- Gallery
- Reviews
- Articles
- Licenses
- Vacancies
- Insurance partners
- Partners
- Controlling organizations
- Schedule for receiving citizens for personal requests
- Online consultation with a doctor
- Documentation
Gastritis is inflammation of the gastric mucosa. It can be acute or chronic.
Heredity predisposes to the development of gastritis, especially if there is gastroduodenitis or peptic ulcer in the family. Symptoms of acute gastritis usually appear 6-12 hours after exposure to the causative factor.
Acute gastritis in children begins with:
- the appearance of general malaise;
- loss of appetite;
- feelings of nausea;
- feeling of heaviness in the stomach;
- Chills often appear, then the temperature rises to 37-38 °C.
Subsequently there are:
- repeated vomiting;
- pain in the upper abdomen;
- belching of air, often with an unpleasant smell of rotten eggs or a sharply sour taste.
The vomit contains the remains of food eaten 4-6 hours ago. An objective study reveals:
- pale skin;
- coating of the tongue with a white-yellow coating;
- bloating;
- pain in the epigastric region;
- moderate increase in heart rate;
- short-term diarrhea often appears, indicating involvement of the intestines in the pathological process.
The duration of the disease is 2-5 days. Acute gastritis due to food poisoning , in addition to the indicated symptoms, is accompanied by intoxication: longer vomiting, dehydration, temperature up to 39 degrees, longer duration of the disease - up to 7-10 days.
Gastritis, which appears against the background of common infectious and somatic diseases , is rarely identified as an independent disease and is regarded as secondary. It aggravates the course of the underlying disease and delays the child’s recovery.
About the disease
Gastritis is one of the most common diseases of the gastrointestinal tract (GIT), which occurs more often in children, starting from school age.
The disease is characterized by the formation of a focus of inflammation in the gastric mucosa. This is how characteristic clinical symptoms appear, which can be provoked by both external and internal causes. The pathology can be acute or chronic. The danger of the disease lies in the disruption of digestive function and the possible development of serious complications that worsen the patient’s quality of life. If left untreated, gastritis progresses from childhood into adulthood.
How to treat the disease
Since there are many types of gastritis, and each of them has its own causes, you cannot limit yourself to one treatment method. To combat each provoking factor, appropriate drugs are needed.
The doctor must determine by characteristic signs whether the patient’s acidity is increased or decreased. Depending on this, a suitable treatment regimen is selected.
Treatment of gastritis is usually complex, it is carried out in the following areas:
If the bacterium Helicobacter pylori is detected, it is important to eradicate it (complete destruction) with antibiotics. This is necessary to eliminate ulcerations, accelerate their healing and prevent the development of peptic ulcers and stomach cancer.
Symptoms of gastritis
The pathogenetic basis of gastritis is inflammation of the gastric mucosa. Because of this, local edema develops with impaired function. The secretion of enzymes decreases and digestion worsens. In parallel, a number of characteristic clinical signs arise:
- pain in the abdomen (“in the pit of the stomach”). They intensify when the child is hungry, because... there is additional secretion of gastric juice, which irritates the mucous membrane;
- loss of appetite;
- irritability;
- the formation of a white coating on the tongue;
- belching sour or rotten with bad breath;
- nausea, vomiting - these symptoms are characteristic of a severe course of the disease.
Due to disruption of the normal digestion process and loss of appetite, the child begins to eat less. There is a lack of vitamins and minerals, which is accompanied by secondary symptoms - pale skin, deterioration in the quality of hair and nails. With prolonged absence of adequate nutrition, the child begins to lose weight, anemia develops, blood pressure decreases, and the heart rate (HR) increases. In the case of a bacterial infection (phlegmonous gastritis), high fever appears (up to 39-40°C) with a marked deterioration in the condition of the small patient. Such patients require immediate hospitalization.
Chronic gastritis
According to the causes of chronic gastritis, there are:
- Primary (exogenous). As an independent disease.
- Secondary (endogenous). As one of the manifestations of other somatic pathologies.
By localization:
- Focal (fundal). When it affects the bottom of the stomach;
- Common. Affects several sections, most or all of the stomach (pangastritis);
- Combined (gastroduodenitis). It causes inflammation of the stomach and duodenum.
With the flow:
- Latent (hidden, asymptomatic);
- Monotonous (symptoms are always present);
- Recurrent (alternate periods of exacerbations and remissions).
