Pneumonia and pneumonia
What is pneumonia? Difference between pneumonia and pneumonia. Symptoms of pneumonia with coronavirus How long does the temperature last for pneumonia Types of pneumonia Pneumonia without fever Polysegmental pneumonia Focal pneumonia Atypical pneumonia Community-acquired pneumonia Viral pneumonia Lobar pneumonia Pneumonia without cough Interstitial pneumonia Pneumocystis pneumonia Mycoplasma pneumonia Is pneumonia contagious in children Treatment of pneumonia How many days is pneumonia treated Double pneumonia in adult. Duration of treatment Clinical recommendations Treatment of pneumonia at home Treatment with folk remedies Drugs for the treatment of pneumonia Antibiotics for pneumonia Breathing exercises For the prevention of pneumonia For rehabilitation after pneumonia
What is pneumonia? Difference between pneumonia and pneumonia.
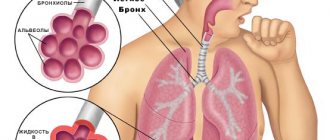
Pneumonia or pneumonia is a group of diseases in which inflammatory processes develop in the lungs. There is no difference between pneumonia and pneumonia
. These processes most often become the result of infections, viruses, microbes, and pneumonia is often infectious in nature. Irritants affect the lung tissue, and an inflammatory process develops, requiring intensive treatment.
Pneumonia can result from:
- untreated colds, ARVI, flu or bronchitis;
- exposure to viruses, bacteria and fungi, for example, chlamydia, legionella, mycoplasma;
- uncomfortable temperature (lung hypothermia);
- exposure to toxic airborne particles or radiation;
- complications after an allergic cough.
Symptoms of pneumonia
- temperature increase;
- shortness of breath and cough;
- chills, fever;
- weakness, headache;
- difficult breathing, chest pain when taking a deep breath;
- sweating;
- signs of intoxication.
An elevated temperature of up to 38-39 degrees is one of the main signs of pneumonia. It is accompanied by severe chills and can rise and fall during the day within 1-1.5 degrees. Fever can last up to 10 days.
In many ways, severe weakness, increased sweating, headache, abnormal bowel movements and abdominal pain with pneumonia are associated with intoxication of the body, its poisoning with tissue breakdown products and toxins.
Today, much attention is paid to the psychosomatics of pneumonia. Long-term stress that weakens the body, chronic diseases and serious overload of an unprepared body can become the basis for the development of pulmonary diseases and lead to inflammation of the lower respiratory tract.
In this case, conventional antibiotic therapy may become ineffective; a long recovery period is required, aimed at normalizing the functions of the nervous system and restoring the body’s strength.
Symptoms of pneumonia due to coronavirus
Pneumonia can be caused by a number of viruses, the main ones of which are adenoviruses, influenza viruses and coronaviruses (including the dangerous SARS-CoV-1, MERS-CoV and the SARS-CoV-2 that brought the pandemic).
If coronavirus causes pneumonia, usually this process is “triggered” by the usual symptoms of a cold: a temperature of 37.5-38 degrees, sore throat, loss of smell, cough, weakness and muscle pain. As a rule, these symptoms last about 7 days. After this, the temperature rises to 40 degrees, intoxication rapidly increases, shortness of breath and chest pain appear. Fever, chills, excessive sweating and severe weakness are also symptoms of the development of coronavirus infection into pneumonia.
Cough - dry, or with unexpressed sputum, sometimes it can be rusty in color due to the destruction of capillaries.
One of the distinctive symptoms of pneumonia due to coronavirus is limited breathing; in severe cases, it is almost impossible to breathe independently. With uncomplicated pneumonia, severe shortness of breath is observed when several pulmonary lobes are affected and is not manifested at rest. Pneumonia caused by coronavirus is characterized by a respiratory rate of more than 22, the patient constantly experiences a feeling of lack of air and the inability to take a full breath.
Respiratory failure leads to cyanosis of the nasolabial triangle; patients experience forced breathing, in which the intercostal muscles actively participate. Patients tend to take unusual positions to make breathing easier. Due to a lack of oxygen supply to the brain, patients may experience confusion, panic attacks, or fainting.
How long does the temperature last for pneumonia?
There are two types of temperature for pneumonia - low-grade and high.
