Carboplatin is a chemotherapy drug from the group of second-generation platinum drugs, which are also classified as alkylating agents. This is one of the most common groups of chemotherapy drugs; they are used for many cancer diseases. This treatment is often called "platinum chemotherapy."
Other platinum drugs: cisplatin, oxaliplatin, lipoplatin, satraplatin, nedaplatin, picoplatin, cycloplatam, triplatin tetranitrate.
Carboplatin is marketed under the commercial name Paraplatin. Let's talk about what types of cancer this drug is used for, how it is treated, what side effects are possible, and how they can be prevented and controlled.
Pharmacological properties of the drug Carboplatin
Antitumor agent. It is an inorganic complex compound of platinum. The mechanism of action is due to interaction with DNA with the formation of intra- and interhelical cross-links, which change the structure of DNA and suppress its synthesis. After intravenous administration for 1 hour, the pharmacokinetic parameters of free and total platinum are described by a two-phase pharmacokinetic model. Protein binding in the first 4 hours is 29%, after 24 hours it is 85–89%. Basically (up to 32% of the dose) is excreted unchanged in the urine. For free platinum, the half-life in the initial phase is about 90 minutes, and in the terminal phase - about 60 hours. The half-life of total platinum in the initial phase coincides with this indicator for free platinum, but in the terminal phase it can exceed 24 hours.
How does carboplatin destroy cancer cells?
Among all platinum drugs, the mechanism of action of cisplatin is the best studied. Carboplatin is thought to act in much the same way. It binds to DNA, promotes the formation of cross-links within the helix and between chains, between DNA and protein molecules. Because of this, damaged DNA cannot be repaired and its replication (synthesis of new DNA), which is necessary for cell division, is disrupted. The cancer cell stops reproducing, and apoptosis—programmed cell death—starts.
Use of the drug Carboplatin
Carboplatin is administered only intravenously through a short infusion over 15–60 minutes. Pre-dissolve in 5% glucose solution or 0.9% sodium chloride solution to a final concentration of 0.5 mg/ml. Adults with normal renal function who have not previously received treatment are administered at a dose of 400 mg per 1 m2 of body surface over 15–60 minutes. The course of therapy can be repeated no earlier than after 4 weeks. In patients receiving drugs that have a myelosuppressive effect, in patients after radiation therapy, as well as in people in serious condition, the initial dose should be 300–320 mg/m2. In patients over 65 years of age, the dose of carboplatin should be adjusted taking into account their general condition. For patients with increased risk factors (testicular tumors and metastatic breast cancer), a high therapeutic dose of 1200–2100 mg/m2 (followed by bone marrow transplantation) can be administered as a long-term infusion; infusion time is 1–24 hours depending on the chemotherapy regimen. In patients with impaired renal function (creatinine clearance less than 60 ml/min), the dose of carboplatin should be reduced and adapted to the level of glomerular filtration.
How is treatment carried out?
Carboplatin is administered intravenously in different ways:
- Through an IV.
- Through a central venous catheter.
- Through the infusion port system. It is a small container shaped like a coin. One of the walls of this tank is represented by a membrane made of polymer material. The doctor makes an incision in the skin, places a reservoir inside and connects it with a catheter to the vein. The wound is sutured. Subsequently, when the drug needs to be administered, the skin with the membrane is pierced with a special needle. Typically, infusion port systems are used in patients who require long-term treatment.
The drug administration procedure lasts about an hour.
Carboplatin chemotherapy is given in cycles. The patient is administered the drug, after which they take a break of 3-4 weeks - this is the duration of the cycle. Such “breathes” are needed so that the body can recover - after all, chemotherapy drugs damage not only cancer cells, but also rapidly multiplying healthy cells.
Typically, the course of treatment consists of 4–6 cycles.
It is important to correctly calculate the dosage and schedule of administration of the chemotherapy drug. The attending physician must take into account the patient’s height and weight, general health, concomitant diseases, and individual tolerance.
Sometimes, for example, for ovarian cancer, carboplatin is administered intraperitoneally - through a puncture in the abdominal wall.
Information for healthcare professionals
On average, carboplatin remains in the blood for 3.5 hours.