By stages (phases) of the process:
- Exacerbation (severe symptoms);
- Incomplete clinical remission (unexpressed symptoms, inflammation of the stomach is visible during FGDS);
- Clinical remission (there are no symptoms, but during FGDS inflammation of the mucous membrane is detected);
- Clinical and endoscopic remission (no symptoms, no traces of inflammation during instrumental examination).
According to changes in the mucous membrane:
- Superficial (without atrophy);
- Hypertrophic (with the growth of the mucous membrane, the formation of cysts and polyps);
- Hemorrhagic (tendency to bleeding from the walls of the stomach);
- Erosive (with the formation of stomach ulcers);
- Subatrophic (slow small-focal atrophy);
- Atrophic;
- Mixed.
Causes of gastritis
The most common cause of gastritis is dietary errors.
Eating too spicy, fatty, hot, rough food leads to mechanical and chemical irritation of the child’s gastric mucosa, which is accompanied by the appearance of typical signs of the disease. It is worth noting that if such a diet violation is episodic in nature, the disease may not have time to develop. In addition to the nutritional (food) aspect, pathogenic microorganisms play an important role in the etiology of gastritis. Most often, the cause of the disease is bacteria that enter the child’s stomach with poor-quality food (food poisoning). A similar effect occurs when using aggressive medications, alcohol or drugs.
An important endogenous cause of gastritis in children is the bacterium Helicobacter Pylori. The pathogen normally lives in the pyloric part of the stomach, and if there are appropriate conditions for its reproduction, it affects the entire surface of the mucous membrane of the organ. The bacterium secretes aggressive toxins that irritate the inner layer of the stomach and provoke inadequate secretion of hydrochloric acid. The result of this phenomenon is the development of gastritis.
Additional provoking factors are considered:
- hereditary predisposition;
- irregular food intake;
- eating large amounts of fast food, snacks (chips, crackers), carbonated drinks;
- chronic diseases of other gastrointestinal organs in the acute stage (cholecystitis, pancreatitis);
- seasonal weakening of immune defense;
- uncontrolled use of medications (antipyretics, antibiotics, hormonal agents).
Treatment
The treatment plan for gastritis in children depends on the form of the disease and its severity.
Therapy for acute gastritis includes:
- Bed rest for 2-3 days;
- Gastric lavage;
- Hunger in the first 8-12 hours after the onset of symptoms, then switching to liquid food (puree soups, low-fat broths, crackers without spices and salt, jelly and porridge), on days 5-7 the child is transferred to normal food;
- Drink plenty of fluids (preferably special solutions for rehydration);
- In case of severe dehydration, saline solution with 5% glucose solution is administered intravenously;
- Laxative for constipation;
- Antiemetics for vomiting;
- Antibiotics for infection;
- Additionally: B vitamins, enzymes for the gastrointestinal tract.
For chronic gastritis, the following is additionally prescribed:
- Eradication therapy (a special treatment regimen for the destruction of Helicobacter pylori (omeprazole + amoxicillin + imidazole/metranidazole/clarithromycin). Duration - 10 days. If ineffective, the regimen is changed.
- M-cholinergic receptor blocker to relax the smooth muscles of internal organs and suppress the secretion of the digestive glands.
- Antacids, histamine H2 receptor blockers to reduce gastric secretion.
Treatment is carried out until remission occurs, the duration of which is variable: from several months to several years.
Diagnosis of gastritis
“SM-Doctor” is a medical center whose gastroenterologists have many years of successful experience in the early detection and treatment of gastritis of any etiology in children aged 0 to 18 years. Our own laboratory and modern diagnostic equipment guarantees the identification of the root cause of inflammation in the stomach in the shortest possible time. The gastroenterologist begins the diagnosis of gastritis by collecting a history of the disease and analyzing the patient’s complaints. After this, the specialist palpates the abdomen and conducts a full physical examination. To confirm the final diagnosis, the doctor prescribes the following auxiliary tests and procedures:
- fibroesophagogastroduodenoscopy (FEGD) is an endoscopic technique that allows you to visually assess the condition of the gastric mucosa and identify the area of damage;
- pH-metry is a technique for assessing the acidity of the stomach contents;
- general clinical tests (blood, urine).
To identify the presence of H. Pylori, the doctor may prescribe a urease breath test or a specialized serological blood test (determines the concentration of antibodies to the corresponding pathogen). Positive results of these tests influence the choice of treatment for the patient.