With pneumonia, the temperature can rise sharply to 39-40 degrees and can last for two weeks. It is important to remember that it is important to lower the temperature under the supervision of a doctor and in full compliance with the individual protocol of antibacterial therapy. Although a high fever is a common symptom of pneumonia, lowering it is part of the overall treatment.
When body temperature reaches 40 degrees, you need to call an ambulance
. Such an increase in temperature may indicate that the body’s immunity cannot cope with the infection and it needs emergency help.
Low-grade fever for pneumonia is in the range of 37-38 degrees. In the absence of severe shortness of breath, reducing such a temperature is usually not recommended. It provides the body with the ability to mount an immune response to a viral attack. An increase in temperature signals a lack of the body's own resources to suppress the viral infection.
The temperature returns to normal when a viral infection of the body is reflected after antibiotic therapy.
How to recognize the very first signs of incipient pneumonia?
At an early stage of the disease, symptoms may vary in intensity. What matters is a person’s age, the state of his immune system, and the characteristics of the body as a whole. Pneumonia can manifest itself acutely, and the patient’s well-being sharply deteriorates. In other clinical cases, the disease develops slowly, over several days or even weeks.
The first symptoms to suspect pneumonia:
- Cough that persists for several days or weeks. Over time, it does not stop, but gains strength. Cough can be different: with or without phlegm, frequent and rare.
- Hyperthermic reaction. A fever with an increase in body temperature to 39-40 degrees is not excluded. In other cases, it remains at the level of low-grade fever (37 - 37.5 degrees).
- Shortness of breath, feeling of lack of air.
- Increased fatigue.
- Hoarseness.
- Rhinitis, pain and sore throat.
- Confusion.
- Reluctance to eat, nausea, loose stool.
It may take 2 to 4 days from the moment of infection until the first symptoms appear. When the incubation period is over, the first signs of the disease will appear. To prevent its progression, you must immediately contact a specialist.
Allergist-immunologist Ilyintseva N.V. at Allegris MC: cough or pneumonia?
Types of pneumonia
Pneumonia without fever
Quite a dangerous type - asymptomatic pneumonia
, not manifested by elevated temperature. There may be no symptoms other than weakness. The body may not signal a disease even by coughing. Often this situation is a consequence of a weak immune response and the body’s inability to fight the virus.
Doctors advise paying attention to a person’s complexion; often a characteristic spotted blush appears on the background of very pale skin. Human breathing occurs with a whistle. When moving, shortness of breath and rapid pulse appear. The body is weak, gets tired quickly, chest pain and difficulty breathing are possible.
Asymptomatic pneumonia is dangerous because there is no cough and excess sputum does not come out. The infectious process stagnates in the lungs. Often this is a consequence of untreated colds or bronchitis.
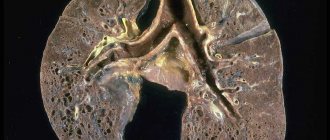
For diagnosis, a chest x-ray is taken in 2 projections. The main sign of pneumonia is limited darkening of the lung tissue.
Polysegmental pneumonia
Bilateral polysegmental pneumonia affects several segments of the tissue of both lungs. It often affects children under one year of age and people with reduced immunity. The first stage of the disease may be asymptomatic or similar to ARVI
.
The development of symptoms of bilateral pneumonia - cough with sputum, shortness of breath, moist rales in the lungs, chest pain. This clinical picture is accompanied by an increase in temperature to 39-40 degrees, fever, increased sweating, tachycardia, headaches and changes in consciousness. With polysegmental pneumonia, sputum stagnates in the bronchi, which is difficult to drain due to progressive edema.
Focal pneumonia
An acute form of the disease with an inflammatory process occurring in a limited area of lung tissue (lung lobe). Symptoms of this form of pneumonia are fever, dry cough or slight sputum production, chest pain, and general weakness.
Often focal pneumonia is a complication of acute respiratory infections and bronchitis. This diagnosis increases during seasonal ARVI and influenza.
Body temperature rises to 38-39 degrees, sometimes it can be normal or have subfebrile values. Breathing quickens to 25-30 units, tachycardia manifests itself up to 110 beats. per minute
Fever usually stops 3-5 days after the start of antibiotic therapy. The period for relieving symptoms of focal pneumonia is 3-4 weeks.
Atypical pneumonia
Atypical pneumonia is an infectious disease accompanied by inflammation. This lung damage is caused by uncharacteristic pathogens - viruses, mycoplasmas, chlamydia and other numerous infectious agents.