The concentration of platinum in the drug molecule in the blood plasma significantly exceeds its concentration in free form.
Carboplatin binds to plasma proteins and leaves the body for a long time, mainly through the kidneys. Its half-life is at least 5 days. In patients with a creatinine clearance (CC) of 60 ml/min or more, approximately 70% of the administered dosage is excreted in urine after 12–16 hours. Platinum is found in carboplatin in 24-hour urine, and only 3 to 5% of the administered dosage is excreted in the urine after 24 to 96 hours. As CC decreases, renal clearance of the drug also decreases. Therefore, in patients with CC less than 60 ml/min, carboplatin dosages should be reduced.
Side effects of the drug Carboplatin
Leukopenia, thrombocytopenia, anemia; increased concentrations of creatinine, urea, uric acid in the blood plasma; nausea, vomiting (may develop 6–12 hours after administration and usually disappear within 24 hours), diarrhea, constipation, increased activity of liver enzymes; paresthesia, decreased deep tendon reflexes, decreased hearing in the high frequency range; disturbances of water and electrolyte balance (hypomagnesemia, hypokalemia, hypocalcemia); allergic reactions (erythematous rash, itching, fever); alopecia, flu-like syndrome, reactions at the injection site.
Special instructions for the use of the drug Carboplatin
Treatment with carboplatin can only be carried out by specialists with experience in therapy with cytotoxic drugs. The drug is prescribed with caution to patients with impaired renal function. In this category of patients, as well as in elderly people, patients who have previously received chemotherapy, and with prolonged immobilization of patients, the risk of myelotoxicity is increased. In these cases, the dose should be reduced and the composition of peripheral blood should be carefully monitored. The maximum decrease in platelet levels usually occurs between 14 and 21 days after the start of treatment, and in leukocytes - between 14 and 28 days. The minimum level should be: for platelets - 50,000 per 1 mm3, for leukocytes - 2000 per 1 mm3. If the cell count is below this level, then therapy should be suspended until normal values are restored (usually 5-6 weeks). In severe cases, maintenance transfusion therapy may be required. To avoid profound myelosuppression, repeated courses of carboplatin treatment should not be repeated under normal conditions more than once a month. Neurological examination and monitoring of hearing function should be performed regularly during and after treatment with carboplatin. Women of childbearing potential receiving carboplatin should use reliable contraception. Carboplatin has mutagenic, embryotoxic and teratogenic effects. Personnel should take special precautions when handling carboplatin.
Current aspects of the use of carboplatin in modern chemotherapy of solid tumors
Published in the journal “Effective pharmacotherapy in oncology, hematology and radiology” No. 2/2010
A.Yu. Mashchelueva, M.E. Abramov
Russian Oncology Research Center named after. N.N. Blokhina
Currently, a wide range of antitumor drugs are used in modern oncology. One of the most important and frequently used is carboplatin.
The history of the discovery and development of platinum preparations begins in 1969, when the American chemist Rosenberg, working with platinum electrodes lowered into liquid, saw that the microorganisms in the liquid stopped dividing. He did an analysis and realized that platinum salt, a long-known chemical compound of platinum, had formed there. This is how the idea of developing new antitumor drugs based on platinum arose, which received the opportunity for particularly rapid development in the last 20 years, when various platinum derivatives were created: cisplatin, cycloplatam, carboplatin, oxaliplatin. All these drugs are currently widely used as part of chemotherapy regimens for various nosologies.
Platinum drugs have a similar mechanism of action, based on the formation of covalent bonds with cell DNA, mainly with the nitrogen atom in the seventh position of guanine and adenine. One carboplatin molecule combines with two nucleotides, forming a cross-link, usually within one DNA strand (90%), less often between strands (5%). This leads to disruption of DNA synthesis and functions. The cytotoxicity of carboplatin is also due to binding to nuclear and cytoplasmic proteins. The effect does not depend on the period of the cell cycle [1].
