Neutrophils are the largest group of granulocytes, the main function of which is phagocytosis (destruction) of pathogenic flora in the human body.
Neutropenia is a decrease in the number of neutrophils in the blood, which leads to the risk of bacterial and fungal infections.
In a healthy state, protection of the immune “borders” is provided by mature segmented neutrophils. Younger band neutrophils also help to “control” the situation, but there are much fewer of them (this is clearly visible from the results of a blood test, where normally mature neutrophils number from 42-72%, and young ones only from 1-6%).
But, in the event of certain diseases, the ratio of all types of neutrophils (segmented, band, myelocytes, metamyelocytes) is sharply disrupted, which leads to a pathological increase in neutrophils or their decrease (neutropenia).
At the same time, the number of neutrophils in human blood is not stable, unlike other cell groups of the leukocyte formula. The maturation, development and normal ratio of these granulocytes are affected not only by congenital and acquired pathologies, but also by severe emotional shock, stress, dietary disturbances, etc.
Neutropenia in children should be carefully investigated to prevent both severe pathologies and radical treatment without serious reasons.
Classification of severity of neutropenia:
- Light (1-1.5 x 109/l);
- Moderate (0.5-1 x109/l);
- Heavy (less than 0.5 x109/l).
If the level of neutrophils decreases critically, this leads to the development of infection in the intestines, mouth, thereby causing digestive system disorders, gingivitis, stomatitis, fungal skin lesions, etc.
Severe neutropenia in the presence of cancer pathology has an extremely adverse effect on the functioning of the immune system, leading to progressive inflammation and infections, including death.
General information
Neutropenia or agranulocytosis is a condition characterized by a decrease in the number of neutrophil granulocytes in the blood. With severe neutropenia in a person, the likelihood of developing fungal and bacterial infections, as well as the severity of their course, increases. With agranulocytosis, the level of leukocytes decreases to less than 1•10 per 9/L due to a decrease in the number of granulocytes (less than 0.75•10 per 9/L) and monocytes .
There are several forms of the disease depending on the pathogenesis. Speaking about neutropenia - what it is, it should be noted that this condition was first described in 1922. Currently, due to the active use of cytostatic treatment and various medications, the frequency of manifestation of this syndrome has increased.
To diagnose this condition, it is necessary to determine the number of leukocytes in the blood and the leukocyte formula. However, during the diagnostic process, it is very important to find out the cause of this manifestation in order to provide adequate treatment.
Why this condition can occur, and what treatment methods are used depending on the cause of neutropenia, will be discussed in this article.
Pathogenesis
The pathogenesis of different forms of agranulocytosis is different, and for many it has not yet been studied well enough. In autoimmune forms of the disease, the death of granulocytes occurs due to the influence of autoantibodies. In hapten agranulocytosis, the mechanism of the individual reaction of the body has not been fully studied. When haptens are administered after the first occurrence of hapten agranulocytosis, this condition will recur again.
Neutrophils
Granulocytes (neutrophils) provide protection to the body from attacks by bacteria and fungal infections. With the development of neutropenia, the response to such infections is ineffective.
The limit of the lower norm of neutrophils is 1500/μl in representatives of the Caucasian race; in people of the Negroid race this figure is slightly lower - about 1200/μl. The number of these cells is unstable - depending on the influence of various factors, it can change over a short period of time.
When the number of neutrophils decreases to <500/μl, an infectious process can develop due to the influence of endogenous microflora (in the intestines, in the mouth). If the number of these cells is reduced to <200/μl, the inflammatory response may be suppressed and typical signs of such a process (leukocytes in the urine, in the area of infection, leukocytosis) may not be observed.
In acute neutropenia , especially when combined with other factors (oncological disease, etc.), the function of the immune system is significantly impaired, which can subsequently lead to fulminant fatal infections. The risk of developing infectious processes is also affected by the integrity of the skin, mucous membranes, blood supply and tissue nutrition. People with severe neutropenia most often develop the following infectious diseases: pneumonia , furunculosis , septicemia .
