Pharmacological properties of the drug Cyproterone
Cyproterone refers to synthetic antiandrogens - antagonists of male sex hormones. It is an antiandrogenic agent with a steroid structure. Cyproterone acetate, through competitive binding, blocks tissue receptors of male sex hormones - androgens (testosterone, dihydroepiandrosterone, androstenedione, etc.). Designed to eliminate the phenomena of androgenization in women, correction of deviations in the sexual sphere in men, antiandrogen therapy for prostate carcinoma. Androgens are also produced in small quantities in the body of women, mainly in the adrenal glands, ovaries and skin. Androgen-dependent derivatives of the skin (sebaceous glands and hair follicles) with an increase in the level of androgen production increase sebum secretion, which is a pathogenetic factor in the development of seborrhea and acne (acne), there is excess hair growth in women according to the male type (hirsutism) with simultaneous hair loss on the head (androgenic alopecia). Cyproterone reduces these signs of androgenization in women, which is clinically manifested by healing or preventing the formation of acne, reducing excessive sebum secretion on the scalp and facial skin. Cyproterone also has gestagenic properties - it inhibits the secretion of gonadotropic hormones in the pituitary gland and inhibits ovulation, which determines its contraceptive effect. In men, excessive formation of androgens causes increased testicular function, increased potency and libido, and in such androgen-dependent diseases as prostate carcinoma, it contributes to the progression of the disease. The administration of the drug reduces excessive sexual desire, protects the prostate gland (the target organ for androgens) from the effects of androgens, and inhibits the growth of prostate tumors. Used in the form of tablets and prolonged depot form for intramuscular administration.
Subtleties of application
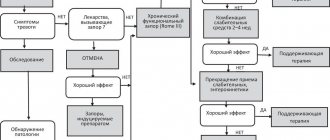
Estrogen in COCs helps eliminate LDL and increase HDL and triglyceride levels. Progestins counteract estrogen-induced changes in lipid levels in the body.
- For acne, medications containing cyproterone acetate, drospirenone or desogestrel are prescribed as a progestin. COCs containing cyproterone acetate and ethinyl estradiol are more effective for acne than the combination of ethinyl estradiol and levonorgestrel [4].
- For hirsutism, medications containing progestogens with antiadrogenic properties are recommended: cyproterone acetate or drospirenone [5].
- Combinations of estradiol valerate and dienogest are more effective in reducing menstrual blood loss than ethinyl estradiol and levonorgestrel [6]. In addition, the intrauterine system is indicated for the treatment of menorrhagia.
- Preparations containing drospirenone 3 mg and ethinyl estradiol 20 mcg are recognized as the most effective combination for correcting PMS symptoms, including those of a psychogenic nature [7].
- Taking oral contraceptives increases systolic blood pressure (BP) by 8 mmHg. Art., and diastolic - by 6 mm Hg. Art. [8]. There is evidence of an increased risk of cardiovascular events in women taking COCs [9]. Due to the increased likelihood of developing myocardial infarction and stroke in patients with arterial hypertension, when prescribing COCs, the benefit/risk ratio must be carefully weighed.
- In non-smoking women under 35 years of age with compensated hypertension, COCs can be prescribed with careful monitoring of blood pressure during the first months of use.
- In cases of increased blood pressure while taking COCs or in women with severe hypertension, an intrauterine system or DMPA is indicated [10].
- The selection of a contraceptive for patients with dyslipidemia must be carried out taking into account the effect of the drugs on lipid levels (see Table 5).
- Because the absolute risk of cardiovascular events in women with controlled dyslipidemia is low, COCs containing 35 mcg or less of estrogen can be used in most cases. For patients with LDL levels above 4.14 mmol/l, alternative means of contraception are indicated [8].
- The use of COCs in women with diabetes mellitus accompanied by vascular complications is not recommended [2]. A suitable option for hormonal contraception for diabetes mellitus is the intrauterine levonorgestrel-releasing system, and, as a rule, no dose adjustment of hypoglycemic drugs is required.
- The results of epidemiological studies examining the risk of myocardial infarction when oral contraceptives are prescribed to women who smoke are contradictory. Due to limited convincing data, COCs are recommended to be prescribed with caution to all women over 35 years of age who smoke.