The most common side effects include the following. From the gastrointestinal tract - nausea, vomiting, abdominal pain. Possible complications from the nervous system and sensory organs are peripheral polyneuropathy, asthenia, convulsive syndrome. However, compared to cisplatin, the neurotoxicity of carboplatin is much less pronounced and occurs in 1-6% of cases. From the cardiovascular system and hematopoietic organs - myelosuppression (thrombocytopenia is most often observed, leukopenia, neutropenia, anemia is less common). From the respiratory system - shortness of breath, bronchospasm, cough. From the genitourinary system - impaired renal function. On the part of the skin - in rare cases, the development of alopecia and an allergic reaction in the form of itching and urticaria is possible. On the metabolic side, hypomagnesemia, hypocalcemia, changes in sodium concentration, hypokalemia, increased alkaline phosphatase activity, AST levels, creatinine, total bilirubin, and decreased creatinine clearance occur.
Until recently, the standard chemotherapy for ovarian cancer was the regimen of cisplatin + cyclophosphamide, but based on the results of further studies, it was found that the combination of taxanes and cisplatin is superior to it by increasing the frequency of objective effect (from 64% to 77%), the median time to progression (13 and 18 months) and overall survival (24 and 38 months), respectively [2].
The next step was the replacement of cisplatin with carboplatin due to the pronounced nephro- and neurotoxicity, as well as the emetogenicity of the former. A comparative analysis showed that the use of carboplatin in combination with taxanes did not worsen treatment results, but a decrease in the frequency and intensity of toxic side effects was observed [3,4].
The equal effectiveness of carboplatin and cisplatin in the treatment of epithelial ovarian tumors was confirmed in several randomized studies, such as Alberts (342 patients), Ten Bokkel (339 patients), Edmondson (103 patients).
The above facts have led to the fact that the use of taxol and carboplatin has now become the “gold standard” of drug treatment for ovarian cancer.
Calculating the dose of carboplatin using the Calvert formula (AUC 5-7) allows treatment with minimal toxicity and greatest effectiveness [5,6].
Returning to the topic of scientific monitoring of the use of drugs and their implementation in practice, it should be noted that after the establishment of taxanes and carboplatin as the optimal treatment regimen for ovarian cancer in the treatment of this pathology, there was a certain lull in the treatment of this pathology, which was disrupted by the GOG 182 study, the goal of which was to improve results first-line chemotherapy by adding a third drug to the combination of paclitaxel and carboplatin. However, carboplatin remained an unchanged component of the regimens.
A total of 4312 patients with stage III-IV epithelial ovarian cancer after cytoreductive surgery were included in the study. The study design is presented in Table 1.
Table 1
. GOG Study 182. Chemotherapy regimens.
| Group 1 (control) | Carboplatin AUC × 6 Paclitaxel 175 mg/m2 3 hours every 3 weeks × 8 courses |
| Group 2 | Carboplatin AUC × 5 1 day Paclitaxel 175 mg/m2 3 hours 1 day Gemcitabine 800 mg/m2 days 1 and 8 every 3 weeks × 8 courses |
| Group 3 | Carboplatin AUC × 5 Paclitaxel 175 mg/m2 3 hours Doxil 30 mg/m2 every 3 weeks × 8 courses |
| Group 4 | Carboplatin AUC × 5 Day 3 Topotecan 1.5 mg/m2 1-3 days every 3 weeks 4 courses then Carboplatin AUC × 6 Paclitaxel 175 mg/m2 3 hours every 3 weeks × 4 courses |
| Group 5 | Carboplatin AUC × 6 Day 8 Gemcitabine 1000 mg/m2 Days 1 and 8 every 3 weeks × 4 courses then Carboplatin AUC × 6 Paclitaxel 175 mg/m2 3 hours every 3 weeks × 4 courses |
However, the study showed that the addition of a third drug did not improve treatment outcomes and significantly increased hematological toxicity [7].
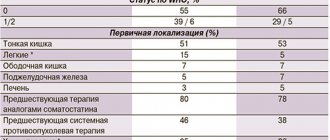
table 2
. Preliminary results of the GOG 182 study.
| Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | |
| Time to progression | 16.1 months | 16.4 months | 16.4 months | 15.3 months | 14.4 months |
| Lifespan | 40.0 months | 40.4 months | 40.8 months | 39.1 months | 40.2 months |
| Neutropenia grade 4 | 59 | 74 | 69 | 57 | 56 |
| Thrombocytopenia grade 3-4. | 22 | 64 | 38 | 36 | 58 |
The same conclusion was reached by Italian researchers who, in a randomized study, compared the efficacy and toxicity of the combination of carboplatin and paclitaxel with the combination of topotecan, carboplatin and paclitaxel. The addition of topotecan did not prolong the time to progression, but increased the hematological toxicity of therapy [8].