The presence of places where vascular catheters were placed and injections were performed additionally increases the risk of developing skin infections. The most common pathogens are Staphylococcus aureus, coagulase-negative staphylococci, but other bacteria can also provoke the pathological process. People with agranulocytosis often develop other diseases: colitis , paraproctitis , stomatitis , otitis , sinusitis , etc. Those patients who have prolonged neutropenia after chemotherapy , stem cell transplantation, high doses of corticosteroid drugs are prone to developing fungal infections.
Infectious complications, leukopenia and neutropenia
Infectious complications, leukopenia and neutropenia
Infections are caused by the growth of various microorganisms, such as bacteria, viruses or fungi, inside the human body.
Infections can begin in any organ, but most often they occur in those parts of the body that are in close contact with the external environment, for example in the skin, mucous membranes of the digestive tract (oral cavity, esophagus, intestines), respiratory tract (larynx, trachea, bronchi, lungs) and organs of the genitourinary system. Normally, the body is protected from most pathogens of infectious diseases by the immune system, which can effectively destroy microorganisms. However, during the period of antitumor therapy, the functioning of the immune system may be disrupted - treatment methods such as radiation therapy, chemotherapy, as well as some “targeted” drugs can damage the bone marrow, in which the cells necessary for the functioning of the immune system - leukocytes - are formed. There are many forms of leukocytes, the most important of which are neutrophils - cells that play a major role in the body’s resistance when it “collides” with pathogens of bacterial infections. Poor diet, lack of sleep and stress also weaken the immune system.
The severity of suppression of the immune system function reflects the number of neutrophils in the blood. Normally, their number exceeds 2.0 * 10^9 cells per 1 liter of blood (you can also find the designation 2000 cells per 1 μl). A decrease in their number is designated by the term “neutropenia”. Depending on the severity of neutropenia, the following degrees of severity are distinguished:
- 1st degree – neutrophil count <2000 cells/μl, but more than 1500 cells/μl (<2.0*10^9/l, but ≥ 1.5*10^9);
- Grade 2 – neutrophil count <1500 cells/µl, but more than 1000 cells/µl (<1.5*10^9/l, but ≥ 1.0*10^9). With most drug regimens, a decrease in the number of neutrophils to this level is an indication for delaying the next course of treatment;
- grade 3 – neutrophil count <1000 cells/µl, but more than 500 cells/µl (<1.0*10^9/l, but ≥ 0.5*10^9);
- 4th degree – number of neutrophils <500 cells/μl, (<0.5*10^9/l);
With the development of “deep” neutropenia - degrees 3-4, you should especially carefully monitor your health and regularly measure your body temperature.
“Febrile” neutropenia – the number of neutrophils <1000/μl (<1.0*10^9/l) in combination with an increase in temperature >38.3 oC or with an increase in temperature ≥38.0, provided it persists for 1 hour and longer.
Typical symptoms of infection include: fever (temperature increased to 38 oC or higher), cough or sore throat, diarrhea, ear or sinus pain, skin rash, pain when urinating or change in urine color, genital discharge paths, etc. Be sure to consult your doctor if any of the above symptoms occur.
It is worth considering that taking certain medications, such as non-steroidal anti-inflammatory drugs such as paracetamol, aspirin, ibuprofen, as well as glucocorticosteroids (dexamethasone, methylprednisolone, prednisolone, etc.) can reduce body temperature and mask other symptoms of infection. This can lead to serious consequences; be sure to tell your doctor if you have taken or are constantly taking these or other drugs with a similar mechanism of action.
To diagnose neutropenia, a general (clinical) blood test is used; blood for analysis is taken from a finger or from a vein. If the development of an infection is suspected, depending on its clinical picture, additional examination methods are carried out, for example, urine analysis, stool analysis, chest x-ray, abdominal ultrasound, etc.
Infectious complications and “febrile” neutropenia in cancer patients are dangerous and potentially life-threatening complications. Patients receiving antitumor treatment are recommended to regularly (for example, once a week) monitor their general blood count and are advised to always have antibacterial drugs with them. Consult your doctor for more information.
What can I do to prevent the infection from developing?
