Introduction
In recent decades, the incidence of neuroendocrine tumors (NETs) has been steadily increasing.
NETs are a relatively rare heterogeneous group of neoplasms with an annual incidence of 35 cases per 100,000 people. The updated WHO classification of gastroenteropancreatic (GEP) tumors verifies them depending on location, clinical manifestations and degree of differentiation. Due to their slow growth and lack of early symptoms, most NETs are often diagnosed at advanced stages, when treatment options are limited [1]. NETs occur in any organ where endocrine cells are present. These neoplasms may not produce clinical symptoms, but if they are functional, endocrine syndromes develop that pose a threat to the health and life of patients.
The goal of treating patients with NET is to eliminate the tumor itself and suppress the symptom complex caused by carcinoid syndrome. The only radical method of treatment remains surgical, and if it is impossible to use, inhibition of tumor growth and suppression of hormonal expression with somatostatin analogues (in particular, octreotide) can prolong life and improve its quality in patients.
Production[edit]
Digestive system[edit]
Somatostatin is secreted by delta cells at several locations in the digestive system, namely the pyloric antrum, duodenum, and pancreatic islets. [13]
Somatostatin, released in the pyloric antrum, travels through the portal venous system to the heart, then enters the systemic circulation to reach sites where it will exert its inhibitory effect. In addition, the release of somatostatin from delta cells may act in a paracrine manner. [13]
In the stomach, somatostatin acts directly on acid-producing parietal cells through a G protein-coupled receptor (which inhibits adenylate cyclase, thereby effectively counteracting the stimulatory effect of histamine), reducing acid secretion. [13] Somatostatin may also indirectly reduce stomach acid production by preventing the release of other hormones, including gastrin and histamine, which effectively slow down the digestive process.
Brain [edit]
| Sst is expressed in mouse telencephalon interneurons at embryonic day 15.5. Allen's Brain Atlases | Expression of Sst in the adult mouse. Allen's Brain Atlases |
Somatostatin is produced by neuroendocrine neurons of the ventromedial nucleus of the hypothalamus. These neurons project to the median eminence, where somatostatin is released from neurosecretory nerve endings into the hypothalamic-pituitary axis through the neuronal axons. Somatostatin is then carried to the anterior pituitary gland, where it inhibits the secretion of growth hormone from somatotrope cells. Somatostatin neurons in the periventricular nucleus mediate the negative feedback effects of growth hormone by their own release; Somatostatin neurons respond to high circulating concentrations of growth hormone and somatomedins by increasing the release of somatostatin, thereby decreasing the rate of growth hormone secretion.
Somatostatin is also produced by several other populations that project centrally, i.e., to other brain regions, and somatostatin receptors are expressed in many different brain regions. Specifically, populations of somatostatin neurons originate in the arcuate nucleus,[14] the hippocampus,[15] and the short-latency nucleus of the solitary tract. [ citation needed
]
Use of somatostatin analogues in the treatment of NETs
Octreotide, the first synthetic analogue of somatostatin, was initially used to correct the clinical manifestations of carcinoid syndrome. Recent studies have shown that treatment with octreotide can be not only symptomatic, but also targeted, taking into account the antitumor effects of the drug. A long-acting octreotide has been developed that provides greater ease of administration [2].
Clinical effects of extended-release octreotide
Octreotide demonstrated good effects on hormonal hypersecretion and NET growth. The drug plays a key role in the correction of symptoms caused by the secretion of neuropeptides in patients with well-differentiated carcinomas, has antitumor activity in intestinal carcinoids, significantly increasing the time of progression of NETs. Long-acting octreotide is effective both as monotherapy and in combination with chemotherapy or radionuclide therapy of peptide receptors [3]. The drug is administered once a month; it has an effective and safe antitumor and symptomatic effect while continuously maintaining concentration in the body [4–6].