This type of disease differs from “typical” pneumonia caused by bacterial coccal flora. Symptoms of atypical pneumonia:
- weakness,
- headaches and muscle pain,
- dyspnea,
- sweating,
- fever,
- cough.
To diagnose atypical pneumonia, it is necessary to determine the causative agent, for which PCR, RIF, and culture methods are used. An X-ray of the lungs is necessary. After identifying the pathogen, drug treatment is prescribed.
Atypical pneumonia caused by coronavirus is called acute respiratory syndrome (SARS). It is difficult to identify the infectious agent, and therefore to treat, due to the rapid mutation of the virus.
SARS infection occurs through airborne droplets. The incubation period is from 3 to 10 days. Depending on the pathogen, atypical pneumonia is divided into:
- Q fever,
- chlamydial pneumonia,
- legionella pneumonia,
- severe acute respiratory syndrome,
- mycoplasma pneumonia, etc.
Among the drugs recommended for the treatment of atypical pneumonia, the main one is ribavirin, which is now widely used to treat pneumonia caused by coronavirus. After the start of treatment, corticosteroids are introduced into the protocol; in severe cases, blood plasma transfusion is used. Treatment includes oxygen therapy, diuretics to prevent pulmonary edema, infusion therapy to relieve intoxication, symptomatic treatment for cough and symptoms of respiratory syndrome.
Community-acquired pneumonia
Community-acquired pneumonia is not associated with the patient's hospital stay. This diagnosis is made when the patient was not hospitalized or contracted pneumonia no less than 14 days after discharge or no later than two days after hospitalization.
Community-acquired pneumonia develops due to the impact of pathogenic microorganisms on the respiratory tract. This occurs when the patient has a complicated history of cardiovascular or metabolic diseases, an unhealthy lifestyle, weak immunity, advanced age, or severe hypothermia.
Pneumococci, streptococci, Haemophilus influenzae, staphylococci, chlamydia, legionella, and adenoviruses enter the human body at home, in crowded places through airborne droplets, entering the air when coughing and sneezing from the patient’s respiratory tract.
With reduced immunity and other unfavorable factors, the drainage system of the lungs is disrupted, and pathogenic microorganisms remain in them, causing an inflammatory process.
For the treatment of community-acquired pneumonia, drug therapy is used according to a protocol associated with the pathogen identified by bacteriological analysis.
Viral pneumonia
Viral pneumonia is caused by respiratory viruses, often familiar to us. These are influenza viruses, parainfluenza, enteroviruses, adenoviruses. Therapy for viral pneumonia is the use of antiviral and symptomatic drugs.
Symptoms of viral pneumonia are acute:
- a sharp increase in temperature,
- intoxication syndrome,
- severe productive wet cough,
- pain in the lungs.
Diagnosis of viral pneumonia is based on laboratory data.
Often viral pneumonia develops against the background of acute respiratory viral infection, in which case the typical symptoms of a respiratory disease are aggravated for several days by high fever, cyanosis, cough with rusty-colored sputum, wheezing in the lungs and chest pain.
Viral pneumonia caused by the influenza virus is often bilateral, with focal lesions in the lungs. Moreover, among viral pneumonia there are often cases of a relatively mild form of the disease with moderate symptoms and rapid recovery.
In childhood, viral pneumonia accounts for 90% of all types of this disease. In severe cases, viral pneumonia is severe in children:
- with high temperature
- vomiting,
- intense symptoms of intoxication,
- lack of appetite or complete refusal to eat,
- severe cough.
In severe cases, hospital treatment is prescribed.
Adults suffer from viral pneumonia less often than children (the percentage of viral pneumonia among other types of disease does not exceed 35%). Viral pneumonia most often affects people over 65 years of age. The incidence of the disease increases in the autumn-winter period.
Lobar pneumonia
Lobar pneumonia is an acute infectious disease. This diagnosis is made when one or more lobes of the lung are affected when fibrinous effusion and fibrinous deposits on the pleura appear in the alveoli.
The most common causative agent of lobar pneumonia is pneumococcus, and the main cause of the disease is decreased immunity.
