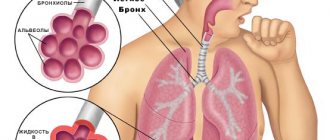
Obstructive bronchitis is an inflammation of the bronchi, which is accompanied by a narrowing of their lumen due to swelling or spasm, as well as the accumulation of thick mucus, which leads to impaired ventilation. The disease manifests itself as a wet cough, shortness of breath, and wheezing. Unlike other forms of bronchitis, the treatment regimen in this case is broader: antispasmodic therapy, hormonal drugs and more are often included.
Acute obstructive bronchitis often develops in young children, while adults are more susceptible to chronic disease. In the second case, concomitant disorders are often observed, that is, we are talking about chronic obstructive pulmonary disease.
Mechanism of development and causes of obstructive bronchitis
Acute obstructive bronchitis is most often associated with respiratory syncytial viruses, influenza, parainfluenza viruses, adenoviruses, and rhinoviruses. Young children are more susceptible to the disease, especially those who often suffer from acute respiratory viral infections, have weakened defenses, and allergic reactions.
Chronic obstructive bronchitis develops against the background of factors such as:
- smoking, including passive smoking (inhalation of tobacco smoke);
- harmful working conditions: contact with chemicals, polluted air at work;
- allergic reactions, etc.
It is worth noting that men are more likely to get sick. Other risk factors include working in the agricultural and metallurgical industries, on the railroad, and even in the office if the activity involves printing on laser printers.
The disease begins with inflammation of the small and medium bronchi, as well as surrounding tissue. As a result, the movement of the cilia of the bronchial epithelium is disrupted, the mucous membranes change, some cells are replaced by others. The secretion also transforms - it stagnates, clogging the small bronchi, which causes a violation of pulmonary ventilation.
The content of local immunity factors - interferon, lysozyme, lactoferrin - decreases in sputum. Thick mucus loses its bactericidal properties and becomes an optimal environment for bacteria to multiply.
Bronchospastic reactions develop, the altered mucous membranes swell, there is more mucus, and a spasm of smooth muscles occurs. What distinguishes bronchitis from obstructive bronchitis is that in the first case the patency of the bronchi is not impaired, but there is only an inflammatory component of the disease.
(ICD-10: E10-E14) Hypoglycemic state
A hypoglycemic state is a condition characterized by an acute energy deficiency in the neurons of the brain as a result of a decrease in blood sugar due to an overdose of insulin, hypoglycemic drugs, salicylates, alcohol, or insufficient dietary carbohydrate intake.
Clinical signs:
| Urgent Care:
|
Symptoms of obstructive bronchitis
In obstructive bronchitis, acute symptoms manifest themselves in the form of obstruction itself and infectious toxicosis. The main manifestations include the following:
- fever - increased body temperature to 338-39 °C;
- headache;
- disruption of digestive processes;
- weakness;
- respiratory disorders - dry or productive obsessive cough, worse at night;
- dyspnea;
- flaring of the wings of the nose when inhaling;
- participation in breathing of the muscles of the neck, shoulder girdle, and abs;
- retraction of intercostal spaces during inspiration;
- prolonged whistling exhalation;
- audible wheezing.
Symptoms can last from 7 to 21 days, depending on the general condition and individual characteristics of the patient’s body. If we are talking about recurrent obstructive bronchitis (3 episodes per year or more), the risk of developing a chronic form increases. The latter involves the persistence of symptoms for 2 or more years.
Symptoms of chronic obstructive bronchitis consist mainly of cough and shortness of breath. After a coughing attack, as a rule, a little mucous sputum is released. During exacerbations, the amount of sputum increases, it becomes mucopurulent. The cough may be constant and accompanied by characteristic wheezing. If there is a complication in the form of arterial hypertension, it is not uncommon to see blood in the sputum.
Difficulty in exhalation is not immediately observed, but sometimes the disease begins with this type of shortness of breath. Shortness of breath can be of varying intensity: some describe the condition as a feeling of lack of air during physical activity, others note a severe lack of oxygen even at rest. The degree of shortness of breath is determined by the severity of the disease and concomitant ailments.