- Obesity with a body mass index of 30 kg/m2 and above reduces the effectiveness of COCs and transdermal GCs [8]. In addition, the use of COCs in obesity is a risk factor for venous thromboembolism. Therefore, the method of choice for such patients is mini-pills (gestagen-containing tablet contraceptives) and intrauterine contraceptives (levonorgesterel-releasing system).
- Use of COCs with estrogen dosages of less than 50 mcg in nonsmoking, healthy women over 35 years of age may have beneficial effects on bone density and vasomotor symptoms during perimenopause [8]. This benefit must be considered in light of the risk of venous thromboembolism and cardiovascular factors. Therefore, women of the late reproductive period are prescribed COCs individually.
List of sources
- Van Vliet HAAM et al. Biphasic versus triphasic oral contraceptives for contraception //The Cochrane Library. — 2006.
- Omnia M Samra-Latif. Contraception. Available from https://emedicine.medscape.com
- Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53,297 women with breast cancer and 100,239 women without breast cancer from 54 epidemiological studies. Lancet 1996; 347(9017):1713–1727.
- Carlborg L. Cyproterone acetate versus levonorgestrel combined with ethinyl estradiol in the treatment of acne. Results of a multicenter study. Acta Obstetricia et Gynecologica Scandinavica 1986;65:29–32.
- Batukan C et al. Comparison of two oral contraceptives containing either drospirenone or cyproterone acetate in the treatment of hirsutism. Gynecol Endocrinol 2007;23:38–44.
- Fruzzetti F, Tremollieres F, Bitzer J. An overview of the development of combined oral contraceptives containing estradiol: focus on estradiol valerate/dienogest. Gynecol Endocrinol 2012;28:400–8.
- Lopez LM, Kaptein AA, Helmerhorst FM. Oral contraceptives containing drospirenone for premenstrual syndrome. Cochrane Database Syst Rev 2012.
- Armstrong C, Coughlin L. ACOG releases guidelines on hormonal contraceptives in women with coexisting medical conditions. — 2007.
- Carr BR, Ory H. Estrogen and progestin components of oral contraceptives: relationship to vascular disease. Contraception 1997; 55:267–272.
- Burrows LJ, Basha M, Goldstein AT. The effects of hormonal contraceptives on female sexuality: a review. The journal of sexual medicine 2012; 9:2213–23.
Indications for use of the drug Cyproterone
Moderately pronounced phenomena of androgenization in women (hirsutism, severe or moderate forms of androgenetic alopecia and acne) with resistance to other types of therapy. Prescribed for severe androgenization phenomena. Men are prescribed antiandrogen therapy for inoperable prostate carcinoma, either without or after prior orchiectomy; in the treatment of prostate carcinoma with RF LH agonists; for the correction of painful or pathological abnormalities in the field of sexual desire, necessitating a reduction in sexual activity.
Use of the drug Cyproterone
Women with moderate androgenization phenomena are prescribed 10 mg/day orally, usually in combination with a gestagen-estrogen drug to simultaneously prevent pregnancy and prevent the development of intermenstrual bleeding. Both medications are taken from the 1st day of the menstrual cycle, cyproterone is taken 10 mg/day from the 1st to the 15th day of the menstrual cycle. The gestagen-estrogen drug is taken daily from the 1st to the 21st day of the cycle, 1 tablet per day. Then they take a 7-day break, during which menstrual-like bleeding occurs. If there is no bleeding, medication can be continued only after pregnancy has been ruled out. After the break, treatment is continued in the above manner. For amenorrhea, taking cyproterone begins on any day and the 1st day of taking the drug is conventionally taken as the 1st day of the menstrual cycle. The duration of treatment is usually several months. Acne and seborrhea are treatable faster than hirsutism and alopecia. After clinical improvement, stop taking cyproterone and continue to take only the gestagen-estrogen drug. In cases of severe androgenization in women, cyproterone is used from the 1st to the 10th day of the menstrual cycle, 100 mg once a day, in combination with taking a gestagen-estrogen drug from the 1st to the 21st day of the cycle. The treatment regimen is similar to that above. After clinical improvement, the dose of cyproterone can be reduced