The disease begins acutely, with an increase in temperature to 39 degrees, chills, and chest pain. A dry cough is replaced by the production of “rusty” sputum. Shortness of breath is pronounced. Breathing is harsh, with wet and dry wheezing. Subsequently, vocal tremors are detected due to impaired breathing. Lobar pneumonia can be accompanied by irregular heart rhythms, a drop in blood pressure and severe headaches.
At the end of the acute phase of the disease, breathing returns to normal, although a rapid pulse and decreased blood pressure may still bother the patient.
Croupous pneumonia is a disease of adults, and it is treated in a hospital in the therapy department.
Pneumonia without cough
Pneumonia is most often accompanied by a characteristic set of symptoms, but it happens that the disease occurs in a latent form. Asymptomatic pneumonia is difficult to diagnose, since the patient cannot recognize the health problem based on obvious signs. Latent pneumonia can occur without fever and even without wheezing in the lungs.
Most often, people over 60 years of age suffer from latent pneumonia.
Immune system dysfunction is the main cause of asymptomatic pneumonia. It can also develop due to improper use of cough medications during a respiratory illness. If sputum is poorly excreted, it accumulates in the lungs and becomes a breeding ground for pathogenic flora.
A complication after influenza, bronchitis or ARVI is another cause of asymptomatic pneumonia.
If there is no cough, but there is a suspicion of illness, you need to listen to the following symptoms:
- increased weakness,
- decreased performance,
- severe headaches.
The patient exhibited severe sweating, rapid pulse, shortness of breath and chest pain. The temperature may rise.
To detect pneumonia with hidden symptoms, it is necessary to carry out in-depth diagnostics, which will help determine the stage and severity of the disease.
Interstitial pneumonia
Interstitial pneumonia is an inflammatory process in which the walls of the alveoli and the connective tissue of the parenchyma are affected. The disease is caused by infectious agents:
- mycoplasma,
- chlamydia,
- pneumocystis,
- legionella,
- respiratory viruses,
- herpes virus.
Interstitial pneumonia can also be a reaction to dust. Interstitial pneumonia is focal or diffuse and may involve a lobe or the entire lung.
Symptoms of the disease:
- dyspnea,
- dry cough,
- chest pain,
- temperature up to 38 degrees,
- cardiopulmonary failure.
The disease is determined using CT and laboratory diagnostics.
The disease can be severe, with a high probability of pulmonary fibrosis. At risk:
- smokers,
- HIV-infected,
- people with alcoholism.
Interstitial pneumonia can occur in a chronic form (more than 12 months), during which time the patient is limited in activity, suffers from severe shortness of breath and high fatigue. Severe weight loss is common.
Treatment includes oxygen therapy, corticosteroids, and cytostatics. Due to decreased respiratory function, mechanical ventilation is prescribed.
Pneumocystis pneumonia
Pneumocystis pneumonia is a type of atypical pneumonia. Its infectious agents are the protozoan microorganisms Pneumocystis. The disease is transmitted by airborne droplets and often develops in people with a compromised immune system.
At risk for PCP:
- aged people,
- HIV patients,
- tuberculosis,
- patients with blood diseases,
- patients taking immunosuppressants.
The disease may have relapses. In particular, in patients with HIV infection in the AIDS stage, the probability of recurrent disease is 25%.
Pneumocystis enter the body through the respiratory tract, actively multiply, and provoke the appearance of large amounts of mucus and metabolic products. Once in the blood, infectious agents provoke the formation of specific antibodies. The alveoli are affected, gas exchange is disrupted. In conditions of respiratory failure, pulmonary fibrosis develops, subsequently emphysema and pneumothorax.
Symptoms of the disease first look like signs of ARVI or laryngitis. The period of the first stage is up to 10 days. Weakness, severe cough, weight loss in the second stage of the disease are intensified by severe shortness of breath. The skin acquires a bluish tint. The cough becomes productive with sputum that is difficult to clear.
The third stage brings relief of symptoms, but wheezing in the lungs and symptoms of weakness may persist for a long time.
Treatment of Pneumocystis pneumonia occurs in a hospital and includes antibacterial and symptomatic treatment.
Mycoplasma pneumonia
Mycoplasma pneumonia is an atypical pulmonary infection. Infectious agent – Mycoplasma pneumoniae. This type of pneumonia is characterized by:
- obsessive cough,
- low-grade fever,
- chest pain and muscle pain,
- abdominal pain and disturbances in the gastrointestinal tract.
Mycoplasma pneumonia most often affects children, adolescents and adults under 35 years of age.