Your doctor will give you advice on necessary precautions during treatment, such as the following:
- To maintain the processes of formation of leukocytes and neutrophils, good nutrition with a sufficient amount of proteins and vitamins in the diet is extremely important; eat more meat, fish, seafood and other products. Monitor your weight during treatment; if it steadily decreases, be sure to inform your doctor about this;
- Wash your hands well, especially before eating. Avoid contact with germs. Try not to contact people who have cold symptoms. Thoroughly wash everything you eat, thoroughly heat-treat all meat and fish products you eat, and wash all fruits and vegetables before eating.
- Keep your body clean. If you have a catheter or venous port, keep the skin around it dry and clean. Use only a soft toothbrush, brush your teeth well and regularly, and check your mouth for any sores. In case of trauma to the skin, for example, by cutting yourself, carefully treat the injury site. Try not to visit crowded places unless necessary.
Treatment and prevention of neutropenia
If neutropenia develops again and again during treatment, or the development of infectious complications is noted during therapy, your doctor may decide to reduce (reduce) the doses of anticancer drugs. Reducing the dose of anticancer drugs reduces their negative impact on hematopoietic processes and, in many cases, helps prevent the development of neutropenia.
The so-called “granulocyte colony-stimulating factors (G-CSF)”, for example filgrastim, peg-filgrastim, etc. G-CSF promotes the formation of immune system cells in the bone marrow.
Typically, G-CSF is administered 24 to 72 hours after chemotherapy, either subcutaneously or intravenously. Their use makes it possible to effectively maintain the number of neutrophils and leukocytes in the blood and carry out more aggressive chemotherapy. Most patients give themselves these injections themselves, the most convenient is injection under the skin of the abdomen. A lot of training materials on the technique of performing them (for example) have been published on the Internet. Discuss with your doctor whether G-CSF is appropriate for your individual case.
ATTENTION! Infectious complications arising during antitumor treatment can pose an immediate threat to life. Do not self-medicate, consult a doctor.
Classification
Depending on the severity of neutropenia, the following forms of this condition are distinguished:
- mild (neutrophil count - 1000–1500/μl);
- moderate (500–1000 µl);
- severe (less than 500/μl).
Depending on the characteristics of the process, the following forms are distinguished:
- Acute – develops quickly, over several hours or days. It results from the very rapid destruction or consumption of neutrophils.
- Chronic – develops over several months or years. As a rule, it develops due to a decrease in the production of neutrophils and excessive splenic sequestration.
Depending on the origin, the following forms of neutropenia are distinguished:
- Primary – associated with an internal lack of myeloid cells in the bone marrow.
- Secondary – associated with the influence of external factors.
According to the pathogenetic factor, the following forms of this condition are distinguished:
- Myelotoxic agranulocytosis - develops due to exposure to ionizing radiation and the influence of benzene vapor. Also, myelotoxic agranulocytosis can be a consequence of the use of cytotoxic agents.
- Immune agranulocytosis is a consequence of the influence of autoantibodies and antibodies to granulocytes after taking hapten drugs. Immune agranulocytosis can be observed with systemic lupus erythematosus , etc.
- Idiopathic form - has an unknown etiology.
Depending on the characteristics of the condition, the following forms are distinguished:
- Absolute neutropenia is a decrease in the absolute number of neutrophils in the blood. Absolute neutropenia is characteristic of a number of conditions and diseases: acute and chronic viral, bacterial and fungal diseases, autoimmune diseases, acute leukemia , lymphoma , etc.
- Relative neutropenia is a decrease in the specific gravity of neutrophils in the blood against the background of a normal or increased number of these cells.
Etiology
Neutrophils develop in the bone marrow within 15 days, remain in the bloodstream for about 8 hours, constitute the overwhelming cellular part of the leukocyte formula, and when “pests” are detected, they are immediately sent to eliminate them.
The main causes of neutropenia that disrupt this physiological process:
- Development of pathogenic flora in the body (bacteria, viruses, fungi).
- Exposure to radiation, chemotherapy.
- Pathologies in the functioning of the bone marrow.
- Folic acid deficiency.
- Congenital pathologies of internal organs, glands and systems.
Neutropenia in children can also develop due to disruption of the pancreas and retarded mental development (Shwachman-Diamond-Oski syndrome).