An exacerbation can be provoked by acute respiratory viral infections, high workload, arrhythmia, the use of certain medications and other reasons. At the same time, shortness of breath and sweating increase, loss of strength, muscle pain, etc. appear.
In severe cases, additional muscles may be involved in the act of breathing, wheezing, swelling of the neck veins, changes in the shape of the nails and bluish skin are observed.
(ICD-10: J44.1) Broncho-obstructive syndrome
Broncho-obstructive syndrome is a violation of the ventilation ability of the lungs, which is based on impaired bronchial obstruction and is a complication of chronic obstructive pulmonary disease and a number of other conditions.
Clinical signs:
| Urgent Care:
|
Tactics
- Relief of shortness of breath.
- An asset to the doctor of the clinic.
- If there is no effect - hospitalization
Symptoms by stage
The severity of chronic obstructive bronchitis is assessed by such an indicator as forced expiratory volume in 1 second, or FEV1:
- Stage 1: FEV1 exceeds 50% of normal. A person’s quality of life suffers slightly; constant medical monitoring is not needed.
- Stage 2: FEV1 is 35–49% of normal. There are negative changes in the patient’s quality of life, and there is a need for observation by a pulmonologist.
- Stage 3: FEV1 is less than 35% of normal. Exercise tolerance is sharply reduced; inpatient treatment and outpatient observation in the pulmonology department/office are required.
Complications of the disease include emphysema, so-called cor pulmonale, respiratory failure, etc.
(ICD-10: J46) Status asthmaticus
Status asthmaticus (status asthmaticus) is a severe life-threatening complication of bronchial asthma; occurs as a result of a prolonged intractable attack and is characterized by swelling of the bronchioles, accumulation of viscous sputum in them, increasing suffocation and hypoxia.
Clinical signs:
| Urgent Care:
If there is a threat of respiratory arrest:
|
Tactics
- Stopping an attack, reducing shortness of breath.
- Restoring breathing.
- Hospitalization in the intensive care unit.
Diagnosis of obstructive bronchitis
Treatment of obstructive bronchitis in adults is preceded by a comprehensive diagnosis. The scope of necessary research is determined by the expected form and stage of the disease.
The doctor will conduct an examination, listen to the lungs, evaluate the tone and wheezing after coughing, etc. He will also direct you to a number of studies, including:
- X-ray: necessary to exclude lung lesions and detect concomitant diseases.
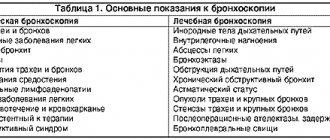
- Bronchoscopy: involves examining the bronchial mucosa. It is possible to simultaneously perform mucus collection for further bacteriological examination and a therapeutic procedure such as lavage.
- Bronchography: This x-ray examination involves the insertion of an endoscope and is performed under local or general anesthesia.
- Pulmonary function tests: spirometry, peak flowmetry, pneumotachymetry. Based on the data obtained, the doctor will assess the degree and reversibility of obstruction, impaired ventilation, and the stage of bronchitis.
- Laboratory tests: general and biochemical blood tests, general urine analysis, bacteriological and microscopic examination of sputum, immunological tests.
- Determination of blood gas composition, etc.
The data obtained will allow the doctor to prescribe a treatment regimen.
(ICD-10: J45) Bronchial asthma, attack (moderate severity)
Bronchial asthma, attack (moderate severity) is a complication of bronchial asthma of moderate severity, characterized by repeated attacks of shortness of breath or suffocation with difficulty exhaling due to impaired bronchial obstruction.
Clinical signs:
| Urgent Care:
|
Tactics
- Stopping an attack.
- An asset to the doctor of the clinic.
- If there is no effect - hospitalization
Treatment of the disease
The main principles of treatment of obstructive bronchitis in adults are maintaining rest, drinking plenty of warm drinks, maintaining optimal air humidity in the room, alkaline and medicinal inhalations.