With a high prevalence of the disease, mycoplasmas are not very stable in external conditions. They respond to changes in temperature (in particular, heating) and do not grow in dry environments.
These microorganisms often cause bronchitis, bronchial asthma, and they can also cause non-respiratory pathologies (otitis, encephalitis, meningitis, anemia).
The incubation period for mycoplasma pneumonia is usually 12-14 days. The disease rarely begins acutely, more often it is the appearance of symptoms of laryngitis, less often - bronchitis. Weakness, sweating, and fever up to 38 degrees also accompany the onset of the disease.
Complications of mycoplasma pneumonia can include:
- Stevens-Johnson syndrome,
- Guillain-Barre syndrome,
- myelitis,
- encephalitis,
- meningitis.
If the disease is recognized at an early stage, it can be cured within two to three weeks. For treatment, macrolides, fluoroquinolones, bronchodilators, expectorants are prescribed; in the recovery stage, immunomodulators, physiotherapy, massage, and breathing exercises are prescribed.
Differences between pneumonia and bronchitis
Bronchitis and pneumonia are different diseases that affect the respiratory system. They have similar symptoms, so differentiating them can be difficult.
Main differences:
- In 90% of cases, bronchitis is caused by viruses, and pneumonia is caused by bacteria.
- During inflammation of the bronchi, body temperature rarely rises to feverish levels.
- Sputum with bronchitis is light. In patients with pneumonia, it looks green or yellow, and blood may appear in it.
- With bronchitis, wheezing in the lungs is dry, and with pneumonia, it is moist.
It is impossible to differentiate between pneumonia and bronchitis on your own; consultation with a specialist is necessary.
Pneumonia in children
Pneumonia in children is an acute infection of the lungs. She is short of breath. Cough and symptoms of intoxication.
Intrauterine infection with pneumonia occurs due to herpes viruses and chlamydia. Medicine already knows cases of intrauterine pneumonia caused by coronavirus.
In the first year of life, the most common causative agents of the disease are pneumococcus and Haemophilus influenzae. Preschoolers suffer from pneumonia, which is caused by:
- infection with Haemophilus influenzae and Escherichia coli,
- Staphylococcus aureus,
- Pseudomonas aeruginosa.
Schoolchildren are more likely to suffer from atypical pneumonia.
At risk for pneumonia are children with immunodeficiency, those who have suffered from stress, cold, or those suffering from chronic infectious diseases.
Treatment of pneumonia in children consists of antibiotics, antipyretics, expectorants, and bronchodilators. After the acute phase and during the rehabilitation period, physiotherapy, massage and physical therapy are indicated.
In case of timely detection, childhood pneumonia is treated at home, and in serious cases - in a hospital, and quite successfully. For childhood pneumonia, hospitalization is not always indicated, and if parents take medications responsibly, childhood pneumonia is cured within 2-3 weeks.
Diagnostics
Diagnosis of pneumonia includes the following steps:
- An initial visit to the doctor, during which he collects anamnesis, examines the patient, and listens to his breathing.
- Taking a chest x-ray. Darkening in the images allows you to visualize the inflamed areas.
- Donation of blood, urine and sputum for analysis. These studies allow us to assess the severity of inflammation (based on the level of leukocytes and ESR). The study of sputum provides information about the causative agent of the infection.
- CT or MRI of the lungs, fibrobronchoscopy. These studies are prescribed when the doctor still has doubts about the accuracy of the diagnosis.
Only a doctor can diagnose pneumonia based on a number of research procedures. Its symptoms have some similarities with bronchitis and other lung diseases. Therefore, you should not hesitate to contact a specialist.
Is pneumonia contagious?
Whether pneumonia is contagious or not depends on its type and the causes of the disease. At the same time, it is impossible to become infected with pneumonia directly, but pathogenic microflora, having penetrated the body of another person, can become a source of the inflammatory process, including pneumonia.
Pneumonia can be caused by bacteria, viruses, fungi, and protozoa. A person poses the greatest danger to others at the initial stage of the disease, when he coughs and releases infectious agents with his cough.
But it is important to remember that even with infection, the development of the inflammatory process may not occur. Strong immunity prevents pneumonia from developing, and all the fight against the infectious agent occurs in the upper respiratory tract. In other words, the same infectious agent can cause different reactions in different people: from mild ARVI to severe pneumonia.