to 25–50 mg/day. In women after menopause or with a removed uterus, only cyproterone monotherapy is administered at a dose of 25–50 mg/day according to the following scheme: 21 days on, 7 days off. For inoperable prostate carcinoma (to exclude the influence of androgens of the adrenal cortex after orchiectomy), cyproterone is prescribed 100 mg 1-2 times a day or administered intramuscularly as a depot injection 300 mg once every 2 weeks. If orchiectomy has not been performed, cyproterone is prescribed 100 mg 2-3 times a day or administered intramuscularly once a week. If the condition improves or the disease remits, cyproterone is continued. The duration of therapy is determined individually and is about 6 months. When treating patients with inoperable prostate carcinoma with RF LH agonists, only cyproterone is first prescribed for 5–7 days, 100 mg 2 times a day, and in the next 3–4 weeks, an RF LH agonist is added. To limit the effect of adrenal cortex androgens during treatment with RF LH agonists, cyproterone continues to be taken at a dose of 100 mg 1–2 times a day. When treating pathological deviations of sexual desire, the dose of cyproterone is selected individually. Usually, at the beginning of the course, 50 mg is prescribed 2 times a day or injections of a depot form of 300 mg IM once every 10–14 days; if necessary, the oral dose is increased to 100 mg 2 times a day, and temporarily - up to 3 times a day or up to 600 mg of the depot form once every 10-14 days intramuscularly. In case of a satisfactory therapeutic effect, the single dose is reduced to the minimum maintenance dose. In most cases, 25 mg 2 times a day is enough for this. In this case, the dose reduction should be gradual over several weeks. To stabilize the therapeutic effect, cyproterone is usually used long-term, for several months.
Transdermal Therapeutic System (TTS)
The transdermal therapeutic system patch is applied for 7 days. The used patch is removed and immediately replaced with a new one on the same day of the week, on the 8th and 15th days of the menstrual cycle.
TTS appeared on the market in 2001 (“Evra”). Each patch contains a week's supply of norelgestromin and ethinyl estradiol. TTC is applied to dry, clean skin of the buttocks, abdomen, outer surface of the upper arm or torso with minimal hair growth. It is important to monitor the density of TTC attachment every day and not apply cosmetics nearby. Daily release of sex steroids (203 mcg norelgestromin + 33.9 mcg ethinyl estradiol) is comparable to that of low-dose COCs. On the 22nd day of the menstrual cycle, the TTS is removed and a new patch is applied 7 days later (on the 29th day).
The mechanism of action, effectiveness, disadvantages and advantages are the same as those of COCs.
Contraindications to the use of the drug Cyproterone
Pregnancy, severe liver dysfunction, hereditary benign hyperbilirubinemia (Rotor syndrome, Dubin-Johnson syndrome), liver tumors, a tendency to thrombus formation, severe diabetes mellitus with vascular complications, sickle cell anemia, a history of herpes, idiopathic jaundice or itching during pregnancy, severe chronic depression. For prostate carcinoma, the diseases listed above (with the exception of primary liver tumors and severe depression) are a relative contraindication and the issue of using cyproterone is decided individually. The use of cyproterone is not recommended for people under the age of 18 (before the completion of puberty).
Combined oral contraceptives (COCs)
Most drugs use the estrogen ethinyl estradiol at a dosage of 20 mcg. The following is used as a gestagen:
- norethindrone;
- levonorgestrel;
- norgestrel;
- norethindrone acetate;
- norgestimate;
- desogestrel;
- Drospirenone is the most modern progestin.
A new trend in the production of COCs is the release of drugs that increase the level of folate in the blood.
These COCs contain drospirenone, ethinyl estradiol and calcium levomefolate (a metabolite of folic acid) and are indicated for women planning a pregnancy in the near future. Monophasic COC contraceptives have a constant dose of estrogen and progestin. Biphasic COCs contain two, triphasic - three, and four-phase - four combinations of estrogen and progestogen. Multiphasic drugs have no advantages over monophasic combined oral contraceptives in terms of effectiveness and side effects [1].
