Causes
The following factors contribute to the occurrence of gardnerellosis:
- Taking antibiotics, including vaginal medications (suppositories, etc.);
- The presence of an intrauterine device;
- Infectious diseases;
- Poor environmental situation;
- Frequent change of sexual partners;
- Unbalanced diet, limited consumption of fermented milk products;
- Wearing synthetic, tight underwear;
- Constant douching;
- Using intimate cosmetics, tampons, etc.
Bacterial vaginosis can also appear against the background of pathologies of internal organs:
- Disruptions in the functioning of the endocrine system, including during pregnancy;
- Stress;
- Disturbances in the bacterial balance of the intestinal microflora and genitourinary system;
- Increased physical and emotional stress;
- Decreased immunity.
How gardnerellosis manifests itself in men
Symptoms in men depend on the location of Gardnerella activity. In most cases, the bacterium lingers in the lower part of the urinary tract - the urethra. Symptoms of gardnerellosis are:
- itching, burning, swelling and redness in the area of the external urethral opening;
- difficulty urinating;
- pain during micturition;
- burning after going to the toilet;
- grayish discharge from the urethra;
- unpleasant odor emanating from the genitals.
Gardnerellosis increases the likelihood of concomitant infections. In the case of balanoposthitis, swelling, redness, burning, and the formation of ulcers in the area of the head and foreskin are possible. Inflammation of the bladder (cystitis) is manifested by an increased urge to urinate, pain in the lower abdomen, and, somewhat less frequently, by an increase in body temperature. Inflammation of the seminal vesicles (vesiculitis) can manifest itself brightly (fever, weakness and pain in the suprapubic region) or blurred (periodic moderate pain, impaired potency, etc.). Prostatitis is characterized by pressing pain in the groin, decreased libido, problems with erection and orgasm, as well as difficulty urinating and the urge to go to the toilet at night.
If you have any questions, call us at: +7 Medical administrators are always ready to advise you.
Symptoms
If the disease develops, the following appears:
- Burning and itching;
- Copious discharge with a fishy odor;
- Unpleasant sensations during urination and sexual intercourse;
- Swelling of the external genitalia.
With bacterial vaginosis, inflammation affects the vagina, urethra and cervix.
Why is bacterial vaginosis dangerous?
With concomitant gardnerellosis after childbirth and in the presence of intrauterine contraceptives, complications may appear: endometritis, adnexitis, etc. This disease negatively affects pregnancy, which in most cases ends in premature birth.
Diagnostics
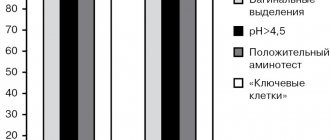
The diagnosis of bacterial vaginosis is established on the basis of clinical and special laboratory research methods. The “gold diagnostic standard” proposed by R. Amsel are:
- Vaginal discharge of homogeneous consistency, gray-white color with an unpleasant odor.
- Vaginal discharge has a pH greater than 4.5.
- Presence of a positive amine test.
- The presence of “key” cells (covered with gram-variable flora) in smears of vaginal discharge.
The diagnosis is established even if 3 of the 4 criteria described above are present.
The pH-metry test is low specific, but highly sensitive (80 - 98%).
The amine test is highly specific (87 - 97%), its sensitivity is in the range of 34 - 79%. The essence of the amine test is to increase or appear a “fishy” odor when mixing equal proportions of vaginal secretion and potassium hydroxide. A specific odor indicates the presence of volatile amines: cadaverine, tyramine, phenethylamine, histamine, putrescine and isobutylamine, which are metabolic products of strict anaerobic bacteria.
In 70 - 90% of cases, bacterioscopy of vaginal discharge reveals “key” cells (vaginal epithelial cells covered with gram-variable rods and/or coccobacilli). High sensitivity and specificity of the technique is achieved by Gram staining of smears.
Characteristic signs of the disease are:
- The presence of a large number of vaginal epithelial cells in smears.
- The presence of a large number of “key” cells in smears.
- Complete absence or sharp decrease in lactobacilli.
- The presence in smears of a large number of gram-negative and/or gram-variable bacilli and/or coccobacilli (Gardnerella vaginalis, Fusobacterium spp, Bacteroides spp.), as well as virion-like gram-variable bacilli (Mobiluncus spp).
- Rare presence or complete absence of polynuclear leukocytes.
General microbial contamination is assessed using a 4-point system:
- “+” – minimum (up to 10) number of microbial cells in one field of view.
- “++”—moderate (from 11 to 100) number of microbial cells in one field of view.
- “+++” - a large (from 100 to 1000) number of microbial cells in one field of view.
- “++++” is a massive (more than 1000) number of microbial cells in one field of view.
The correctness of the preliminary diagnosis is confirmed by bacteriological examination, which is the most reliable step in the diagnosis of bacterial vaginosis. This technique is also used to monitor the effectiveness of antimicrobial therapy. Due to its non-specificity for bacterial vaginosis, culture testing for Gardnerella vaginalis is not recommended.
Rice. 6 and 7. Smear microscopy. Gram stain. “Key” cells (mature cells of the vaginal epithelium, covered with gram-variable bacteria).
