Bronchiectasis is an expansion of a separate section of the bronchi with changes in structure and function. Bronchiectasis is not an independent disease, but occurs as a result of many other diseases and conditions.
Bronchiectasis increases the patient's susceptibility to respiratory tract infections, which leads to frequent exacerbations and progression of the disease. Thus, bronchiectasis is a chronic progressive bronchopulmonary disease that requires constant medical supervision and supportive treatment, the volume of which increases with exacerbations.
Symptoms of bronchiectasis
Symptoms of bronchiectasis vary: from repeated episodes of respiratory tract infections, between which all symptoms of the disease completely disappear, to daily cough with sputum, the nature of which can vary from mucous (colorless) to mucopurulent (light yellow) and purulent (dark yellow, green or grey-green). Patients with bronchiectasis are characterized by a large volume of sputum - up to 100-200 ml per day, but sometimes the sputum is more scanty. From time to time, bloody streaks or clots may appear in the sputum, which is associated with trauma to the thinned bronchial wall during a hacking cough.
In rare cases, bronchiectasis is complicated by severe pulmonary hemorrhage requiring surgical intervention. When inflammation passes from the bronchial wall to the lung tissue, pneumonia can develop, and to the pleura - pain in the chest when breathing and coughing. In later stages of the disease, respiratory failure may develop.
Exacerbations of the inflammatory process in bronchiectasis are often accompanied by weakness, prolonged episodes of temperature (usually no higher than 37.2-37.50C), and weight loss.
4.Treatment
The therapeutic strategy for bronchiectasis is determined by its stage and clinical severity.
The most universal means are mucolytics and antibiotics, postural drainage, physiotherapeutic methods (special massage, breathing exercises, etc. are effective). In more severe cases, immunomodulators and immunostimulants, oxygen therapy, and sanitizing bronchoscopy are prescribed; As a last resort, life-saving measure, they resort to surgery to restore airway patency.
Diagnosis of bronchiectasis
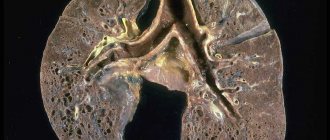
Bronchiectasis is detected by high-resolution computed tomography (CT) of the lungs. Conventional radiography, and especially fluorography, are not sensitive enough to diagnose this disease. According to CT scans of the lungs, it is sometimes possible to determine the cause - in congenital malformations of the lungs, tracheobronchomegaly, emphysema, tuberculosis, etc.
As a rule, to establish the cause, additional studies are required, the range of which can be quite wide, determined by the doctor during a conversation with the patient (collection of complaints and anamnesis), as well as based on the results of a CT scan of the lungs. Thus, if genetic diseases are suspected, a genetic analysis is carried out; if a fungal infection of the lungs is suspected, immunological studies (determination of antibodies to fungi) and special sputum cultures for fungal flora are performed.
What other studies are used in diagnosis?
Mandatory studies in patients with bronchiectasis are bacteriological analysis of sputum and a study of respiratory function (spirography, respiratory function or body plethysmography).
Bacteriological analysis of sputum (sputum culture)
Bronchiectasis creates ideal conditions for the colonization of various microorganisms - the constant presence of bacteria on the surface of the bronchial mucosa in bronchiectasis. Long-term colonization of bacteria can cause inflammation even in the absence of other provoking factors (hypothermia, ARVI, etc.). This inflammation is manifested by frequent or persistent bronchitis with fever, weakness, sweating, and weight loss.
If the bacteria are not or cannot be removed from the bronchial tree, the inflammation becomes chronic with constant production of purulent sputum and lung damage. That is why it is important to regularly conduct bacteriological examination of sputum in order to control the composition and number of microorganisms present in the bronchi.
Pulmonary function test (PRF)
With chronic inflammation, the lumen of the bronchi narrows due to swelling of the bronchial mucosa, accumulation of mucus in the lumen of the bronchi, and sometimes bronchospasm (contraction of the muscles of the bronchial wall) can develop.
All these processes narrow the lumen of the bronchi and can cause shortness of breath. To diagnose these conditions, various methods of studying the function of external respiration are used. The simplest and most accessible method is spirometry, but more complex research methods are often required - measuring lung volumes (body plethysmography) and assessing the diffusion capacity of the lungs (the ability to pass oxygen from inhaled air into the blood). The results of these studies are important for prescribing treatment for a patient with bronchiectasis.
1.General information
Bronchiectasis, or bronchiectasis, is a serious, dangerous disease of the respiratory system. It consists of irreversible deformation (expansion) of the airways, the bronchi, most often in the lower parts of the bronchial tree, which is accompanied by a chronic purulent-inflammatory process and functional failure, expressed to one degree or another.
Bronchiectasis is by no means a sporadic rarity; it is detected with a frequency of about 1% in the general population (more often in children, up to 65% are boys). However, with regard to this disease, many etiopathogenetic, therapeutic, diagnostic and even classification issues remain unresolved today.
Thus, the debate is still ongoing about whether bronchiectasis should be considered an independent disease or a type of chronic pneumonia; whether this pathology is primary, or whether it is a secondary syndrome acquired as part of other diseases or under the influence of various causes. One way or another, the problem remains acute and relevant; it is being intensively studied by world pulmonology both in theoretical and in purely practical, therapeutic and diagnostic aspects.