About three dozen COCs are available on the pharmaceutical market, the vast majority of which are monophasic. They are available in the form of 21+7:21 hormonally active tablets and 7 placebo tablets. This facilitates consistent daily monitoring of regular COC use.
Combined oral contraceptives (COCs) list: types and names
Mechanism of action
The main principle of operation of COCs is to inhibit ovulation. The drugs reduce the synthesis of FSH and LH. The combination of estrogen and progestin gives a synergistic effect and increases their antigonadotropic and antiovulatory properties. In addition, COC contraceptives change the consistency of cervical mucus, cause endometrial hypoplasia and reduce contractility of the fallopian tubes.
Efficiency largely depends on compliance. The pregnancy rate during the year ranges from 0.1% with correct use to 5% with violations of the dosage regimen.
Advantages
Combined hormonal contraceptives are widely used to treat menstrual irregularities and reduce or eliminate ovulatory syndrome. Taking COCs reduces blood loss, so it is advisable to prescribe them for menorrhagia. COCs can be used to adjust the menstrual cycle - if necessary, delay the onset of the next menstruation.
COCs reduce the risk of developing benign breast formations, inflammatory diseases of the pelvic organs, and functional cysts. Taking COCs for existing functional cysts helps to significantly reduce them or completely resolve them. The use of COCs helps reduce the risk of malignant ovarian diseases by 40%, endometrial adenocarcinoma - by 50% [2]. The protective effect lasts up to 15 years after discontinuation of the drug.
Flaws
Side effects: nausea, breast tenderness, breakthrough bleeding, amenorrhea, headache.
Estrogen, which is part of COCs, can activate the blood clotting mechanism, which can lead to the development of thromboembolism. The risk group for developing such complications while taking COCs includes women with high levels of LDL and low levels of HDL in the blood, severe diabetes accompanied by arterial damage, uncontrolled arterial hypertension, and obesity. In addition, the likelihood of developing blood clotting disorders increases in women who smoke.
Contraindications for the use of combined oral contraceptives
- thrombosis, thromboembolism;
- angina pectoris, transient ischemic attacks;
- migraine;
- diabetes mellitus with vascular complications;
- pancreatitis with severe triglyceridemia;
- liver diseases;
- hormone-dependent malignant diseases;
- bleeding from the vagina of unknown etiology;
- lactation.
COCs and breast cancer
The most comprehensive analysis of cases of breast cancer development while taking COCs was presented in 1996 by the Collaborative Group on Hormonal Factors in Breast Cancer [3]. The study assessed epidemiological data from more than 20 countries. The study results showed that women who are currently taking COCs, as well as those who have taken them in the past 1–4 years, have a slightly increased risk of developing breast cancer. The study highlighted that women participating in the experiment were much more likely to undergo breast examinations than women not taking COCs.
Today it is assumed that the use of COCs may act as a cofactor that only interacts with the underlying cause of breast cancer and possibly potentiates it [2].
Side effects of the drug Cyproterone
Sometimes there may be changes in body weight and sexual desire, a feeling of anxiety, depressed mood, depression, increased fatigue, and decreased attention. In women, combination therapy using cyproterone causes temporary suppression of ovulation and prevents conception, sometimes - engorgement of the mammary glands, and very rarely - liver dysfunction. When using cyproterone in men, the ability to fertilize decreases, recovering 3-4 months after stopping treatment. Very rarely, liver dysfunction and gynecomastia are noted, sometimes together with increased tactile sensitivity of the nipples of the mammary glands. In rare cases, during the use of cyproterone, benign and, extremely rarely, malignant liver tumors develop.
Vaginal ring
The hormonal vaginal ring (NovaRing) contains etonogestrel and ethinyl estradiol (daily release 15 mcg + 120 mcg, respectively). The ring is installed for three weeks, after which it is removed and a week-long break is maintained. On day 29 of the cycle, a new ring is inserted.
The dosage of ethinyl estradiol in the vaginal ring is lower than that of COCs, due to the fact that absorption occurs directly through the vaginal mucosa, bypassing the gastrointestinal tract. Due to the complete suppression of ovulation and regular release, independent of the patient, the effectiveness is higher than that of COCs (0.3–6%). Another advantage of the ring is the low likelihood of dyspeptic side effects. Some patients experience vaginal irritation and discharge. In addition, the ring may accidentally slip out.