The risk of developing pneumonia is greater:
- in children under 1.5 years old,
- old people,
- for those who suffer from immunodeficiency,
- suffering from chronic pathologies of the cardiovascular system, bronchi and lungs, kidneys,
- in diabetics,
- allergy sufferers,
- smokers.
It is important to remember that some types of pneumonia are not contagious. These are those types of disease that are not associated with infection. For example, pneumonia caused by stagnation of fluid in the respiratory tract.
Differences in older people
Pneumonia in older people is often diagnosed, which is associated with weakened immunity and deterioration of the protective functions of the respiratory system. The older the patient, the more vulnerable he is to infections.
The first sign of the disease is a cough. It is dry, sputum is released in minimal quantities.
Pneumonia is especially dangerous for patients with Alzheimer's disease, with weak immunity, and with a history of stroke. Their cough reflex is weakened, which is why the disease can remain undiagnosed for a long time.
A striking symptom of pneumonia in older people is severe shortness of breath. It bothers a person even after minimal physical activity and can appear at rest. Body temperature is most often elevated, but in 20% of cases it can remain within normal limits.
Sometimes the first sign of illness is apathy, which is accompanied by chronic fatigue, daytime sleepiness, and refusal to eat. A person ceases to be interested in the events happening around him, loses interest in matters that previously worried him. Urinary incontinence is often added to the listed symptoms. In such a situation, an incorrect diagnosis is often made - senile dementia. Doctors should be alert to exacerbations of chronic diseases, progression of diabetes mellitus or heart failure.
If the patient does not have a cough and the body temperature does not rise, the prognosis is less favorable. Delayed diagnosis leads to the development of complications.
Pneumonia in elderly bedridden patients is a serious problem faced throughout the world. The risk of developing pulmonary edema increases due to heart failure, emphysema and COPD.
Treatment of pneumonia
How many days does pneumonia take to be treated?
The duration of treatment depends on the underlying causes of pneumonia. Pneumococcal infection can be defeated in 7 days. Legionella or staphylococcus causes pneumonia, which must be treated for at least three weeks. Pseudomonas aeruginosa will force you to undergo therapy for up to forty-two days. Complicated pneumonia must be treated for up to two months.
Focal pneumonia is treated faster than lobar polysegmental pneumonia. In the first case, the clinical picture becomes favorable within ten days, in the second, treatment takes about a month.
Bilateral pneumonia in an adult. Duration of treatment
When predicting the treatment of bilateral pneumonia in an adult, one should always take into account chronic diseases, the state of immunity and the causes of the disease. Patients with severe metabolic damage, diabetes mellitus, high hypertension, and heart disease have a chance of longer treatment and long-term rehabilitation after pneumonia. The clinical picture can reveal symptoms of pneumonia up to two months from the start of therapy, while a strong body can recover in one month.
Clinical guidelines
The latest clinical recommendations for the treatment of pneumonia are contained in the letter of the Ministry of Health of the Russian Federation dated March 6, 2020 N 30-4/I2-2702 “On the algorithm for providing medical care to the adult population with community-acquired pneumonia.” The document is relevant and defines the procedure for diagnosis and treatment of all types of community-acquired pneumonia (those that developed outside the hospital, or those diagnosed in the first 48 hours from hospitalization). The letter defines the rules for hospitalization for pneumonia, the timing of the start of antibacterial therapy after diagnosis, the classification of forms of the disease by severity, based on symptoms.
Clinical guidelines provide as much detailed information as possible about the diagnosis and treatment of pneumonia, but they are addressed to doctors and medical personnel. Anyone can find them online and read them to raise awareness about the disease, but under no circumstances should you engage in self-diagnosis and self-medication according to prescribed antibacterial therapy protocols
. At the first signs of discomfort, you should consult a doctor.
Treating pneumonia at home
Clinical guidelines provide clear criteria for hospitalization of patients with pneumonia. Patients with a mild form of the disease and many of those suffering from moderate pneumonia without a significant medical history are treated at home.
The main rules for treating pneumonia at home:
- compliance with the antibacterial therapy protocol;
- keeping to bed for the first days and drinking plenty of fluids to relieve symptoms of intoxication;
- the need to get up every 5-6 hours and move slightly for up to 20 minutes;
- after normalization of the clinical picture, short walks are indicated;
- nutritious but light food;
- complete cessation of smoking;
- maintaining indoor air humidity within 60-70%.