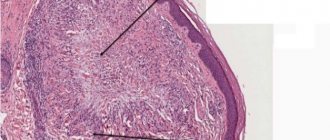
Types of damage to the mucous membrane
Gastritis can also be classified according to the degree of change in the gastric mucosa. The mildest form is superficial, when the inflammatory process affects only the upper part of the mucosa. More dangerous forms include the following:
Although hyperplastic gastritis is characterized by the appearance of neoplasms, they are predominantly benign.
The atrophic form often leads to stomach cancer. Each of these types can be focal or diffuse: the first covers a small area of the mucous membrane (although there may be several of them), the second spreads over its entire surface.
Treatment of gastritis
Gastritis is a gastrointestinal disease, the key aspect of treatment of which remains diet.
The child should eat often, but in fractional portions. Fried, fatty foods, smoked foods, spicy seasonings, and marinades are temporarily excluded. All food must be boiled or steamed. It is recommended to feed the child pureed foods to minimize mechanical irritation of the gastric mucosa. Medication correction of the baby’s well-being is achieved using the following groups of drugs:
- proton pump inhibitors (Pantoprazole, Omeprazole), which reduce acidity;
- enveloping drugs - Almagel, Gaviscon;
- antibiotics (Metronidazole, Clarithromycin) are used to identify H. Pylori or other pathogenic bacteria.
In case of serious complications (bleeding, perforation, etc.), surgical intervention may be required.
Prevention of gastritis of any etiology involves eating well-heat-treated food in fractional portions. It is recommended not to abuse fast food. But the main thing is regular, nutritious meals. Gastritis is often also called “students’ disease” due to constant dry snacks. “SM-Doctor” is an advanced medical center that provides a full package of diagnostic and therapeutic services to patients with various forms of gastritis. The sooner the child begins to receive adequate treatment, the faster he will recover.
Consequences of gastritis
The health prognosis for this disease is positive with adequate treatment. The child is subject to dispensary observation until 3 years of age. A pediatrician and a gastroenterologist consult the child 2 times a year. Sanatorium-resort treatment in gastroenterological sanatoriums is welcome. In most cases, it is possible to relieve inflammation and restore the structure of the mucosa. However, in some patients the process is not completely cured and relapses of the disease are observed. For every exacerbation, you should contact a pediatrician or pediatric gastroenterologist.
The following complications of gastritis are distinguished:
- Stomach ulcer . A mucosal defect is formed, which can progress over time and cause perforation or penetration of the stomach wall.
- Gastric bleeding is caused by damage to the vascular network. This is due to ulcers, erosions and areas of necrosis in the mucous membrane.
- Anemia . Atrophy of the mucosa leads to a deficiency of vitamin B12, which is necessary for normal hematopoiesis.
- Tumor . A stomach ulcer can malignize and develop into a malignant tumor. This occurs when cells lose their normal structure.
The consequences of gastritis and their severity directly depend on the timeliness of seeking medical help. Therefore, if you notice the first symptoms of the disease, immediately make an appointment with a doctor. At the Into-Sana clinic, your child is examined by qualified specialists with many years of experience.
Diet features
Proper nutrition is the key to minimizing relapses of gastritis.
- Regular fractional meals in equal portions.
- Only high-quality food, freshly prepared.
- Lack of fatty, spicy, smoked, fried foods containing a lot of spices and additives, raw vegetables, buns, legumes.
- Eating steamed or boiled foods.
- The presence in the menu of cereals, mashed potatoes, chicken, lean meat and fish, weak tea, cocoa with milk, honey, crackers, etc. on the recommendation of a doctor.
Diagnostics
The question of how to treat gastritis is relevant for many people faced with this problem. First of all, it is necessary to undergo a comprehensive diagnosis. Its purpose is to determine the specifics of the disease in a particular case. As part of the diagnosis, the doctor interviews the patient and examines him. During the dialogue, the doctor asks the patient what he ate before symptoms appeared, what medications he uses, and whether he has any concomitant diseases. Among the signs indicating the presence of acute gastritis in a patient are problems with the skin, plaque on the tongue, rashes between the nose and lips, and an unpleasant odor from the mouth. When palpating the abdomen, pain occurs.
To confirm or refute the diagnosis, the gastroenterologist must conduct a comprehensive study, the results of which allow one to obtain an accurate answer to the question of what the patient is sick with.
Is it possible to cure gastritis in a child?
Compliance with all doctor’s recommendations and a carefully thought-out nutrition plan for the child gives a good prognosis for the treatment of gastritis. It is especially important to adhere to a therapeutic diet during an exacerbation of the disease.
Signs of exacerbation of gastritis:
- decreased appetite;
- pain and feeling of heaviness after eating;
- belching, etc.