Carcinoids are mainly slow-growing NETs with low proliferative activity. Octreotide remains the standard for symptomatic treatment of carcinoid syndrome, possessing antiproliferative activity and simultaneously inhibiting tumor growth. Although octreotide treatment by itself rarely results in tumor remission, it does slow tumor progression. If radical or interventional treatments for liver metastases are not possible, or the metastases are not limited to one location, then systemic treatment with somatostatin analogues remains the only option [7]. Standard conservative treatment is octreotide, interferon-α and chemotherapy. Due to the complexity of efficacy studies as well as the high potential for side effects, the widespread use of interferon-α in the treatment of metastatic NETs is limited, and high-grade NETs are not highly sensitive to chemotherapy due to low mitotic rates, high levels of the anti-apoptotic protein Bcl-2, and increased expression multidrug resistance gene. Therefore, the use of somatostatin analogues remains the most promising [8].
Somatostatin analogues are the standard of care for patients with functioning gastroenteropancreatic NETs. A decrease in hormonal hypersecretion was obtained in more than 70% of patients with malignant functioning NETs of the intestine and pancreas; stabilization of tumor growth was observed in more than 50% of patients with progressive tumor growth [9]. Gastroenteropancreatic neuroendocrine tumors (GEP NETs) are a relatively rare group of heterogeneous neoplasms with an indolent course. The use of octreotide in their treatment has radically changed therapeutic tactics. The PROMID and RADIANT-2 clinical trials confirmed the benefits of long-acting octreotide treatment for GNO: tumor size stabilized in approximately half of the cases and decreased in approximately 10% of patients. Long-acting octreotide has a robust safety profile and is well tolerated, with treatment discontinuation due to side effects rare [10–13].
The PROMID (placebo-controlled, prospective, randomized trial of patients with metastatic intestinal NETs), conducted at 18 centers in Germany and including 85 patients, demonstrated the antiproliferative effect of long-acting octreotide in well-differentiated gastrointestinal NETs, 40% of which were functioning and 60% non-functioning. , with a statistically significant increase in progression-free survival compared with placebo. Combination therapy with somatostatin analogues coupled with radionuclide therapy has also proven its effectiveness [14].
Functions [edit]
The D-cell is visible at the top right, and somatostatin is represented by the middle arrow pointing to the left.
Somatostatin is classified as an inhibitory hormone [6] and is induced by low pH. [ citation needed
] Its effects spread to different parts of the body. The release of somatostatin is inhibited by the vagus nerve. [16]
Anterior pituitary gland[edit]
In the anterior lobe of the pituitary gland, the effects of somatostatin are as follows:
- Suppressing the release of growth hormone (GH) [17] (thereby counteracting the effects of growth hormone releasing hormone (GHRH))
- Suppression of thyroid-stimulating hormone (TSH) release [18]
- Inhibition of adenylate cyclase in parietal cells
- Suppression of prolactin release (PRL)
Gastrointestinal system[edit]
- Somatostatin is homologous to cortistatin (see somatostatin family) and inhibits the release of gastrointestinal hormones.
- Reduces the rate of gastric emptying, reduces smooth muscle contraction and intestinal blood flow [17]
- Suppresses pancreatic hormone production Somatostatin release is triggered by the beta cell peptide urocortin3 (Ucn3) to inhibit insulin release. [19] [20]
- Suppresses glucagon release [19]
Possibilities for adjusting the dose of octreotide
Patients who do not respond or stop responding to standard doses of octreotide are prescribed high doses of this drug, which lead to a decrease or normalization of the production of biologically active amines and neuropeptides [15]. Search the PubMed (1998–2012) and Cochrane Library (2000–2013) databases for literature on the efficacy and safety of extended-release octreotide at doses higher than those approved by the FDA for the treatment of NETs (30 mg/month). identified 1086 publications. Eleven studies reported the use of higher doses to control symptoms and tumor progression, although symptom severity and quality of life were not quantified. 10 studies reported the effectiveness of the drug in 260 patients in a dose range of 40 mg/month. or 30 mg every 3 weeks. up to 120 mg/month. Eight studies presented expert clinical opinion on the advisability of increasing the drug dose to 60 mg/month. to control symptoms and prevent tumor progression. Eight studies examined the safety of high doses, with no increased toxicity associated with doses greater than 30 mg/month. [16].