Neutropenia is divided into:
- Spicy;
- Chronic.
Acute neutropenia develops rapidly due to the rapid consumption/destruction of neutrophils, chronic - due to a decrease in the production of granulocytes or excessive splenic secretion.
- Primary;
- Secondary.
Primary neutropenia is associated with internal disorders (congenital pathologies, idiopathic neutropenia, cyclic neutropenia, benign ethnic), secondary - due to the influence of external factors on the maturation and development of bone marrow cells.
Causes
Granulocytopenia can develop due to a number of reasons, which depend on the type of disease.
- Myelotoxic agranulocytosis develops against the background of suppression of the production of myelopoiesis precursor cells in the bone marrow. It can develop as a result of exposure to cytostatic drugs, ionizing radiation on the body, and also develop as a result of taking other medications ( Streptomycin , Levomycetin , Gentamicin , Colchicine , Penicillin , etc.).
- Immune agranulocytosis develops due to the formation of antibodies that attack one’s own leukocytes. The development of hapten immune agranulocytosis is associated with the use of sulfonamides, NSAIDs-derivatives of pyrazolone, drugs prescribed to patients with tuberculosis , diabetes mellitus , and helminth infections . Haptens form complex compounds with blood proteins or leukocyte membranes and become antigens to which the body begins to produce antibodies. The immune form of the disease also develops in a number of diseases - influenza , yellow fever , malaria , infectious mononucleosis , viral hepatitis, typhoid fever , polio , etc.
- Autoimmune agranulocytosis develops as a result of a pathological reaction of the immune system, as a result of which antineutrophil antibodies are formed. A similar form is observed in patients with autoimmune thyroiditis , systemic lupus erythematosus , rheumatoid arthritis , etc.
- Severe agranulocytosis can develop as a result of chronic lymphocytic leukemia , aplastic anemia , Felty's syndrome .
- The congenital form of the disease develops due to genetic disorders.
Neutropenia, associated with insufficient bone marrow production, is observed in megaloblastic anemia associated with deficiency of folic acid and vitamin B 12 .
The process of neutrophil production can be disrupted by multiple myeloma, leukemia, lymphoma, or metastatic tumors.
Febrile neutropenia (neutropenic fever) is a condition that threatens the patient’s life and develops acutely. At the same time, the number of neurophils in the blood decreases to below 500/mm3. Febrile neutropenia occurs during or after cytostatic chemotherapy for leukemia, and is less common during cytostatic chemotherapy in the treatment of other cancers. It is also possible for this condition to develop after radiation therapy, etc.
Secondary neutropenia
Secondary neutropenia most often develops due to:
- Taking certain medications (antibiotics, antihistamines, antipyretics, barbiturates, analgesics);
- Development of infections;
- Immune reactions;
- Bone marrow infiltration.
Secondary neutropenia provokes pathologies:
- Liver, spleen, kidneys;
- Pancreas, thyroid gland;
- Aplastic anemia;
- Megaloblastic anemia;
- Myelodysplastic disorders;
- Myelofibrosis, leukemia;
- Sepsis, HIV, Felty's syndrome;
- Rh-conflicting neutropenia;
- Lymphoproliferative diseases, etc.
In the case of secondary neutropenia, it is not the blood “test” that needs to be treated, but the patient with specific symptomatic manifestations.
Primary and secondary neutropenia should be distinguished, since in the first case, a decrease in the level of neutrophils is the only manifestation, while secondary ones develop on the basis of infections, systemic autoimmune pathologies and onco-neoplasia.
Symptoms of neutropenia
As a rule, symptoms of neutropenia in children and adults do not develop until the infectious process begins to progress in the body.
Most often, the main manifestation of infectious processes is fever. In this case, the typical symptoms of focal inflammation - pain, swelling, redness, infiltrates - may be absent. Sometimes focal symptoms develop in adults and children, such as mouth ulcers. But they can also be insignificant.
Signs of drug-induced neutropenia may include fever, rash, and lymphadenopathy.
In general, signs of agranulocytosis may be as follows:
- Manifestation of severe weakness.
- Joint pain.
- Pale skin.
- Heavy sweating.
- High body temperature.