A study was conducted in Greece in which doxorubicin was added to a combination of cisplatin and paclitaxel. The control group received paclitaxel and carboplatin. The median duration was 44 and 37 months, respectively; the difference was not statistically significant. Regarding toxicity, an increase in the degree and duration of neutropenia was observed. Thus, it was concluded that the triple combination does not lead to a significant improvement in the results of therapy for patients with ovarian tumors compared to the standard one [9].
The next step towards improving the results of chemotherapy for ovarian cancer was the attempt to add bevacizumab, an antibody to VEGF that inhibits the angiogenesis of tumor vessels, to the standard “carboplatin + paclitaxel”. Thus, in a study by Cannistra et al. bevacizumab at a dose of 15 mg/kg IV once every 3 weeks was prescribed to patients with progression after treatment with topotecan and liposomal doxorubicin. The study included 44 patients, of whom 7 (16%) showed an objective effect from the drug. Acute intestinal perforation was noted in 5 (11%) patients, and arterial thromboembolism was noted in another 4 (9%) patients [10].
These data demonstrate the effectiveness of this triple combination, but the reported serious adverse side effects significantly limit the possibility of adding bevacizumab to therapy in treatment-naïve patients. In this regard, the leading role of the combination of carboplatin and taxanes in the first-line treatment of ovarian cancer has been almost completely established.
Undoubtedly, the use of platinum drugs, including Carboplatin-Ebeve, remains fundamentally important in the treatment of ovarian cancer. But regarding the broader discussion of the use of carboplatin, it is possible to consider its use in the treatment of other types of cancer pathologies. In particular, quite good results were obtained when studying combinations of carboplatin with other drugs in the treatment of non-small cell lung cancer.
The combination of platinum derivatives and taxanes is currently recognized as the standard of care for first-line treatment of non-small cell lung cancer. When considering the choice of a specific platinum derivative, cisplatin is usually used in combination with taxanes. However, when analyzing the results of treatment of 1489 patients who received chemotherapy containing cisplatin and 1479 patients who received carboplatin, it was concluded that patients with disseminated NSCLC can be prescribed both cisplatin and carboplatin. The rate of objective effect was significantly higher in the cisplatin group – 30% and 24%, respectively. At the same time, the better immediate efficacy of cisplatin did not lead to an increase in life expectancy compared with carboplatin. When cisplatin was prescribed, patients were more likely to experience nausea, vomiting, and signs of nephrotoxicity, while when carboplatin was prescribed, the only common toxicity was thrombocytopenia. Thus, we can conclude that the inclusion of carboplatin in the treatment regimen for disseminated NSCLC does not worsen long-term results, but is better tolerated, thereby not having a negative impact on the quality of life of patients [11,12].
Another study by Eleni M. Karapanagiotou et al. discussed the combination of carboplatin and pemetrexed in the adjuvant treatment of resectable patients with stage IB, II and IIIA non-small cell lung cancer after surgical treatment. The following regimen was chosen: carboplatin AUC 5 and pemetrexed days 1 and 14 for a total cycle length of 28 days. This study resulted in a time to progression of 26 months with moderate, manageable toxicity. Based on this, it was concluded that the combination of carboplatin and pemetrexed is not inferior in effectiveness to other regimens, but has less toxicity, which contributes to its wider implementation in practice [13].
It is impossible not to note the importance and relevance of discussing the issue of using carboplatin in the treatment of breast cancer. A number of studies have shown that the addition of carboplatin to trastuzumab and paclitaxel therapy in the first line of Her-2-positive disseminated breast cancer is more effective than the combination of trastuzumab and paclitaxel. When comparing the two given regimens, the objective response rate was 53% in the trastuzumab + paclitaxel group and 62% in the trastuzumab + paclitaxel + carboplatin group, respectively [14].