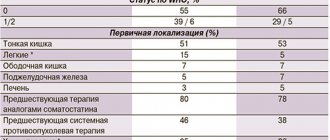
JR Strosberg et al. (2014) studied the possibility of increasing the dose of octreotide in patients with NET. Patients with carcinoid syndrome or pancreatic NET received a dose of octreotide greater than 30 mg every 4 weeks. from 2000 to 2012. Among 239 patients with NET, 53% were men, the mean age at first dose escalation was 60 years (standard deviation (SD) 11 years), time from start of dose escalation was 1.7 years (SD 2 ,0 year). The main indications for dose increases were manifestations of carcinoid syndrome or other hormonal activity (62%), as well as radiologically confirmed tumor progression (28%). The most common dose increase was 40 mg every 4 weeks. (71%) and 60 mg every 4 weeks. (18%). Of the 90 patients who experienced hot flashes before the first dose increase, 73 (81%) either stopped experiencing them altogether or reported them to be less severe. Of 107 patients with diarrhea, 85 (79%) noted its reduction or complete relief after the first dose escalation. This study showed that increasing the dose of octreotide administered could lead to improved control of carcinoid syndrome manifestations [17].
Long-acting octreotide stabilizes high-grade intestinal tumors, but survival analysis was not performed due to insufficient case numbers reported. To relieve carcinoid syndrome, high doses of the drug are often used. S. C. Lau et al. (2018) conducted a study to determine whether octreotide dose correlates with survival in patients with GNO. Overall survival was compared in 170 patients who received low (<30 mg) and high (≥30 mg) doses of octreotide. Baseline characteristics were similar in the groups: mean age 62–63 years, 50 men (58%); 46 (48%) tumors were localized in the small intestine, and 74 (66%) had liver metastases. The average time from diagnosis to initiation of treatment was 5.5 and 6.0 months. respectively. Long-acting octreotide treatment was initiated for the purpose of correcting neuroendocrine symptoms (71%), stabilizing the condition (23%), or monitoring biomarkers (6%). The median overall survival was longer in the group receiving high doses of octreotide (66 months compared with 22 months, multivariate hazard ratio (HR) 0.5; p < 0.01). Age ≥65 (HR 1.9; p<0.01) and pancreatic tumors (HR 1.7; p=0.03) were predictors of worse survival [18].
In patients with advanced NET (1999–2009) treated with long-acting octreotide for 12 months, 5-year survival was compared depending on the dose they received over 28 days, averaged over the first 3 months: low ( ≤20 mg), moderate (21–30 mg) and high (>30 mg). Among the 222 patients, 81 (36%) received low doses, 82 (37%) received medium doses, and 59 (27%) received high doses. Multivariate analysis showed that, compared with the mean, low dose was associated with significantly worse survival (HR 2.00; p=0.001), whereas high baseline dose (HR 1.09; p=0.719) showed no additional benefit compared with average. This population-based study identified a potential survival benefit of 21–30 mg in elderly patients with advanced NET [19].
K. Al-Efraij et al. conducted a retrospective review of the treatment of inoperable patients with NETs and metastases who received extended-release octreotide at a dose of 30 mg/month. and higher from 2005 to 2011. Increasing the dose of octreotide was associated with effective improvement of NET symptoms in patients who were refractory to standard doses [20].
Studies on the effectiveness of long-acting octreotide
S. Saglam et al. (2015) retrospectively reviewed the medical records of 23 patients with nonfunctional metastatic or unresectable GEP NETs who were treated with long-acting octreotide as first line at a dose of 30 mg every 4 weeks. Primary and secondary endpoints were progression-free survival (PFS) and overall survival (OS); patients were followed up for an average of 47 months. The mean PFS and OS were 25.0±3.4 months. [95% CI: 18.4; 31.5] and 71.3±9.5 months. [95% CI: 52.7; 89.9] respectively, with an estimated 5-year OS of 58%. Patients with ≤25% liver tumor burden had better PFS compared with patients with >25% (32.2±6.2 vs. 19.4±2.7 months; p=0.043). Octreotide is an effective and well-tolerated treatment option in patients with high-grade nonfunctional GEP NETs [21].