- Ulcerative lesions of the pharynx and oral cavity.
Signs of myelotoxic agranulocytosis, in addition to those listed above, include moderate hemorrhagic syndrome . In this case hematomas , nosebleeds and hematuria develop. Myelotoxic agranulocytosis can lead to vomiting and stool containing blood, and bleeding gums.
Signs characteristic of immune agranulocytosis, as a rule, develop acutely. The immune type of the disease is manifested by fever , weakness , and sweating . Ulcerative-necrotic processes develop in the oral cavity. As a result of lesions of the pharynx and oral cavity, stomatitis , pharyngitis , gingivitis , tonsillitis , etc. can develop. Ulcerations with a grayish coating, necrotic plaques, and ulcers on the tonsils (the so-called agranulocytic tonsillitis) appear on the mucous membrane.
lymphadenitis may develop .
Neutropenia
Oncological hospital in Moscow / Neutropenia
Cancer treatment at the Moscow Oncology Hospital
Leukocytes are blood cells that participate in the immune response. They are heterogeneous in structure and have functional differences.
Three types of leukocytes (neutrophils, basophils, eosinophils) belong to granulocytes, since they have granularity (granules) in the cytoplasm, and two types do not have granularity and are called non-granulocytes - monocytes and lymphocytes.
The leading role in protecting the body from infection belongs to the largest group of leukocytes - neutrophils. They make up 48-78% of all leukocytes, and their absolute content is usually more than 2 thousand cells/μl of blood.
They are formed in the bone marrow, where they transform into mature forms within a week and are released into the blood. They live there for a third or a quarter of the day. And all this time they counteract foreign influences on the body:
- captures and destroys solid particles;
- produce bactericidal enzymes;
- actively move to bacteria and inflammation.
Degrees of neutropenia
Neutropenia is a decrease in their number per unit volume.
The most important danger in this case is the sharply increasing threat of severe infections. Its level is directly related to the degree of neutropenia.
- I Art. – the number of neutrophils is in the range of 1.5-1.9 thousand cells/μl;
- II Art. – neutrophils 1-1.4 thousand cells/μl;
- III Art. – neutrophil content 0.5-0.9 thousand cells/μl;
- IV Art. – decrease in neutrophils less than 0.5 thousand cells. /µl
Causes of neutropenia
There are many reasons for the development of neutropenia:
- bacterial and viral infections;
- blood diseases;
- hereditary defects;
- antibacterial, antiviral, anti-inflammatory therapy.
In cancer patients, one of the main causes of neutropenia is myelosuppression (bone marrow suppression) as a result of the toxic effects of chemotherapy or radiotherapy.
It occurs in every second patient receiving these types of treatment.
The myelotoxicity of chemotherapy drugs varies. When prescribing chemotherapy, take into account:
- mechanism of action of cytostatics. Some of them (taxanes, platinum drugs, nitrosoureas) are particularly potent bone marrow depressants;
- dependence of neutropenia on the dose of cytostatic;
- higher risk of neutropenia when prescribing polychemotherapy than when treating with a single drug.
A noticeable decrease in the patient’s neutrophils begins approximately a week after the end of the next course and deepens over the next week. Then the number of neutrophils begins to increase, and by the third or fourth weeks it reaches the initial level.
Signs of neutropenia
Mild neutropenia can only be detected by a laboratory blood test and requires increased infection prevention measures.
As the number of neutrophils progressively decreases, the patient may develop signs of an infectious process:
- body temperature rises above 38 degrees;
- the patient is chilling or sweating profusely;
- sore throat or mouth, where ulcerations are possible;
- abdominal pain appears;
- there may be loose stools, ulcers on the mucous membrane and skin around the anus;
- frequent, painful urination;
- cough, shortness of breath;
- profuse vaginal discharge and itching;
- redness, soreness and swelling in the area of even minor skin damage.
Diagnosis of neutropenia
In such cases, they act as quickly as possible. Diagnosis is carried out promptly and treatment is started based on its results.
Diagnostic measures include:
- general and biochemical blood tests;
- culture of blood, urine and swabs from the oral cavity, pharynx, vagina;
- chest x-ray;
- Ultrasound of the abdominal organs.