The effect of hormonal contraceptives on libido has not been sufficiently studied; research data are contradictory and depend on the average age in the sample and gynecological diseases, the drugs used, and methods for assessing the quality of sexual life. In general, 10–20 percent of women may experience a decrease in libido while taking medications. In most patients, the use of GCs does not affect libido [10].
Acne and hirsutism usually have low levels of sex hormone binding globulin (SHBG). COCs increase the concentration of this globulin, having a beneficial effect on the condition of the skin.
Special instructions for the use of the drug Cyproterone
Before starting treatment for androgenization phenomena in women, it is recommended to conduct a general medical and gynecological examination (including the mammary glands), and pregnancy should also be excluded. If intermenstrual bleeding occurs, treatment should not be interrupted; it usually stops on its own. In case of heavy and repeated bleeding, a gynecological examination is necessary to exclude organic diseases of the female genital organs. During treatment, liver function, adrenal cortex, and peripheral blood composition should be regularly monitored. During pregnancy and breastfeeding, the use of cyproterone is contraindicated. Taking the drug during pregnancy may cause signs of feminization in male newborns.
Cyproterone-Teva
Use strictly as prescribed by a doctor!
The patient should be informed of the need to inform the doctor about the use of any other medicinal product.
Before starting treatment with cyproterone, the patient is recommended to undergo a general medical examination, including determination of the peripheral blood formula, urine analysis, glucose concentration in blood plasma and urine, indicators of the blood coagulation system, blood pressure, body weight, determination of the functional state of the liver and adrenal glands. Women should undergo a comprehensive endocrinological and gynecological examination, including examination of the mammary glands, ovarian function, cytological examination of cervical mucus, and it is also necessary to exclude pregnancy. With long-term use of cyproterone, these diagnostic measures are recommended to be carried out every 6 months.
Overweight patients are advised to consult a nutritionist.
In patients with diabetes mellitus, treatment is carried out under constant medical supervision, because Dosage adjustment of insulin and other hypoglycemic drugs may be required. Monitoring of liver function in patients with diabetes mellitus should be performed approximately every 8 weeks.
Rare cases have been described after the use of cyproterone, when life-threatening intra-abdominal bleeding occurred in patients with benign and malignant liver tumors. Treatment with cyproterone should be stopped if there are signs of hepatoma - liver enlargement, pain and a feeling of heaviness in the epigastric region of the abdomen. With long-term use of cyproterone at a dose of 200-300 mg/day, its hepatotoxic effect (jaundice, hepatitis and liver failure) may occur, which in several cases has led to death. Most of the reported cases involved elderly patients with prostate cancer. The hepatotoxic effect of cyproterone is dose dependent and usually develops after several months of treatment. If the development of hepatotoxicity is suspected, a liver function test should be performed. If toxic liver damage is confirmed, the use of cyproterone should be discontinued, unless hepatotoxicity is due to another cause. for example, prostate cancer liver metastasis. In this case, continuation of treatment is possible provided that the expected benefit from the use outweighs the possible risk.
Cyproterone is not recommended for use in diseases accompanied by exhaustion (cachexia), due to the fact that catabolic reactions in the body may increase.
Isolated cases of vascular thromboembolism during treatment with cyproterone have been described. However, a cause-and-effect relationship with cyproterone has not been established. However, patients with a history of deep vein thrombosis, pulmonary embolism, myocardial infarction, cerebrovascular accident or advanced malignancy are at high risk of recurrent thromboembolism while using cyproterone.
Several reports contained information about the occurrence of meningioma with long-term use of cyproterone at a dose of more than 25 mg/day. If a patient is diagnosed with meningioma, use of cyproterone should be discontinued.
Very rarely, when using the drug in high doses, shortness of breath may occur. This may be due to the stimulatory effect of progesterone and synthetic progestogens on respiration, which is accompanied by hypocapnia and compensatory respiratory alkalosis. Symptoms disappear after discontinuation of cyproterone without special treatment.
During the use of cyproterone, it is necessary to regularly evaluate the state of adrenocorticosteroid function due to the fact that in experimental studies using high doses of cyproterone, its decrease was noted due to the manifestation of the cortico-like effect of cyproterone.