F. Cioppi et al. (2017) conducted a longitudinal, open-label study of LARO-MEN1 to evaluate the feasibility of early initiation of the drug as a prophylactic approach for the treatment of GEP NETs associated with multiple endocrine neoplasia type 1 (MEN1) syndrome. Thirty patients with MEN1 were studied, and 8 of them who had small (<2 cm) NETs and an increase in at least one gastroenteropancreatic hormone were administered extended-release octreotide 10 mg IM every 28 days. The drug showed good efficacy and safety; in most patients, tumor size remained stable over the 6-year treatment period. The study confirmed the possibility of prophylactic use of octreotide to delay or avoid surgery in such patients [22, 23].
After examining the Medicare database, C. Shen et al. (2014) identified patients aged ≥65 years who had carcinoid syndrome was diagnosed. 2450 (51%) of 4848 patients with advanced disease and 81 (10%) of 807 patients with solitary NET were prescribed long-acting octreotide for a period of 6 months. from the onset of the disease. A multivariate proportional hazards model revealed that the drug provided an increase in 5-year survival for patients with advanced stages of the disease (HR 0.61; p≤0.001) [24].
Adrenocortical cancer has a poor prognosis, and current treatment options, such as mitotane- or platinum-based chemotherapy regimens, have limited effectiveness. X. Wang et al. (2019) demonstrated a patient with metastatic adrenocortical cancer with low tolerance to mitotane who was prescribed long-acting octreotide therapy after undergoing Octreoscan scintigraphy; a good response to therapy was obtained in this patient [25].
Clinical studies have demonstrated a synergistic effect between long-acting octreotide and the protein kinase inhibitor everolimus. The activity and safety of everolimus were assessed in combination with long-acting octreotide in 50 patients with NETs of the gastroenteropancreatic tract and lungs. Patients received everolimus 10 mg/day in combination with extended-release octreotide 30 mg every 28 days. The primary endpoint was objective response rate (ORR). Primary localization of tumors: in the pancreas (14 patients), lungs (11 patients), ileum (9 patients), jejunum and duodenum (2 patients) and unknown location (14 patients); 13 (26%) patients had carcinoid syndrome. ORR was 18%; 2% of patients had a complete response, 16% had a partial response, and 74% achieved stable disease. The calculated clinical effect was 92%. Combination therapy with everolimus and octreotide was effective, well tolerated and, as the study showed, can be used as first-line therapy in patients with NET [26].
In the RADIANT-2 study, everolimus in combination with long-acting octreotide demonstrated a 5.1-month increase in survival in patients with advanced NETs manifesting as carcinoid syndrome. compared with those receiving placebo plus long-acting octreotide [27].
YM Liu et al. (2019) assessed the tumor burden that reduces the effectiveness and safety of transcatheter arterial embolization (TAE) in combination with long-acting octreotide therapy for NET metastasis to the liver. The study involved 29 patients with this pathology who were treated at Sun Yat-sen University Hospital in 2014–2018. The average age was 25–69 (50±11) years. All patients had histologically confirmed metastases of a well-differentiated tumor in the liver: 17 patients received combination therapy - TAE in combination with long-acting octreotide and 12 patients - only long-acting octreotide. The volume of liver damage was assessed according to RECIST (Response Evaluation Criteria In Solid Tumors) 1.1 criteria. It was shown that TAE in combination with long-acting octreotide was more effective in reducing tumor burden compared to octreotide monotherapy [28].