Treatment of neutropenia
Leukopoiesis stimulants are prescribed according to strict indications, which, in accordance with international standards, are determined by the attending physician in relation to a particular patient. Most of these drugs promote the release of leukocytes from the bone marrow, but do not increase their production in it.
The most effective are two colony-stimulating factors (CSF), which actually promote the production and maturation of new neutrophils. These are granulocyte (G-CSF) and granulocyte-macrophage (GM-CSF) colony-stimulating factors.
They are indicated for patients with neutropenia if they:
- neutrophils are no more than 100 cells per 1 ml, which means the risk of life-threatening infections is extremely high;
- the tumor is progressing;
- pneumonia occurred;
- sepsis with multiple organ failure developed;
- there is a tendency to low blood pressure;
- a fungal infection was detected;
- age over 65 years.
The problem of neutropenia in cancer patients is given great importance in the European Clinic. Here they are fully aware of the threat of deadly infections against its background, as well as the obstacles to the further implementation of chemotherapy and radiotherapy. Therefore, everything necessary is being done to prevent and treat this serious complication.
Contact us
Tests and diagnostics
Doctors may suspect neutropenia in people who have frequent, severe infections or unusual infections. This condition is also highly likely to occur in patients undergoing radiation therapy and receiving cytotoxic drugs.
- Anamnesis must be taken into account: the doctor must know what medications or toxic substances the patient took.
- Granulocytopenia is determined by conducting a laboratory blood test to determine the leukocyte formula. A blood test can detect agranulocytosis.
- Culture may also be done to determine infection.
- However, in the diagnostic process, it is important not only to determine the presence of this phenomenon, but also to find out the mechanism and reason for its development. For this purpose, the doctor conducts a physical examination and questioning of the patient.
- A urine and stool test is performed.
- An informative method of investigation is chest radiography.
- People who are immunocompromised have a chest CT scan.
- Other tests are also ordered depending on signs of infection.
Bone marrow testing is performed to determine whether the development of neutropenia is due to decreased production of neutrophils by the bone marrow.
NEUTROPENA is a complication that reduces the effectiveness of chemotherapy
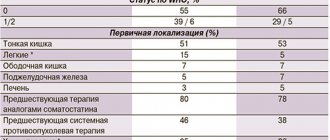
Breast cancer is a disease entity, especially early breast cancer, for which it is fundamental to administer the right regimens at the right doses and the right timing in neoadjuvant and adjuvant treatment (that is, either before surgery or after surgery, respectively). When carried out in full - and only in full, in compliance with the doses and timing of treatment - the entire planned course of chemotherapy can increase life expectancy. We are not talking about something like that now, we are talking about months, about years of life.
Fortunately, recently, to improve the results of treatment of early breast cancer - this has already been confirmed in serious large-scale studies - more “strict” drug treatment regimens have been used, which can improve long-term results, that is, increase the number of people cured, surviving and living without symptoms. patient illnesses. But these regimens, which are called dose-consolidated, involve reducing the intervals between injections. Usually, everyone is accustomed to the fact that after the administered course of chemotherapy, some interval is planned - 3-4 weeks, during which the patient usually recovers and is ready for the next administration: blood counts are restored (primarily neutrophils), because, as we have already discussed with you before This means there is a threshold, safe level of neutrophils that allows you to continue/start the next treatment cycle. If it is impossible to achieve it, we cannot begin therapy, which leads to a delay in the planned cycle.
Surveys show that, unfortunately, up to 40% of clinicians prefer to modify regimens rather than do something different. As we have already established, modification of the regimen, changing the intervals between cycles, and reducing the dose lead to a loss of effectiveness of the treatment. It has been proven, for example, that reducing the dose of adjuvant chemotherapy prescribed for early breast cancer by 15% already leads to a significant decrease in life expectancy, and reducing the dose by 35% or more, that is, by a third, completely eliminates the value of this chemotherapy. The survival rate of patients is the same as if they had not received chemotherapy at all.