The following types of drugs are used in therapy:
- antibacterial (if there is evidence indicating the addition of a bacterial infection), rarely and according to indications - antifungal drugs;
- bronchodilators for severe narrowing of the bronchial lumen;
- mucolytics - agents that thin mucus and promote its removal;
Treatment
Therapy depends on the form of the disease. In the acute form, full-scale drug therapy is always necessary. Its purpose is:
- relieving bronchospasm,
- suppression of viral activity,
- relief of mucus discharge,
- restoration of respiratory function,
- relaxation of the pectoral muscles.
First of all, the doctor selects effective antiviral medications for the patient and advises them to drink as much fluid as possible per day. The following drink is recommended :
- decoctions of dried fruits
— fruit drinks and berry compotes
- fresh juices (freshly squeezed juices), but not from citrus fruits
– alkaline mineral water
- weak and medium brewed tea
It is better to exclude chocolate and dishes containing it, honey, spices, and citrus fruits from the diet (only tea with lemon is acceptable). These products are highly allergenic and can lead to bronchospasm.
A special massage is required, which helps to liquefy sputum (percussion massage) and relax the muscles of the chest. To relieve bronchial spasm, drugs from the group of antispasmodics are used. The most effective is the well-known no-spa.
Drugs that relieve shortness of breath - bronchodilators (Asthmopent, Berotec) - are also used in the treatment of obstructive bronchitis in adults. Astmopent is available in the form of an aerosol for inhalation. For adults, a single dose is 1-2 doses. The interval between doses should be at least 20 minutes. The next time the drug is used is after 4 hours. The maximum daily number of inhalations is 12 doses. As for the side effects of Asthmopent, there may be fatigue and anxiety. Rarely there are symptoms from the gastrointestinal tract: nausea and vomiting, unpleasant taste in the mouth. The following side effects are also likely:
- dizziness
- headache
- increase in blood pressure
- hyperhidrosis
- tachycardia
- tremors and muscle contractions
- various heart rhythm disturbances
- hypokalemia, etc.
If a person is hypersensitive to the components of the drug, allergic reactions may occur. The drug should not be prescribed if the patient has tachycardia and other arrhythmias, and it is not suitable for breastfeeding mothers. An overdose of Astmopent can cause:
- dry mouth
- nausea
- headache
- anxiety
- difficulty falling asleep
- decreased or increased blood pressure
- tachycardia, etc.
Astmopent is prescribed with caution for coronary heart disease, hyperthyroidism, arterial hypertension, epilepsy and uncontrolled diabetes.
Berotec, which is used, as already noted, for the treatment of obstructive bronchitis in adults, can cause the following side effects:
- nausea and vomiting
- feeling of heartbeat
- tachycardia
- decrease in diastolic blood pressure
- increased systolic blood pressure
- heart rhythm disturbances
- angina attacks
- dizziness and headache
- increased excitability
- nervousness
- convulsions
- development of mental changes (very rare, mainly during long courses)
- local irritation of mucous membranes
- cough
- hives/itching
- Quincke's edema
- myalgia
- severe hypokalemia
Contraindications for taking Berotek:
- hypertrophic obstructive cardiomyopathy
- individual sensitivity to constituent substances
- tachyarrhythmia
- first trimester of pregnancy
- lactation
Medicines such as mucolytics relieve coughs, among which lazolvan is very effective. You need to not only take medications, but also do breathing exercises. If a microbial process has joined the pathological process, only then can the doctor prescribe antibiotics.
Obstructive chronic bronchitis also requires symptomatic therapy: treatment aimed not at eliminating the cause, but at relieving symptoms. The goal is to reduce the number and duration of exacerbations and slow down the pathological process. It is important to quit smoking during this period if the sick person has such a habit. You need to change your profession or place of work if the cause of bronchitis lies precisely in your stay in hazardous industries. Also, if possible, improve living conditions if they are unsatisfactory.
The doctor prescribes bronchodilators, bronchodilators, xanthine drugs (theophylline, etc.), mucolytics. If there is no effect, resort to treatment with corticosteroids.
Walks in the fresh air are important, at least 1-1.5 hours. If there is a coniferous forest nearby, it is better to walk there. In this case, you need to dress according to the weather, so that another respiratory tract disease does not join the disease.
Emergency hospitalization is necessary for:
- severe symptoms of intoxication of the body, weakness and lethargy
- very high temperature
- lack of appetite for a long time
- nausea