In a study conducted by G.S. Emelyanova et al. (2012), 67 patients with a morphologically confirmed diagnosis of NETs of various locations and disseminated progressive tumor process took part. Immunohistochemical examination was performed in 53 patients; 14 patients had only cytological verification of the diagnosis. Treatment was carried out with Octreotide-depot in mono mode and in combination with interferon-α at a dose of 3 million IU 3 times/week. subcutaneously 47 patients received octreotide depot at a dose of 20–40 mg: 17 as monotherapy, 30 in combination with chemotherapy. The effectiveness of treatment was assessed by controlling tumor growth. Tumor response to treatment was assessed according to RECIST criteria. Control of symptoms of carcinoid syndrome was assessed using quality of life questionnaires, changes in the frequency of hot flashes and incidence of diarrhea. Clinical response was defined as a reduction in hot flashes to less than 1 time per week and a decrease in the frequency of diarrhea to less than 4 times per day or, if diarrhea was observed 2-4 times per day, a decrease in its frequency, as well as the disappearance of abdominal pain. The symptomatic effect of Octreotide-depot was obtained in all patients; the drug made it possible to control the symptoms of carcinoid syndrome in all patients; tolerability was good; no increase in the toxicity of immuno- and chemotherapy was observed [29].
History of evolution[edit]
Six somatostatin genes have been found in vertebrates. The currently proposed origin story for these six genes is based on three whole-genome duplication events that occurred in vertebrate evolution along with local duplications in teleost fishes. The ancestral somatostatin gene was duplicated during the first whole genome duplication event (1R) to create SS1
and
SS2
.
These two genes were duplicated during a second whole-genome duplication event (2R) to create four new somatostatin genes: SS1, SS2, SS3
and one gene that was lost during vertebrate evolution.
Tetrapods retained SS1
(also known as
SS-14
and
SS-28
) and
SS2
(also known as cortistatin) after splitting into the Sarcopterygii and Actinopterygii lineages.
In teleosts , SS1, SS2
and
SS3
were duplicated during the third whole genome duplication event (3R) to create
SS1, SS2, SS4, SS5
and two genes that were lost during the evolution of teleosts.
SS1
and
SS2
went through local duplication to give rise to
SS6
and
SS3
. [8]
Clinical observations
Long-acting octreotide relieves clinical manifestations in patients with NETs and has antitumor activity in patients with metastatic intestinal NETs, but it remains unclear whether it has antiproliferative effects in patients with advanced pancreatic NETs. H. Kitade et al. (2018) reported a 71-year-old man with multiple liver metastases from pancreatic NETs who was treated with everolimus 10 mg and sunitinib 25 mg daily for 3 weeks. However, therapy was discontinued due to disease progression and serious side effects. Extended-release octreotide was initially administered simultaneously with everolimus; the level of tumor markers decreased markedly, and liver metastases decreased in size. Immunohistochemical examination of tumor samples obtained before treatment showed a high level of expression of somatostatin receptor type 2. Clinical observation suggested that long-acting octreotide may be an option for the treatment of advanced pancreatic NETs after discontinuation of everolimus and sunitinib [30].
T. Arao et al. (2017) presented a 54-year-old woman hospitalized for treatment of acromegaly. Growth hormone (GH) levels were 39.8 ng/mL, insulin-like growth factor-1 (IGF-1) levels were 717 ng/mL, and GH levels were not suppressed (22.9 ng/mL) during an oral glucose tolerance test. MRI showed that the tumor, measuring 21x17 mm, extended into the right suprasellar region and invaded the cavernous sinus. Treatment with long-acting octreotide was started at a dose of 20 mg every 4 weeks. After three doses, GH and IGF-1 levels decreased to 2.19 ng/ml (to 1.69 after glucose tolerance test) and 205 ng/ml, respectively. A decrease in GH and IGF-1 levels, a decrease in tumor size and cavernous sinus invasion allowed surgical treatment to be performed without subsequent complications. Preoperative administration of long-acting octreotide improved outcomes in the treatment of acromegaly [31].