Rice. 8 and 9. Smear microscopy. Gram stain. “Key” cells, on the surface of which there is a huge number of Gardnerella bacteria.
Treatment
Treatment of this pathology is carried out in stages:
- Stage I – reducing the level of pathogenic microorganisms. Antibacterial therapy is used for these purposes;
- Stage II – restoration of the vaginal microflora. In this case, probiotics, suppositories with lactobacilli, and immunomodulators are used.
A control smear is prescribed after one and a half to two months. Until then, it is recommended to use condoms during sexual intercourse.
Possible treatments:
- The “Gineton” device is a low-frequency ultrasound, the effect of which is the basis of this hardware technique, which eliminates the source of infection and improves the penetration of drugs into tissues.
Treatment of pregnant women
Therapeutic therapy during pregnancy differs from the standard regimen in that:
- Antibiotics are not prescribed;
- Treatment is carried out after the first trimester.
Treatment of bacterial vaginosis
Treating bacterial vaginosis is not an easy task. There are currently no optimal treatment regimens. Late diagnosis and low effectiveness of antimicrobial drugs lead to frequent relapses. Patients may not receive appropriate medical care for years.
The goal of treatment is to delay the growth of microorganisms that are not typical for this microcenosis and restore the normal microflora of the vagina.
To eliminate obligate anaerobic microflora, antimicrobial drugs of different mechanisms of action are used. Metronidazole and Clindamycin are the drugs of choice for the treatment of bacterial vaginosis. The effectiveness of these drugs reaches 85 - 95%.
Metronidazole
Metronidazole (Trichopol, Metrogyl) is one of the drugs of choice in the treatment of bacterial vaginosis. 5-nitroimidazole derivatives are active against protozoa and anaerobic bacteria. They are used both orally and intravaginally. The most effective is combination treatment, when the drug is used simultaneously orally and intravaginally:
- Metronidazole, Metrogyl and Trichopolum are used orally. Side effects from the digestive tract, nervous system and frequent allergic manifestations limit the intake of medications.
- The vaginal route of administration is more preferred. Trichopolum is used intravaginally in the form of tablets 1 time per day, 500 mg for 7 - 10 days. Before insertion into the vagina, the tablet is moistened in cold boiled water. Metrogyl gel is applied 2 times a day, 1 applicator for 5 days in a row.
Other drugs of the nitroimidazole group
In the treatment of bacterial vaginosis, other drugs of the nitroimidazole group are also used: Tinidazole, Ornidazole. Drugs in this group are contraindicated during pregnancy.
Clindamycin
Clindamycin (Dalacin) is one of the drugs of choice for the treatment of bacterial vaginosis. Its effectiveness reaches 91%. It is used orally and intravaginally in the form of ovules and cream. Allergies and increased growth of yeast-like fungi are the main side effects of the drug.
Prevention of the development of vaginal vaginosis
In order to prevent the development of vaginal candidiasis, treatment is supplemented with antimiotics. Convenient to use are such drugs as intravaginal tablets Terzhinan (ternidazole + neomycin sulfate + nystatin + prednisolone), Klion-D suppositories (metronidazole + miconazole), Metrogyl Plus gel (metronidazole + clotrimazole), Metromicon-Neo suppositories (metronidazole + miconazole) .
Drugs such as Fluconazole, Diflucan, Mikosist, etc. are used internally to prevent candidiasis.
Restoration of vaginal microcenosis
Eubiotics such as Atsilak, Lactobacterin, Bifidumbacterin stimulate the growth of vaginal lactoflora. The drugs are used in the form of suppositories once a day at night for 10 days. Before using eubiotics, control microbiological confirmation of the absence of fungi is mandatory.
Rice. 10 and 11. Metronidazole and Clindamycin are the drugs of choice for the treatment of bacterial vaginitis.
Complications
Bacterial vaginosis, as a rule, does not cause complications. But under certain circumstances, bacterial vaginosis can cause:
- Premature birth. In pregnant women, bacterial vaginosis is associated with premature birth and low birth weight babies.
- Sexually transmitted infections. Bacterial vaginosis makes women more susceptible to sexually transmitted infections such as HIV, herpes simplex virus, chlamydia or gonorrhea. If you have HIV infection, bacterial vaginosis makes it more likely that a woman will be able to infect her partner more easily.
- Risk of infectious complications after gynecological operations. Bacterial vaginosis can cause postoperative complications (eg hysterectomy).
- Inflammatory diseases of the pelvic organs. Bacterial vaginosis can cause inflammation of the pelvic organs, for example, prevention of HIV, uterus and fallopian tubes, which leads to an increased risk of infertility.
When to see a doctor
The following reasons may be reasons for contacting a gynecologist:
- You have never had an infectious disease. Your doctor will help you understand the causes and identify the symptoms.
- You have had similar diseases before, but the symptoms that arose this time are different from before.
- You have had several sexual partners or recently found a new one. Possibly a sexually transmitted disease. The signs and symptoms of some sexually transmitted infections are similar to vaginal bacteriosis.
- You tried to treat yourself and took medications, but recovery did not occur. There is a high temperature or an unpleasant vaginal odor from the vagina.