Treatment with folk remedies
When treating pneumonia with medications, many also resort to folk remedies that support treatment. The most common of them are medicinal herbs. Herbal decoctions help with expectoration, reduce inflammation, and relieve bronchospasms.
Herbs reduce swelling and have a diuretic effect, activate the immune system, which well supports the therapeutic course.
It is useful to drink drinks rich in vitamin C: decoction of rose hips, cranberries, lingonberries, viburnum.
When treating pneumonia with folk remedies, garlic, honey are used, and various compresses and tinctures are made. With the abundance of folk recipes for the treatment of pneumonia, it is important to remember that consultation with a doctor is necessary in each case of their use
. Each folk remedy should be built into therapy and not interfere with its successful course. Therefore, if you want to resort to the help of traditional medicine, you should not overload the body and follow the principles of rationality and consistency with the main treatment protocol.
Symptoms for which you need to call an ambulance
You need to call an ambulance in the following cases:
- Consciousness is confused, the patient is delirious, and his coordination is impaired.
- Breathing is heavy, rapid.
- The upper pressure drops below 90 mm. Hg Art.
- The lower pressure dropped to 60 mm. Hg Art.
If a person has at least 1-2 of the signs listed, it is necessary to call a medical team. Pneumonia is regarded as severe if the patient is exhausted, suffers from alcoholism, diabetes, brain pathologies, and chronic lung diseases. An aggravating factor is age over 60 years.
Drugs for the treatment of pneumonia
Antibiotics for pneumonia
Patients with mild pneumonia are treated at home. It can usually be cured with tablets or suspensions. The doctor prescribes β-lactam antibiotics (amoxicillin, amoxin, flemoxin solutab). For older patients or with severe chronic diseases, protected penicillins and fluoroquinolones (amoxiclav, flemoclav solutab, avelox) are prescribed.
To treat patients with severe and extremely severe pneumonia, drugs of the 3rd and 4th generations are used, which have a bactericidal effect that completely destroys the pathogen cells. Among the representatives of the third generation cephalosporins are oral and parenteral forms. In the first subgroup, suprax in capsules and suspensions, cedex in capsules and specracef in capsules, cefditoren, ceftazidime, cefoperazone,
To destroy mycoplasmas in pneumonia, macrolide antibiotics that are active against atypical flora, tetracyclines - reserve drugs, doxycycline (Unidox Solutab) are suitable.
Adequate treatment of pneumonia cannot do without antibiotics. This is the only modern and effective measure to eliminate the cause of the disease - microorganisms. All drug prescriptions must be supervised by a doctor; self-medication is fraught with aggravation of the disease and the development of bacterial cell immunity to the effects of antibiotics.
Symptoms for which you need to call a doctor
A doctor should be called to your home if the following symptoms appear:
- The cough started to go away, but then suddenly got worse.
- Breathing became faster and shortness of breath appeared.
- When you take a deep breath, you experience chest pain.
- The sputum is yellow, green, or brown.
- The body temperature is not reduced by medications and remains at 38 degrees and above.
- The skin turns pale.
The reason to call a specialist should be a combination of 3 or more symptoms.
Breathing exercises
To prevent pneumonia
Today, the prevention of pneumonia is one of the most important in the complex of health practices and care for the condition of the human body. It has become obvious that lung damage is a real threat, much more widespread and urgent than it seemed to many of us just recently. The coronavirus pandemic has made adjustments not only to our way of life, but has also made it extremely important to take care of our respiratory system and its healthy and complete state.
One of the most effective ways to prevent pneumonia is regular breathing training with the Samozdrav simulator. And there are justified reasons for this and many years of indisputable evidence.
Breathing exercises strengthen the respiratory muscles, which increases the mobility of the chest and diaphragm. Effective movements of the respiratory muscles increase the volume of the chest and lungs. This ensures maximum pulmonary ventilation and air circulation in the alveoli and increases the utilization rate of oxygen in the lungs and its delivery to the tissues.
Maintaining normal lung volumes and regular training of the respiratory muscles forms the correct respiratory rhythm. As a result of this, the respiratory rate, its minute volume and other indicators that are disturbed due to stress, physical inactivity, and chronic diseases are normalized. Physiologically correct breathing is maintained for a long time.
