed on the patient’s neck.” Currently, syphilitic leukoderma can also be found with secondary fresh syphilis. Leucoderma exists for a long time (months, years), but cases of its disappearance after a few days have been described. This “mystery” of this syphilide is also aggravated by the fact that no one has yet been able to detect pale treponema in the affected tissue. Syphilitic leukoderma is also characterized by resistance to specific therapy. Leukoderma is considered a manifestation of syphilis associated with damage to the nervous system and caused by trophic disorders in the form of impaired pigment formation (hyper- and hypopigmentation). It cannot be considered accidental that in the presence of leukoderma, patients, as a rule, also experience pathological changes in the cerebrospinal fluid. Syphilitic leukoderma occurs more often in women on the neck (“necklace of Venus”), especially on its lateral and posterior surfaces. Cases of localization of leukoderm on the body, back, lower back, limbs are described. At first, hyperpigmentation of pale yellow appears, which then intensifies and becomes more noticeable. Further, depigmented spots of rounded outlines appear on a hyperpigmented background. The spots are insulated (spotted shape), can merge (“lace” and “marble” shape). The leukoderm is not peeling, there are no inflammation and subjective disorders. Differential diagnostics must be carried out with pseudo -dolacderm after solar irradiation in patients with bran are lichen, vitiligo, plaque parapsoriasis, and cicatricial atrophy. It should be noted that in recent years the following features of the course of syphilis in the secondary period have been noted: an increase in the number of patients with palmar-siphylids, pustular rashes, atypical roseols characterized by peeling and fusion; Itching is often noted; weakly expressed polyadenitis; Early relapses are observed, similar to both secondary fresh and secondary recurrent; Malignant forms have become more frequent in secondary relapse syphilis. Syphilitic lesions of the internal organs with early syphilis are inflammatory and can be observed in any internal organ, but syphilitic hepatitis, gastritis, nephrosonephritis and myocarditis are most common. In most cases, visceropathy is not clinically expressed, in addition, they do not have pathognomonic signs, which leads to a sufficiently large number of diagnostic errors. Syphilitic lesions of bones and joints can be observed at the end of the initial period, but more often develop in the secondary and are usually limited to pain. Night pain in the bones are characteristic, more often in the long tubular bones of the lower extremities, as well as arthralgia in the knee, shoulder and other joints. Predeostites, osteoperiostitis and hydrarthrosis are less common. Syphilitic lesions of the nervous system in the early forms of syphilis are characterized by the involvement of the central nervous system mainly in the form of hidden, asymmetric meningitis, vascular lesions (early meningovascular neurosyphilis) and vegetative dysfunctions. In conclusion, it should be noted that at present syphilis is often developing against the background of HIV infection, which leads to the following features of its course: the rapid development of the disease up to late manifestations in a short time, a large proportion of rare, atypical and severe forms, absolute predominance in The secondary period of papulent forms, ulcerative chancro are prone to complications up to gangstones and phagedenism, an unusually large number of pale treponema in the separated chacks and erosive papules.
Literature:
1. Fournier Alfred. The doctrine of syphilis: Trans. from French – St. Petersburg. – 1903. – T.1. – 254 p. 2. Fournier Alfred. The doctrine of syphilis: Trans. from French – St. Petersburg. – 1903. – T.2. – 523 p. 3. Venereal diseases. Guide for doctors // Ed. OK Shaposhnikova. – Ed. 2nd, revised and additional – M.: Medicine. – 1991. – 554 p. 4. Skin and venereal diseases. Guide for doctors. In 4 volumes. – T.4 // Ed. Yu.K. Skripkina. – M.: Medicine. – 1996. – 352 p. 5. Pavlov S.T., Shaposhnikov OK, Samtsov V.I. and others. Skin and venereal diseases. – M.: Medicine. – 1985. – 364 p. 6. A.N. Rodionov. Syphilis. Guide for doctors. – St. Petersburg: Peter, 1997. – 284 p.
Congenital syphilis
Penetration of Treponema pallidum from the mother's body into fetal tissue can lead to irreversible morphological changes. Manifestations of congenital syphilis can be divided into early complications that occur within two years after the birth of a child, and late pathological changes. As a rule, doctors are unable to eliminate damage that has already occurred due to infection, so congenital syphilis often becomes a cause of disability.
Main clinical manifestations:
- diffuse rash on various areas of the skin. (Rashes are present in the mouth, on the palms and in the anus);
- extensive peeling of the epithelium;
- increased size of the liver and spleen;
- anemia and lymphadenopathy;
- deafness;
- yellowing of the skin and mucous membranes;
- decrease in the number of platelets in the blood;
- inflammation of the cornea of the eye;
- abnormal development of dental tissue.