Triple negative breast cancer (ER, PR, HER2-negative) deserves special attention in modern practice. For these patients, chemotherapy alone remains the only treatment option. Currently, evidence has accumulated in the literature that triple negative breast cancer is highly sensitive to platinum agents. Thus, at ASCO 2007, the results of using the combination of taxanes + carboplatin in patients with initially existing metastases, as well as relapses of triple negative breast cancer, were reported. 57% of patients had a partial effect of therapy. The median time to tumor progression was 16 weeks (range, 4 to 28 weeks). These data provided preliminary evidence of the effectiveness of carboplatin-containing chemotherapy regimens in the treatment of triple-negative breast cancer [15].
Quite good results were also shown by a weekly regimen of neoadjuvant chemotherapy for breast cancer with the inclusion of Carboplatin-Ebeve when it was impossible to use anthracyclines [16].
An interesting pilot study was the use of carboplatin in combination with navelbine and interleukin-2 (IL-2). Melanoma is known to be a tumor characterized by low sensitivity to chemotherapy, and patients with advanced metastatic disease have a poor prognosis. There is evidence that platinum preparations and vinca alkaloids have shown some effectiveness in the treatment of disseminated melanoma. Interleukin-2 has been suggested to increase tumor sensitivity to chemotherapy. Twenty-two patients were included in the study, 11 of whom had disseminated cutaneous melanoma, 6 had iris melanoma, and 3 had metastatic melanoma without an identified primary site. As a result of treatment with carboplatin, vinorelbine and interleukin-2, 1 patient had a partial response, 9 patients had stable disease for a median of 6 months (range, 3.0 to 8.6 months). The median time to progression in all patients was 1.8 months (range, 0.7 to 8.6 months), and the median survival was 7.2 months (range, 1.4 to 42.0 months). Toxicity was moderate, quite manageable and manifested mainly by myelosuppression. Thus, it was concluded that the use of carboplatin in combination with vinorelbine and interleukin-2 could be considered as second-line chemotherapy in patients who have progressed after treatment with dacarbazine [17].
The effectiveness of carboplatin monotherapy was also shown in a study by Krege et al. for the treatment of stage IIA/B seminoma. The study included 108 patients with the indicated stages of the disease. All patients had not previously received treatment for seminoma. Treatment was with carboplatin AUC 7 mg min/mL every 4 weeks for three cycles in stage IIA (n=51) or four cycles in stage IIB (n=57). Patients with residual tumor greater than 3 cm after treatment were scheduled to undergo surgical treatment. As a result, a complete effect was registered in 88 (81%) patients, partial regression in 17 (16%), 2 (2%) patients had stable disease, and progression was recorded in one case. As for toxicity, the main type was grade III-IV hematological toxicity, the development of nausea and vomiting was noted in only 10% of cases. Despite the fact that during an average follow-up of 28 months, 13% of patients showed progression of the disease (all patients had a partial effect during carboplatin therapy, and subsequent relapse was noted in the retroperitoneal lymph nodes), the use of carboplatin was considered quite effective and safe [18].
A good balance of efficacy and, so to speak, acceptable toxicity of carboplatin in combination with gemcitabine was demonstrated in a multicenter phase II study, which included 50 patients with locally advanced or metastatic pancreatic cancer. The treatment regimen consisted of gemcitabine 800 mg/m2 on days 1 and 8 and carboplatin AUC 4 on day 8 of each three-week cycle. On average, patients received 6 cycles of treatment. Of the 35 patients who responded to treatment, 8 (17%) had partial response, 15 (32%) and 12 (25%) had stabilization and progression, respectively. At the same time, the median time to progression was 4.4 months, the median overall survival was 7.4 months, and the one-year survival rate was 28%. Toxicity of the regimen was minor and predictable (8% anemia, 6% neutropenia, and 13% thrombocytopenia). However, it should be noted that the clinical effect was significantly expressed after 2 cycles of treatment and manifested itself in a decrease in the intensity of the pain syndrome and, as a consequence, a decrease in the amount of painkillers, as well as an increase in body weight. Taking into account the presented results, we can conclude that the use of carboplatin, including Carboplatin-Ebeve, in combination with gemcitabine for the treatment of patients with locally advanced and metastatic pancreatic cancer is advisable and effective. Again, it is worth noting that the described regimen has an acceptable toxicity profile, which, in turn, is also of fundamental importance for its further use in practice [19]. Carboplatin in combination with paclitaxel in the treatment of patients with esophageal cancer [20], in the same combination in the treatment of uterine carcinosarcoma [21], and in combination with raltitrexed in the treatment of metastatic squamous cell carcinoma of the head and neck [22] also demonstrates fairly high efficacy and good tolerability.