Pregnancy with acromegaly occurs rarely and proceeds favorably, but during this period an increase in tumor size may occur. Correcting tumor growth during pregnancy is difficult due to the potential complications of possible surgery and the side effects of anticancer drugs. AM Hannon et al. (2019) described a unique case of octreotide use in a 32-year-old woman with acromegaly diagnosed at 11 weeks. pregnancy. There was a large macroadenoma penetrating into the suprasellar cistern at 20 weeks. Bitemporal hemianopsia developed during pregnancy. The patient refused surgery and was prescribed treatment with octreotide 100 mcg 3 times a day subcutaneously, which led to normalization of visual fields after 2 weeks. therapy. Further decrease in visual fields at 24 weeks. pregnancy forced an increase in the dose of octreotide to 150 mcg 3 times a day; vision remained stable until the end of pregnancy. At 14 weeks. Gestational diabetes was diagnosed, and from the 22nd week. insulin was prescribed. There were no other obstetric complications, and fetal growth continued until the end of pregnancy. A planned caesarean section was performed at 34 weeks, fetal weight at birth was 3.2 kg, Apgar score 9, no congenital anomalies were detected. The menstrual cycle after childbirth is regular. The woman was prescribed extended-release octreotide at a dose of 40 mg and referred for surgery. 2 years after birth, the child was developing normally. The occurrence of acromegaly during pregnancy and the improvement of perimetry parameters with octreotide were first described [32].
Giant pituitary adenomas are benign tumors ≥4 cm in diameter. They present with symptoms due to hypersecretion of one or more pituitary hormones and involvement of surrounding structures in growth, and compression of the pituitary gland can lead to hypopituitarism. F. Dicuonzo et al. (2019) reported a young woman with acromegaly with an unresectable giant GH-secreting pituitary adenoma extending to the cavernous sinus, orbital cavity, maxillary sinus, sphenoid sinus, and right temporal fossa. Treatment with long-acting octreotide helped to quickly relieve headaches and bilateral hemianopia resulting from involvement of the optic chiasm, reduce the clinical manifestations of acromegaly and control tumor growth over time, enhance fertility, and allowed the patient to become pregnant. Therapy was discontinued during pregnancy. The patient gave birth to a healthy son. Tumor size did not increase at the end of pregnancy and during follow-up. This case confirms the possibility of a favorable pregnancy outcome in a patient suffering from acromegaly [33].
Ectopic adrenocorticotropic hormone (ACTH) syndrome is a rare disease often accompanied by severe hypercortisolism requiring surgical intervention. P. Rodrigues et al. (2012) described a 33-year-old patient hospitalized in 1993 with clinical manifestations of Cushing's syndrome. He had high plasma ACTH levels and dramatically increased urinary free cortisol excretion, which were not suppressed by high doses of dexamethasone. The pituitary gland appeared normal on MRI, but a chest CT scan revealed a 1.7 cm mass in the left lung. Instrumental studies showed the presence of ACTH-producing neuroendocrine carcinoma with distant metastases. The patient received chemotherapy plus octreotide, which resulted in a favorable clinical and biochemical outcome. The authors highlight the long-term response to drug therapy with octreotide with excellent antiproliferative effects [34].
A. Kanno et al. (2017) presented a case of insulinoma in an 80-year-old woman with episodes of hypoglycemia. The patient refused surgical treatment; subcutaneous administration of 50 mcg of octreotide at bedtime prevented hypoglycemia at night. The drug is capable of suppressing insulin secretion, although there is no specific protocol for its use in such cases. The patient was unable to administer the drug herself daily; she was prescribed long-acting octreotide, which prevented episodes of hypoglycemia for 4 weeks, and the patient’s quality of life improved significantly [35].
Links[edit]
- ^ abc GRCh38: Ensembl Issue 89: ENSG00000157005 - Ensembl May 2022
- ^ abc GRCm38: Ensembl release 89: ENSMUSG00000004366 - Ensembl, May 2022
- "Human PubMed Reference:". National Center for Biotechnology Information, US National Library of Medicine
. - "Mouse PubMed link:". National Center for Biotechnology Information, US National Library of Medicine
. - "somatostatin". Encyclopædia Britannica. Encyclopedia Britannica Online. Encyclopedia Britannica Inc., 2016. Online. 04 mag. 2016 < https://www.britannica.com/science/somatostatin >.