In general, the congenital form of syphilis is easy to diagnose. Treating the infection early helps prevent more severe complications from developing in the future.
Malignant syphilis
If a syphilitic infection returns after therapy, it may develop a malignant form.
The cause can be either relapse or reinfection (re-infection).
The resulting hard chancre is prone to necrosis and peripheral growth.
The initial period in case of infection lasts only 3-4 weeks, and then a rash appears on the body.
In addition to spots, rupee, ecthyma, and impetigo (pustular syphilide) appear.
The eruptions become ulcerated.
Serological tests may be negative.
But they become positive after the start of penicillin therapy.
General symptoms of relapse of syphilis appear if it occurs in a malignant form:
- fever
- weakness
- intoxication
The disease does not go into a latent state for months.
If this happens, remissions are very short.
Clinical relapses follow one after another.
Diagnostics
An infectious disease can be detected by a venereologist, gynecologist or a doctor of another specialization. During the initial appointment, the specialist will conduct a physical examination to detect the most characteristic signs of the disease and collect medical history. If syphilis is suspected, the patient will be given a referral for laboratory tests. Currently, there are several reliable ways to diagnose the disease.
Basic diagnostic methods:
- Blood and cerebrospinal fluid testing to identify specific and nonspecific markers of infection. First of all, these are antibodies that are present in the patient’s body for many years after infection.
- Microscopic examination of skin formations as an additional diagnosis. The reliability of this method is inferior to other tests.
- Examination of internal organs and the central nervous system to identify complications of the disease.
The patient can donate blood and receive test results within a few days. In the laboratory, specialists carry out diagnostics using the anticardiolipin test, the Wasserman reaction and specific studies aimed at identifying bacterial antigens. All laboratory search methods are divided into preliminary (screening) and confirmatory studies.
The doctor selects a specific examination method based on the expected stage of syphilis and diagnostic purposes. Some specific tests reliably detect the disease even during the incubation period, while nonspecific serological tests are more often used to monitor the results of treatment.
Secondary recurrent syphilis
A syphilitic infection whose symptoms have returned is considered recurrent.
It can be either treated or untreated.
If a person has not received therapy, recurrent symptoms are considered a clinical relapse.
This occurs on average six months after infection.
Relapses do not occur in everyone, but only in 25% of patients.
If a year has passed since the infection and symptoms have not returned, the risk of their recurrence is low.
If 5 years have passed, there will be no recurrence of secondary syphilis with an almost 100% guarantee.
Secondary recurrent syphilis has some features in the clinical picture.
For example, roseolas look different.
With fresh syphilis they are small and randomly located.
Moreover, they are symmetrical and multiple.
Located on the stomach and lateral surfaces of the body.
Often appear along skin tension lines.
While with recurrent syphilis, roseola is large.
There are much fewer inflammatory elements, they are located asymmetrically.
They often group or merge to form various shapes.
The color may change: roseola of recurrent syphilis turn pale, sometimes on the contrary, the pigmentation is more pronounced.
However, the most important thing in the differential diagnosis of fresh and recurrent secondary syphilis is precisely the tendency to group, and not size or color.
Treatment
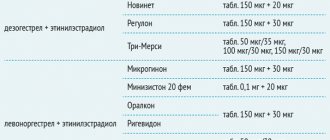
Drug therapy is selected individually after accurate laboratory confirmation of syphilis. Of the variety of antimicrobial drugs, doctors most often prescribe water-soluble penicillins to patients. Despite decades of use of penicillin derivatives as antibacterial therapy, Treponema pallidum has not acquired resistance to these drugs. The treatment regimen is selected in such a way as to maintain the optimal concentration of the drug in the patient’s blood. If an allergic reaction to penicillin derivatives is detected, the doctor selects other medications.
Other treatment options:
- Doxycycline. This antibiotic is an excellent alternative to penicillin derivatives and is suitable for the treatment of early and late latent syphilis.
- Erythromycin, tetracycline derivatives and cephalosporins when bacterial resistance to penicillin is detected.
- Derivatives of bismuth and arsenic in the tertiary form of infection. These are highly toxic drugs prescribed only after hospitalization.
To select therapy, it is advisable to contact a specialized clinic. During the consultation, the doctor will explain the treatment regimen to the patient, indicate the dosage of medications and the regimen. When using antibiotics, it is important to take your medications regularly. Self-treatment of syphilis is unacceptable due to the risk of developing dangerous complications.