Therefore, with the introduction of dose-dense chemotherapy regimens into our daily practice and taking into account that the normal bone marrow of any person in most cases does not have time to recover within this short interval, something needs to be done about this in order to carry out the desired cycle at the right time in the right dose treatment. Chemotherapy regimens, which are used specifically in the treatment of early breast cancer, when we really give a chance and must do so in order to cure the patient (we are not talking about metastatic disease, where the goals and principles of therapy are completely different), stimulate the development of neutropenia of 3-4 degrees gravity.
Developed neutropenia, as a rule, leads to a change in the treatment regimen (namely, a reduction in drug doses) and to prolongation of the intervals between cycles. If we do nothing or do it after the fact, when trouble has already happened, and not in advance, we lose the effectiveness of treatment and completely nullify all our efforts. Therefore, it has long become obvious that in order to comply with the planned treatment regimen, it is necessary to use
Treatment with folk remedies
The use of traditional methods can help improve the body's defenses, since when the number of neutrophils decreases, the body's resistance decreases. Folk remedies can be used as a complement to the main treatment, after consulting with a doctor.
- Infusion of walnut leaves . Chop young walnut leaves (30 g) and pour 300 ml of boiling water into a thermos. Leave for 12 hours, drink 50 ml of the drink once a day. It is also recommended to eat a few walnuts every day.
- Onion infusion . Mix 250 onions, pre-finely chopped, with 1 tbsp. sugar and pour a glass of water. Cook for an hour, then cool and store in the refrigerator. Consume several spoons every day.
- Herbal teas . To boost immunity, it is recommended to drink herbal tea with honey. Its composition in different variations may include chamomile, mint, strawberry and blueberry leaves, lemon balm, etc.
- Blend to boost immunity . To prepare it, mix 500 g of cranberries and apples with 200 g of sugar. Add 1 tbsp. water and bring to a boil. When the mixture has cooled slightly, add 300 g of honey. Use 1 tbsp. l. three times a day.
- Remedy for immunity with aloe . It is necessary to keep 500 g of aloe leaves from a plant at least 3 years old in the refrigerator for about 5 days. Before picking the leaves, aloe should not be watered for two weeks. Next, the leaves should be twisted into a meat grinder, add 300 g of honey and 300 ml of Cahors. Drink 1 tbsp three times a day. l. before eating.
Prevention
- The essence of preventing agranulocytosis is to provide patients at risk of developing this condition with careful and regular hematological monitoring. This is necessary, first of all, during the period of use of myelotoxic drugs.
- It is important to exclude the use of those medications that have previously provoked manifestations of immune agranulocytosis .
- It is also important to practice general preventive measures: strengthen the body's defenses, practice physical activity, healthy eating.
- All infectious diseases should be treated promptly and under the supervision of a physician.
Neutropenia in children
Neutropenia in children under one year of age and older can occur due to various reasons. Pediatrician Komarovsky and other well-known experts note that this condition can develop as a result of severe viral, bacterial and fungal lesions, as well as exposure to radiation, radiation therapy, and toxic damage. Neutropenia in infants can also be associated with genetic disorders, as well as with treatment with drugs that interfere with hematopoiesis. A rare condition is congenital agranulocytosis , where a child develops severe immunodeficiency .
As a rule, severe symptoms of this condition do not appear in children, so most often the problems are determined only after a blood test. But if agranulocytosis is not detected for a long time, then a number of symptoms associated with intoxication of the body develop. Therefore, as pediatrician Komarovsky and other doctors note, it is important to monitor the condition of children who have an increased risk of developing neutropenia, and take timely measures to normalize the body’s condition in order to avoid complications.
Diet
Diet 13 table
- Efficacy: therapeutic effect after 4 days
- Time frame: no more than 2 weeks
- Cost of products: 1500-1600 rubles per week
If the number of neutrophils in the body is reduced, it is necessary to especially carefully monitor nutrition so as not to provoke complications dangerous to health. First of all, it is important to avoid those foods that could potentially contain germs or bacteria.
It is recommended to include the following foods in your diet:
- Pasteurized milk, yogurt, cheese.
- All types of meat and fish that have previously undergone thorough heat treatment.
- Hard-boiled eggs.
- Citrus fruits, bananas, frozen fruits.
- Porridge, pasta.
- Nuts.