Breathing exercises maintain the elasticity of the lung tissue. This increases the vital capacity of the lungs and prevents the development of fibrosis and other changes in the lung tissue. CO2 eliminates bronchospasm, which also increases breathing efficiency.
Breathing training increases the efficiency of the pulmonary circulation. This is especially important for older people, because one of the common causes of pneumonia in the elderly is stagnation of blood in the small circle.
As a result of restoration of the functions of the respiratory system and blood circulation, the inflammatory process is reduced, congestion in the bronchi and lungs is prevented, and mucus and exudate are reabsorbed.
In addition, Samozdrav compensates for the lack of physical activity, and breathing training, like physical exercise, promotes the production of a natural antioxidant (superoxide dismutase), which prevents the development of pneumonia.
All these arguments are the result of numerous in-depth studies related to the study of the effect of breathing training with Samozdrav on human lungs and the prevention of pneumonia, as well as the experience of people of different ages and different levels of health.
Today, millions of people from around the world train with Samozdrav to prevent the development of pneumonia - one of the main dangers to the body during a pandemic.
If you want to get one of the most effective ways to take care of your respiratory system, an indispensable assistant for the prevention of pneumonia, purchase the Samozdrav breathing simulator. Years of experience have proven its effectiveness, accessibility and the highest results in maintaining lung health.
For rehabilitation after pneumonia
During a difficult period of threats of a high viral load on the body, it is important to know how to quickly get back into shape after pneumonia and allow your lungs to work at full strength again. Firstly, it is important to follow the general rules of caring for yourself and your health. Sleep at least 8 hours at night and a couple of hours during the day, eat well, not forgetting vitamins A, B, C and calcium, ventilate the room every three hours.
Particular attention should be paid to your lungs, devoting time to breathing exercises to improve pulmonary circulation and strengthen the pulmonary muscles. Through breathing training with the Samozdrav simulator, exudate will be absorbed, sputum separation will be facilitated, the airways will be cleared, lung tissue will remain healthy and elastic, tissue metabolism will be normalized and intoxication that accompanies the acute stage of the disease will be eliminated. Healthy breathing and normal inspiratory volume will be restored, shortness of breath will go away due to the normalization of oxygen levels in the body,
In the process of breathing training with the Samozdrav simulator, rehabilitation after pneumonia will be successful, it will be quick and comfortable, and you will be able to regain your vital energy in a natural way - by training through correct and healthy breathing.
Treatment at the Yusupov Hospital
Pneumonia is a rather complex and unpredictable disease that requires compliance with all doctor’s instructions, thanks to which it is possible to prevent a sharp deterioration in the patient’s well-being and aggravation of the disease.
Yusupov Hospital in Moscow offers high-quality diagnostics and effective treatment of pneumonia. The specialists of our clinic, whose competence is confirmed by international certificates, will provide comprehensive support until the patient’s complete recovery.
Thanks to the clinic being equipped with modern diagnostic and treatment equipment, our doctors have the opportunity to obtain the most reliable research results and select a treatment method for pneumonia that is most effective for a particular type of disease.
The Yusupov Hospital has its own hospital, where patients can expect comfortable rooms, good nutrition, round-the-clock staff assistance and an individual approach. You can make an appointment with a doctor by calling the clinic.
At-risk groups
There are risk groups that are most susceptible to pneumonia. Their representatives do not necessarily become victims of this complication, but their chances of suffering from the disease are much higher than for other people. In order to take timely care of your health and prevent complications, you should know the risk factors that can lead to illness. The risk group includes:
- people with weak immunity - patients with immunodeficiency, who have recently undergone surgery, weakened by a long-term illness, etc.;
- people with chronic diseases that constantly weaken the immune system;
- taking hormonal medications (they also lower immunity);
- people who are in a state of clinical depression and constant stress;
- pregnant women or women who have recently given birth;
- patients who have had ARVI or influenza;
- people with alcohol or drug addiction.
Sources and reference materials
To download, click on the desired document:
| # | File | file size |
| 1 | Consequences of community-acquired pneumonia and possibilities for their prevention | 2 MB |
| 2 | Restorative treatment of patients with prolonged pneumonia with the inclusion of coolants | 2 MB |
| 3 | Protracted pneumonia | 181 KB |
| 4 | Disease history. Community-acquired lower lobe right-sided pneumonia. Prolonged flow. Acute bilateral catarrhal sinusitis | 118 KB |