Treatment of recurrent syphilis
If a relapse is detected, additional treatment is prescribed.
The use of durable penicillins is unacceptable for him.
Only drugs of medium duration or soluble penicillins are used.
Patients are treated in a hospital.
The best regimen for additional treatment:
- benzylpenicillin sodium 1 million units, every 4 hours;
- course of therapy is 20 days.
Outpatient treatment is used much less frequently.
In such situations, procaine penicillin is used.
It is administered in a similar course, once a day, 1.2 million units.
For allergies to penicillins, ceftriaxone is used.
The course of treatment is 10 days.
Dosage – 1 gram, 1 time per day.
Complications
The course of syphilis negatively affects the condition of all organs and tissues, so untimely treatment can lead to serious negative consequences. Typically, doctors separately consider visceral and neurological complications of the disease. Neurosyphilis, characteristic of the secondary and tertiary periods of the disease, has early and late manifestations. The most severe forms of damage to the central nervous system occur 10-15 years after infection of the body. At the same time, due to the transition of the infection to a latent form, some patients stop treatment, as a result of which late neurosyphilis occurs.
Complications of late neurosyphilis and visceral syphilis:
- Damage to skeletal muscles, manifested by impaired voluntary movements.
- Deterioration of intellectual abilities, memory impairment.
- The emergence of psychotic disorders.
- Irreversible loss of vision and hearing.
- Syphilitic damage to the meninges (meningitis).
- The appearance of external deformities.
- Membranous glomerulonephritis.
- Severe damage to the cardiovascular system.
The prolonged course of syphilis is accompanied by a significant deterioration in the quality of life. After treating a disease of the secondary or tertiary period, the patient will require long-term rehabilitation to eliminate secondary diseases. It is important to understand that the development of disability may be the price of a careless attitude towards one’s own health.
What is clinical relapse of syphilis?
Relapse is usually called the return of the disease after treatment.
But there is also the concept of clinical relapse.
This is the return of symptoms in a patient who has not received treatment.
The secondary and tertiary periods sometimes proceed in waves.
They distinguish two clinical periods, alternately replacing each other:
- latent phase
- clinical relapse
During the latent phase there are no symptoms.
They appear in the relapse phase.
These may be rashes, central nervous system lesions, etc., depending on the stage of the disease.
Forecast
Prognostic data depends on many factors, including the identified stage of the disease, timeliness of treatment and the presence of additional diseases. Modern methods of therapy make it possible to eliminate the pathological condition before bacteria cause damage to internal organs, but in this case it is necessary to rely on timely diagnosis and screening studies. If the disease is detected, the patient must inform all sexual partners about the need for treatment.
Conditions that may negatively affect the prognosis:
- Transition of the disease into a latent form.
- Late or incomplete treatment.
- Tertiary form of syphilis with damage to internal organs and the nervous system.
- The presence of HIV infection in the patient.
- Old age of the patient.
- Congenital pathologies of the immune system.
As practice shows, early neurosyphilis develops much faster in patients suffering from HIV infection. It is imperative to inform the doctor about concomitant diseases in order to correctly select drug therapy.
Causes of relapse of syphilis
Syphilis can be fresh or recurrent.
Recurrent can be treated or untreated.
If a person has manifested secondary syphilis, after a few months the symptoms disappeared, but after a certain time they appeared again - this is a relapse.
If the patient underwent treatment, normalization of serological parameters was observed, but then tests again showed an increase in antibody titer - this is also a relapse, but serological.
It can be difficult to distinguish from reinfection.
That is, from re-infection with a syphilitic infection.
For differential diagnosis, several different antibody tests are performed.
In particular, the determination of immunoglobulins M is informative.
Causes of relapse of syphilitic infection:
- weak immunity, HIV
- inadequate treatment
- long-term syphilis
- transition of the pale spirochete into special forms
Prevention
All sexually transmitted diseases are highly preventable. There is currently no vaccine against syphilis, but following certain rules will allow anyone to avoid infection. First of all, preventive recommendations concern sexual relations.
Rules that can be followed to avoid infection.
- Protected sex. Using a condom will prevent bacterial invasion in most cases.
- Avoiding casual sex. Having sex with one partner can significantly reduce the risk of infection.
- Strict hygiene when living with a person suffering from syphilis. Household transmission of the disease is unlikely, but long-term cohabitation may become an additional risk factor.
A person may not even realize that an infection has already been developing in his body for many years. This development of events is facilitated by promiscuity and hidden forms of the disease. In this regard, doctors recommend undergoing screening examinations aimed at identifying asymptomatic diseases. Screening for syphilis is, first of all, necessary for pregnant women, since this pathology can have an extremely negative impact on the condition and development of the fetus.