Patients with rare hereditary diseases such as galactose intolerance, lactase deficiency, glucose-galactose malabsorption should not take the drug.
When cyproterone is used in men for several weeks, spermatogenesis is often suppressed due to the antiandrogenic and antigonadotropic effect of cyproterone - the number of sperm decreases and the volume of ejaculate decreases. Sexual desire and potency are also very often reduced. Spermatogenesis gradually recovers over 3-5 months. after discontinuation of cyproterone, in some patients, restoration of spermatogenesis may occur within 20 months. It is not yet known whether spermatogenesis can be restored after a very long period of treatment. In 10-20% of cases, men experience gynecomastia, which usually decreases when the drug is discontinued or reduced.
In men of reproductive age, before starting treatment with cyproterone, it is necessary to evaluate the spermatogram. During treatment with the drug, the decrease in spermatogenesis occurs gradually, so cyproterone should not be used as a male contraceptive.
With simultaneous consumption of alcohol in patients with pathologically increased sexual desire, a decrease in the effect of cyproterone therapy may be observed. In patients with alcoholism, treatment with cyproterone for hypersexuality and pathological deviations in sexual behavior is usually ineffective.
Since sexual and androgenic activity are not identical, suppression of androgenic activity is not always accompanied by suppression of sexual desire. Comprehensive treatment is required using psychotherapeutic and sociotherapeutic methods in close collaboration with the patient’s spouse. If appropriate measures are taken, the use of cyproterone to suppress sexual activity can produce positive results.
In patients with organic brain lesions or mental illnesses with deviations in sexual behavior, cyproterone has no clinical effectiveness.
In women, the use of cyproterone should only be carried out under the supervision of an experienced physician - a specialist in the field of hormonal therapy.
Cyproterone should not be used in young women who have not yet completed the formation of a normal menstrual cycle.
Before starting treatment, pregnancy must be completely excluded. If menstrual bleeding stops during treatment, the drug should be discontinued until pregnancy is completely ruled out. During treatment with the drug, pregnancy should not occur. In this regard, women of reproductive age should always use effective methods of contraception when taking cyproterone. It is recommended to take a combined estrogen-progestogen PC in the minimum possible dose of ethinyl estradiol 30-35 mcg. When taken in combination with a PC, you should read the appropriate instructions for medical use.
The use of cyproterone in women suffering from diseases that can aggravate the course of pregnancy (epilepsy, chorea, otosclerosis, multiple sclerosis, porphyria, diabetes mellitus and arterial hypertension) should only be carried out under the supervision of a physician, regardless of how cyproterone is used, as monotherapy or from PC.
In patients with gastrointestinal disorders accompanied by vomiting and/or diarrhea, it is not always possible to prevent pregnancy when using PCs. Despite this, treatment should not be stopped. Until the end of the treatment cycle, it is recommended to use barrier methods of contraception (condoms) as additional contraceptive measures. If there is no menstrual bleeding during a one-week pause in taking the drug, the drug should be discontinued until pregnancy is ruled out.
Taking cyproterone should not be stopped if bleeding in the form of “smearing” is observed outside the weekly break period. In case of heavy and repeated bleeding, a gynecological examination is necessary.
The use of cyproterone in combination with estrogens increases the risk of thrombosis. This fact must be taken into account when using cyproterone in women requiring surgical treatment. It is recommended to interrupt treatment with cyproterone 6 weeks before the planned surgery. During periods of prolonged bed rest, cyproterone should be suspended.
Women at the beginning of treatment with cyproterone often experience tenderness or a feeling of tension in the mammary glands or their enlargement, irregular menstrual bleeding or amenorrhea. There is often a decrease in sexual desire.
Due to decreased function of the sebaceous glands, dry skin may occur.
There were no negative effects of cyproterone on the fertility of patients after cessation of treatment.
Patients who have not reached puberty (the adverse effects of cyproterone on the growth of the patient and the formation of his endocrine system cannot be excluded) should not take cyproterone.
Considering the medical and social significance of the effects of cyproterone, it is recommended to obtain informed consent from the patient before starting treatment.