On the first day of exacerbation of the disorder, it is recommended to refrain from eating, and then carefully introduce puree soups, kefir or low-fat broth into the diet. And it is imperative to exclude carbonated drinks, chocolate, dairy products and fruits.
For chronic gastritis, 4 meals a day are recommended, but it is not allowed to give the child fatty meats and foods containing coarse fiber.
Careful monitoring of the response to treatment, as well as regular examination by a pediatric gastroenterologist, allows you to get rid of the disease as quickly as possible and minimize the likelihood of developing complications and relapses of gastritis in children.
2
0
2
Article rating:
4 out of 5 based on 4 ratings
Author: Omelchenko Elena Vladimirovna
Pediatric gastroenterologist. Highest qualification category. Work experience 29 years.
Advantages of SM-Clinic
In our medical center you will find some of the best gastroenterologists in the city for the diagnosis and treatment of childhood gastritis of all forms. We will quickly diagnose a child of any age, prescribe effective therapy, and provide the necessary consultations on nutrition and relapse prevention.
You can make an appointment by phone.
Sources:
- E. V. Savitskaya. Features of gastroduodenal pathology in children of preschool and primary school age // Suchasna gastroenterology, 2008, No. 3, p. 35-37.
- Yu.V. Belousov. Chronic atrophic gastritis in children // Clinical Pediatrics, 2011, 5 (32).
- L. N. Tsvetkova [and others]. Gastroenterological pathology in children: pathomorphosis of diseases and improvement of diagnostic methods at the present stage // Materials of the XVIII Congress of Children's Gastroenterologists, 2011, p. 5-8.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
How to relieve pain with gastritis in a child?
The nature and degree of pain in different types of gastritis is different, but all pain impulses come from the muscular layer of the stomach, since there are no pain receptors in the mucous membrane. The origin and source of pain signals determines the scheme for their elimination.
Thus, pain in acute gastritis has a cramping nature (spastic pain), so it is relieved by taking antispasmodics, enterosorbents and mandatory diet.
Pain in acute gastritis caused by intoxication is recommended to be relieved by gastric lavage, as well as by taking an enterosorbent and an antiemetic drug if necessary.
Reducing pain during exacerbation of the chronic form of the disease is achieved by taking analgesics, antispasmodics, enzymes and anticholinergics. However, since these medications can negatively affect the functioning of the gastrointestinal tract, while taking them you need to follow a gentle diet and take gastroprotectors.
Thus, the main types of medications that reduce pain in gastritis are:
- analgesics that lower the tone of the muscle fibers of the stomach and reduce their spasm, blocking the transmission of pain impulses from the stomach to the brain;
- gastroprotectors or astringents, they have a bactericidal effect and form a protective film on the gastric mucosa. These drugs not only prevent irritation, but also relieve inflammation of the mucous layer;
- enzymes that help break down food and improve digestion;
- antacids that neutralize the aggressive effects of hydrochloric acid during its excessive synthesis;
- anticholinergics, which have an antispasmodic effect, reduce the secretion of gastric juice and do not affect the formation of a protective layer of mucus.
The composition of the course of therapy is prescribed exclusively by a gastroenterologist, since the type of medications and their dose depend on the type of disease, its prevalence and the degree of inflammation of the mucous membrane.
Classification
Gastritis is a common problem among patients of different ages, and it can be expressed in different forms. At the present stage, doctors classify acute gastritis according to the following criteria:
- According to the depth of inflammation:
- Superficial (partial damage to the mucous membrane);
- Deep (complete damage to the mucous membrane).
- By prevalence:
- Local (affects a specific area);
- Diffuse (spreads over the entire area).
- According to etiology:
- Infectious (penetration of bacteria into the body);
- Non-infectious (manifestation of allergic reactions, entry of chemicals into the body, reduced immunity).
4. According to the nature of the inflammatory process:
- Catarrhal - accompanied by the appearance of redness and swelling of the mucous membrane. In most cases, it is caused by the abuse of junk food;
- Fibrinous - can be caused by infection or poisoning with chemicals, in practice it is rare; when present, a gray or yellow-brown film appears on the walls of the stomach;
- Hemorrhagic (corrosive) - this type is usually classified as a severe form of the disease. Violation of the integrity of the gastric mucosa is the result of exposure to chemicals entering the body;
- Phlegmonous - in this case, destruction of the mucosal wall is observed under the influence of pus, as a result it penetrates into the submucosal tissue. It appears against the background of injuries, infections, complications of oncology or stomach ulcers.