Incorrect treatment as a cause of relapse of syphilis
Relapse occurs often after treatment.
It can occur both through the fault of the doctor and the patient.
If a non-specialized specialist takes on the treatment of a syphilitic infection, he may prescribe the wrong treatment regimen.
Only a venereologist or syphilidologist should do this.
The following treatment features reduce the risk of relapse:
- therapy takes place in a hospital
- Intermediate or short-acting penicillins are used
- the doses are sufficient
- the course duration is sufficient
- there may be several courses
- there may be more than one antibiotic
Errors that can lead to incomplete destruction of bacteria and subsequent relapse:
1. Treatment of late stages of syphilis at home.
Patients should be hospitalized in a hospital.
In extreme cases, this could be a day hospital, where the patient comes daily to receive injections and the necessary medical procedures.
Drugs for the treatment of syphilis are used in injections.
Patients at home without medical supervision can:
- do not give injections;
- buy an alternative drug in tablets and not tell the doctor about it;
- giving injections incorrectly;
- do not administer the entire dose;
- forgetting to give an injection from time to time;
- not being treated completely, etc.
Outpatient 100% control of treatment is not provided.
While in a hospital, the doctor can be sure that the patient has received the full dose of the required antibiotic.
2. Use of one antibiotic.
This is acceptable in the initial stages of syphilis.
But in “experienced” patients, 2 drugs with different mechanisms of action are often used.
The first drug is one of the forms of benzylpenicillin, which the doctor considers appropriate in this particular clinical case.
The second is an antibiotic of a different group, for example, a macrolide or tetracycline.
An important condition: it must have a different mechanism of action, different from penicillin drugs.
Why is this necessary?
We have already said that bacteria are able to “hide” from drugs by turning into L-forms.
These forms lack a cell wall completely or partially.
Penicillins act by affecting the cell wall.
If it is not present, the bacterium is immune to this drug.
It would seem, why then use penicillin at all?
Because only some pale spirochetes change into the L-form.
Most of them are in their usual spiral state.
They die under the influence of penicillin.
While another antibiotic, which inhibits protein synthesis, “finishes off” the remaining L-forms so that they do not cause a relapse in the future.
3. Use of short- or medium-acting drugs.
It is always better for the patient if he:
- visits the doctor less often;
- gives injections less often;
- spends less time on treatment.
Therefore, convenient forms of penicillin have been developed that accumulate in the body and are then gradually released.
They act on the causative agent of syphilis with a gradually weakening effect over 2 weeks or more.
Injections of such drugs are given once a week, which is very convenient for the patient.
But such drugs are less effective.
Therefore, they can only be used in the initial stages of syphilis.
The order of the Ministry of Health provides for the possibility of using durable penicillins not only in the primary, but also in the secondary period.
But many doctors don't want to take risks.
From the secondary period, they refuse such drugs, giving preference to penicillins, used once or several times a day.
This therapy is less well tolerated by the patient and requires hospitalization or frequent visits to the clinic.
But the likelihood of successful treatment is higher, and the risk of relapse is lower.
4. Insufficient control of cure.
You cannot treat a patient and send him home.
He is always being watched.
And for quite a long time - at least 3 months, if treatment is prescribed literally immediately after infection or the appearance of the first symptoms.
The observation period can reach 3 years or more if there were severe forms of syphilis.
Some patients receive additional treatment during this time.
If there is no proper control, then relapses occur very often.
Features of the causative agent of syphilis
The causative agent of syphilis is Treponema pallida, one of three types of spirochetes that are pathogenic to humans, namely the white spirochete (Spirochaeta pallida, also called pale). The other two treponemes cause similar diseases and are common on the American continents.
The pale spirochete is a thin thread with small, uniform bends, 6-14 microns long and 0.25 microns thick. Aniline dyes gave the spirochete a specific color, hence the name “pale”. The syphilis spirochete can be killed by disinfectants and drying. At a temperature of 45-48°C it dies within an hour, a temperature of 55°C kills the spirochete in 15 minutes. Low temperatures do not have a similar effect on the syphilis spirochete. At a temperature of 10°C it remains viable for several days.
The type of white spirochete includes, in addition to the typical pale treponema, also atypical forms that are able to tolerate influences that are unfavorable for its life (medicines, antibodies, radiation, temperature effects). In such conditions, atypical forms of spirochetes are the main way of spreading and maintaining syphilis infection.