In onco-ophthalmological practice, carboplatin has proven itself well in the treatment of retinoblastoma [23].
Thus, to summarize the above, it is necessary to conclude that the experience of using carboplatin, both foreign and domestic, is quite large; the described points are just some examples of successful clinical trials. In addition, we can say that carboplatin, including Carboplatin-Ebeve, as a representative of the “family” of platinum drugs, is currently widely and successfully used to treat various oncological pathologies. Research is ongoing to include carboplatin in new combinations.
Bibliography
- E. Chu, Vincent T. DeVita, Jr. Chemotherapy drug manual. 2007 by Jones and Bartlett Publishers.
- McGuire WP, Hoskins WJ, Brady MF et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and IV ovarian Cancer. N Engl J Med. 1996; 334:1-6.
- Ozols, RF, Bundy BN, Fowler J et al. Randomized phase III study of cisplatin/paclitaxel versus carboplatin/paclitaxel in optimal stage III epithelial ovarian cancer: a Gynecologic Oncology Group Trial (GOG 158). In: Program and abstracts of the American Society of Clinical Oncology 35th Annual Meeting; May 15-18, 1999; Atlanta, Georgia. Abstract 1373.
- Lokich J, Anderson N. Carboplatin versus cisplatin in solid tumors: An analysis of the literature. Ann. Onc., Jan 1998; 9: 13-21.
- Alberts DS, Green S, Hannigan EV et al. J Clin Oncol 1992, 10: 716-720.
- Swenerton K, Jeffrey J, Stuart G et al. J Clin Oncol 1992, 10: 718-722.
- Bookman MA. GOG0182-ICON5: 5-arm phase III randomized trial of paclitaxel (P) and carboplatin (C) vs combinations with gemcitabine (G), PEG-lipososomal doxorubicin (D), or topotecan (T) in patients (pts) with advanced- stage epithelial ovarian (EOC) or primary peritoneal (PPC) carcinoma. Proc Am Soc Clin Oncol. 2006; 24:256s. Abstract 5002.
- Scarfone G, Scambia G, Raspagliesi F et al. A multicenter, randomized, phase III study comparing paclitaxel/carboplatin (PC) versus topotecan/paclitaxel/carboplatin (TPC) in patients with stage III (residual tumor > 1 cm after primary surgery) and IV ovarian cancer (OC). Proc Am Soc Clin Oncol. 2006; 24:256s. Abstract 5003.
- Aravantinos G, Fountzilas G, Kalofonos HP. Carboplatin and paclitaxel versus cisplatin, paclitaxel and doxorubicin for frontline chemotherapy of advanced ovarian carcinoma (AOC): A Hellenic Cooperative Oncology Group Study. Proc Am Soc Clin Oncol. 2006; 24:274s. Abstract 5074.
- Cannistra SA, Matulonis U, Penson R et al. Bevacizumab in patients with advanced platinum-resistant ovarian cancer. Proc Am Soc Clin Oncol. 2006; 24:257s. Abstract 5006.
- Ardizzoni A, Tiseo M, Boni L et al. CISCA (cisplatin vs. carboplatin) meta-analysis: an individual patient data meta-analysis comparing cisplatin versus carboplatin-based chemotherapy in first-line treatment of advanced non-small cell lung cancer. Proc Am Soc Clin Oncol. 2006; 24:366s. Abstract 7011.
- Treat JA, Gonin R, Socinski MA, Edelman MJ et al. A randomized, phase III multicenter trial of gemcitabine in combination with carboplatin or paclitaxel versus paclitaxel plus carboplatin in patients with advanced or metastatic non-small-cell lung cancer. Ann. Onc., Mar 2010; 21: 540-547.