A must read! Help with hospitalization and treatment!
Is it possible to cure the disease?
Bronchiectasis is a chronic progressive disease in which the quality of life of patients depends on the extent of lung damage, the degree of impairment of pulmonary function, the severity and frequency of exacerbations. There is no cure for this disease. But we are able to influence the rate at which the disease worsens. The rate of progression is largely determined by the nature of the chronic bronchial infection.
Thus, it is possible to slow down the progression of the disease and improve the patient’s quality of life with early diagnosis, identification and treatment of their cause, adequate treatment of chronic bronchial infections, prevention of exacerbations and regular medical supervision of the patient.
Are there surveillance programs for patients with bronchiectasis? Yes, they exist. Follow-up examinations with a doctor should be scheduled every 1 to 6 months, depending on the severity of the disease. Even if the patient’s condition is stable (in the remission phase), a general sputum analysis and bacteriological examination of sputum should be performed to assess the activity of inflammation in the bronchi. During the examination, the doctor should assess the severity of shortness of breath, the presence or absence of hemoptysis, general symptoms of inflammation (weakness, sweating, weight loss, temperature), listen to the lungs and, in case of severe impairment of pulmonary function, conduct a stress test (6-minute walk test).
Annual examination of a patient with bronchiectasis should include spirometry with a bronchodilator to assess the rate of decline in pulmonary function, a complete blood count with C-reactive protein (CRP) and immunoglobulin (Ig) A to assess the overall inflammatory response of the body.
At each visit to the doctor, it is advisable to measure saturation (oxygen saturation in the blood) using a pulse oximeter. If saturation decreases below 93%, it is recommended to perform a complete study of the gas composition of arterial blood to decide on the prescription of oxygen therapy.
For patients at high risk of disease progression, it is recommended to repeat CT scans of the lungs routinely once every 2 years. In addition, an X-ray of the lungs is performed annually, as well as if severe or life-threatening complications (pneumonia, pneumothorax) are suspected.
Pulmonary rehabilitation for bronchiectasis
Our pulmonology department has developed a “Pulmonary Rehabilitation Program for Patients with Bronchiectasis.”
A course of complex therapy can replace bronchoscopic sanitation in patients with bronchiectasis.
- sputum becomes easily coughed up, coughing occurs naturally, medications are poured into the smallest bronchi, including antimicrobial agents.
- the introduction of drugs into the bronchus and removal of sputum is not invasive and traumatic.
- Due to the positive effect of drainage techniques and special exercises included in the course, lymphatic drainage of the bronchi and their blood supply improve. As a result, the protective properties of the mucous membrane of damaged bronchi and surrounding lung tissue are enhanced.
- There are no risks inherent in bronchoscopy: the risk of bleeding, damage and allergic reaction to anesthesia.
Bronchiectasis. Complications
The altered walls of the bronchi, which have lost their elasticity and strength, and have lost their natural defense mechanisms, are suitable soil for the rooting and growth of pathogens (both those present in the body and those coming from outside). As a result of repeated inflammations and subsequent destruction of bronchial tissue, the situation worsens and can lead to:
- bleeding;
- recurring bronchitis and pneumonia;
- emphysema;
- secondary amyloidosis.
And ultimately - to the progression of heart and pulmonary failure.
Treatment of bronchiectasis
Treatment of a patient with bronchiectasis is aimed at improving the condition, preventing exacerbations, and, consequently, progression of the disease.
If the cause of bronchiectasis is known, then treatment should be aimed at eliminating it.
The main components of success in treatment:
- adequate antibiotic therapy;
- powerful mucolytic (sputum thinning) therapy;
- bronchodilators;
- breathing exercises, breathing simulators;
- complete nutrition.
In some cases, mainly with a limited prevalence of bronchiectasis, surgical treatment (removal of the affected area of the lung) is possible in a thoracic department or surgical hospital. For this, a consultation with a thoracic surgeon will be necessary.
All patients with bronchiectasis should receive an influenza vaccine annually in the fall, and once every 5 years - the Pneumo-23 anti-pneumococcal vaccine. Of course, vaccination, like any method of treatment, has its contraindications, but modern vaccines reduce them to a minimum and make it possible to safely vaccinate the vast majority of patients, including patients with bronchial asthma and other allergic diseases.
Our specialists
Chikina Svetlana Yurievna
Candidate of Medical Sciences, pulmonologist of the highest category. Official doctor, expert at Russian congresses on pulmonology.
30 years of experience
Kuleshov Andrey Vladimirovich
Chief physician, candidate of medical sciences, pulmonologist, somnologist, member of the European Respiratory Society (ERS).
Experience 26 years
Meshcheryakova Natalya Nikolaevna
Candidate of Medical Sciences, pulmonologist of the highest category, associate professor of the Department of Pulmonology named after. N.I. Pirogov.
Experience 26 years
Nikitina Natalia Vladimirovna
Deputy chief physician, pulmonologist, allergist of the highest category. Full member of the European Academy of Allergy and Immunology.
Experience 15 years