- ^ ab Costoff A. "Section 5, Chapter 4: Structure, synthesis and secretion of somatostatin". Endocrinology: endocrine pancreas
. Medical College of Georgia. paragraph 16. Archived from the original on April 5, 2008. Retrieved February 19, 2008. - "somatostatin preproprotein [Homo sapiens]". NCBI Reference Sequence
. National Center for Biotechnology Information (NCBI). - ^ abc Liu Y, Liu D, Zhang Y, Li S, Liu X, Lin X (September 2010). "Evolution of somatostatin in vertebrates". Gin
.
463
(1–2):21–8. DOI: 10.1016/j.gene.2010.04.016. PMID 20472043. - Gahete MD, Cordoba-Chacón J, Duran-Prado M, Malagon MM, Martinez-Fuentes AJ, Grazia-Navarro F, Luque RM, Castaño JP (July 2010). "Somatostatin and its receptors from fish to mammals". Annals of the New York Academy of Sciences
.
1200
: 43–52. DOI: 10.1111/j.1749-6632.2010.05511.x. PMID 20633132. S2CID 23346102. - "Entrez Gin: Somatostatin".
- ↑
Shen LP, Pictet RL, Rutter WJ (August 1982).
"Human somatostatin I: cDNA sequence". Proceedings of the National Academy of Sciences of the United States of America
.
79
(15):4575–9. DOI: 10.1073/pnas.79.15.4575. PMC 346717. PMID 6126875. - ↑
Shen LP, Rutter WJ (April 1984).
"Sequence of the human somatostatin I gene". The science
.
224
(4645): 168–71. DOI: 10.1126/science.6142531. PMID 6142531. - ^ abc Boron WF, Boulpaep EL (2012). Medical physiology
(2nd ed.). Philadelphia, PA: Elsevier. ISBN 9781437717532. - Minami, Shiro; Kamegai, June; Sugihara, Hitoshi; Suzuki, Nobuchika; Wakabayashi, Ichiji (1998). "Growth hormone inhibits its own secretion by acting on the hypothalamus through its receptors on neuropeptide Y neurons in the arcuate nucleus and somatostatin neurons in the periventricular nucleus". Endocrine Journal
.
45
. Retrieved January 10, 2022. - Stefanelli, Thomas; Bertollini, Christina; Luscher, Christian; Muller, Dominic; Mendez, Pablo (February 2016). "Hippocampal somatostatin interneurons control the size of neuronal memory ensembles". Neuron
.
89
(5). DOI: 10.1016/j.neuron.2016.01.024. PMID 26875623. Retrieved January 10, 2022. - Holst JJ, Skak-Nielsen T, Orskov S, Sayer-Poulsen S (August 1992). "Vagulatory control of somatostatin, vasoactive intestinal polypeptide, gastrin-releasing peptide, and HCl release from the nonantral pig stomach." Scandinavian Journal of Gastroenterology
.
27
(8): 677–85. DOI: 10.3109/00365529209000139. PMID 1359631. - ^ a b Bowen R (2002-12-14). "Somatostatin". Biomedical Hypertexts
. Colorado State University. Retrieved February 19, 2008. - First Aid for USMLE Step 1, 2010. Page 286.
- ^ ab Costoff A. "Section 5, Chapter 4: Structure, synthesis and secretion of somatostatin". Endocrinology: endocrine pancreas
. Medical College of Georgia. paragraph 17. Archived from the original on March 31, 2008. Retrieved February 19, 2008. - ↑
van der Meulen T, Donaldson CJ, Cáceres E, Hunter AE, Cowing-Zitron C, Pound LD, Adams MW, Zembrzycki A, Grove KL, Huising MO (July 2015).
"Urocortin3 mediates somatostatin-dependent negative feedback control of insulin secretion". Natural Medicine
.
21
(7): 769–76. DOI: 10.1038/nm.3872. PMC 4496282. PMID 26076035.