- Eleni M. Karapanagiotou, Paraskevi G. Boura et al. Carboplatin-Pemetrexed Adjuvant Chemotherapy in Resected Non-small Cell Lung Cancer (NSCLC): A Phase II Study. Anticancer Res, Oct 2009; 29: 4297-4301.
- Edith A. Perez. Carboplatin in Combination Therapy for Metastatic Breast Cancer. Oncologist, Sep 2004; 9: 518-527.-
- Chia JW, Ang P, See H, Wong Z, Soh L, Yap Y, Wong N. Triple-negative metastatic/recurrent breast cancer: Treatment with paclitaxel/carboplatin combination chemotherapy. ASCO Meeting Abstracts, Jun 2007; 25:1086.
- Chen XS, Nie XQ, Chen CM, Wu JY, Wu J, Lu JS, Shao ZM, Shen ZZ, Shen KW. Weekly paclitaxel plus carboplatin is an effective nonanthracycline-containing regimen as neoadjuvant chemotherapy for breast cancer. Ann. Onc., May 2010; 21: 961-967.
- Vuoristo MS, Vihinen P, Skytta T, Tyynela K, Kellokumpu-Lehtinen P. Carboplatin and Vinorelbine Combined with Subcutaneous Interleukin-2 in Metastatic Melanoma with Poor Prognosis. Anticancer Res, May 2009; 29: 1755-1759.
- Krege S, Boergermann C, Baschek R, Hinke A, Pottek T, Kliesch S, Dieckmann K.-P., Albers P, Knutzen B, Weinknecht S, Schmoll H.-J., Beyer J, Ruebben H. Single agent carboplatin for CS IIA/B testicular seminoma. A phase II study of the German Testicular Cancer Study Group (GTCSG). Ann. Onc., Feb 2006; 17: 276-280.
- Xiros N, Papacostas P, Economopoulos T, Samelis G, Efstathiou E, Kastritis E, Kalofonos H, Onyenadum A, Skarlos D, Bamias A, Gogas H, Bafaloukos D, Samantas E, Kosmidis P. Carboplatin plus gemcitabine in patients with inoperable or metastatic pancreatic cancer: a phase II multicenter study by the Hellenic Cooperative Oncology Group. Ann. Onc., May 2005; 16: 773-779.
- El-Rayes BF, Shields A, Zalupski M, Heilbrun LK, Jain V, Terry D, Ferris A, Philip PA. A phase II study of carboplatin and paclitaxel in esophageal cancer. Ann. Onc., Jun 2004; 15: 960-965.
- Powell MA, Filiaci VL, Rose PG, Mannel RS, Hanjani P, DeGeest K, Miller BE, Susumu N, Ueland FR. Phase II Evaluation of Paclitaxel and Carboplatin in the Treatment of Carcinosarcoma of the Uterus: A Gynecologic Oncology Group Study. J. Clin. Oncol., Jun 2010; 28: 2727-2731.
- Galetta D, Giotta F et al. Carboplatin in Combination with Raltitrexed in Recurrent and Metastatic Head and Neck Squamous Cell Carcinoma: A Multicentre Phase II Study of the Gruppo Oncologico Dell'Italia Meridionale (GOIM). Anticancer Res Nov 2005; 25: 4445-4449.
- Leng T, Cebulla CM, Schefler AC, Murray TG. Focal periocular carboplatin chemotherapy avoids systemic chemotherapy for unilateral, progressive retinoblastoma. Retina, Apr 2010; 30(4 Suppl): S66-8.
Drug interactions Carboplatin
Carboplatin reacts with aluminum-containing components of needles, syringes, catheters and IV drug sets to form a black precipitate, and therefore instruments made from such materials should not be used to administer carboplatin. The myelotoxic effect may be enhanced by the simultaneous use of carboplatin and other drugs that have myelosuppressive properties. An increase in related side effects may occur when carboplatin is combined with drugs that have ototoxic and/or nephrotoxic properties. Carboplatin should not be combined with complexing agents, as its antitumor activity may theoretically be reduced. The synergism of the action of carboplatin with etoposide and vindesine has been established.