Chronic obstructive pulmonary disease (COPD) is a slowly progressive disease of the respiratory tract.
If COPD is not detected and treated in time, it develops, worsening the quality of life - breathing will become difficult, shortness of breath will interfere with daily activities and work. A constant lack of oxygen leads to serious consequences, primarily to heart failure, arrhythmia, and heart attack. Emphysema and bronchiectasis, pulmonary fibrosis, bullae in the lungs, and pneumothorax that form in COPD are complications of this disease and can lead to hospitalization. More than 2.5 thousand patients with COPD have been treated in our clinic. A third of them came to us without knowing about their diagnosis. Many were treated for asthma without providing adequate care and allowing the disease to progress. There are patients who were diagnosed in vain and they needlessly purchased expensive medications and experienced stress from this diagnosis.
Many years of experience gained while working at the Pulmonology Research Institute allows our pulmonologists to help patients breathe normally, reduce the frequency of exacerbations, and avoid complications.
In 60–80% of patients with Chronic Obstructive Pulmonary Disease (COPD), doctors do not detect this disease.
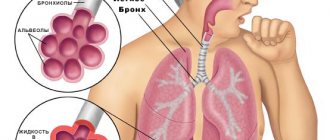
Basic concepts for COPD:
- An obstruction
is an obstacle to the free passage of air. Inflammation processes inside the bronchi lead to their narrowing and difficulty in the passage of air through the bronchi. Therefore, COPD is a broncho-obstructive disease. - Emphysema
- (in Greek “I inflate”) is a pathological expansion of the pulmonary sacs (alveoli) and adjacent parts of the respiratory tract (distal bronchioles), as a result of which the lungs become excessively “inflated”. - Bronchitis
- long-term inflammation of the walls of the bronchi leads to their thickening and deformation. The bronchial mucosa loses its ability to cleanse itself. This leads to sputum retention and coughing.
Impact of COPD on quality of life
Common symptoms of COPD begin to appear in middle age and include:
- shortness of breath or difficulty breathing;
- chronic cough, often with sputum production; and/or
- fatigue.
As COPD progresses, it becomes increasingly difficult for the person to perform normal daily activities, often due to shortness of breath. The associated loss of productivity and home restrictions, as well as medical expenses, result in a significant financial burden.
During exacerbations, COPD symptoms become much more severe and patients may require additional home care or hospitalization for emergency care. Severe exacerbations can threaten the patient's life.
People with COPD often have comorbidities such as cardiovascular disease, osteoporosis, musculoskeletal disorders, lung cancer, depression and anxiety disorders.
Symptoms of COPD
The main clinical manifestations of the disease are:
- Shortness of breath - when damage to the bronchi and bronchioles becomes severe, a problem with gas exchange in the body arises: it becomes increasingly difficult to obtain enough oxygen and get rid of excess carbon dioxide. These changes lead to shortness of breath and increased heart rate.
- Prolonged cough with difficult to clear viscous sputum - cough becomes a constant companion of a person. The sputum changes color from gray to green. It depends on the attached bacterial infection.
- Wheezing. Shortness of breath and cough are accompanied by wheezing and whistling in the chest. The narrowing of the lumen of the bronchus causes whistling sounds when breathing. Phlegm inside the bronchi enhances or changes these sounds.
- Decreased tolerance to physical activity - if previously a person could easily climb to the 3rd floor or run after a bus, then with COPD it is difficult to do this. You need to catch your breath, restore your breathing.
Cases of false-positive diagnosis of COPD occur from 5% to 65% worldwide - the diagnosis is made, but in fact the person does not have it.
When should you see a doctor?
The development of the disease takes more than one year. Many patients smoke more than a pack of cigarettes daily and expose their health to serious risks. The first sign indicating COPD is an active cough, which often occurs in people between forty and fifty years of age who smoke.
You should consult a doctor if the patient begins to notice a productive cough, progressive shortness of breath, worsening and increased recovery time during ARVI.
Symptoms continue to worsen if the patient continues to smoke. At an advanced stage, headaches are observed after waking up, hypercapnia and hypoxemia during night rest.
You should consult a doctor if you have the following symptoms:
- prolongation of the exhalation phase;
- whistling sound when inhaling or exhaling;
- muffled heartbeat in a calm state;
- increase in chest size;
- rapid weight loss, which is especially important for patients with emphysema;
- muscle weakness and constant fatigue.
Diagnosis of COPD
In order to answer the question of COPD or not, it is necessary to conduct two mandatory studies:
- Spirometry (SP) - having received the test results, the doctor assesses the degree of obstruction according to the GOLD (Global initiative for Obstructive Lung Disease) recommendations, and receives an answer whether the patient has COPD. Depending on the degree of narrowing of the bronchi, the pulmonologist prescribes medications - inhalers.
- CT scan of the chest - this study will show changes in the lung tissue - bronchial deformities, emphysema, bullae in the lungs. A doctor can visually assess the severity of changes in a patient with COPD.
Additional research methods are body plethysmography and diffusion test. These are special studies necessary to monitor the course of the disease and prevent its progression.
Stages of the disease:
- Mild severity – GOLD 1, FEV1 is more than 80% of the expected value (FEV1 is the expiratory rate in one second, the indicator is obtained by performing FEV)
- Moderate severity GOLD 2, more than 50% FEV1 less than 80%
- Severe severity GOLD 3, more than 30% FEV1 less than 50%
- Extreme severity GOLD 4, FEV1 less than 30%
To assess the risk of COPD progression, an important indicator is the number of COPD exacerbations per year. It has been proven that the more limited the air flow through the bronchi due to their narrowing (low FEV1), the more frequent the exacerbations and the risk of death.
Global Alliance to Fight Chronic Respiratory Diseases
The Global Alliance Against Chronic Respiratory Diseases (GARD) promotes WHO's work to prevent and control chronic respiratory diseases. GARD is a broad voluntary alliance of national and international organizations and institutions working towards the common goal of reducing the global burden of chronic respiratory diseases.
Bibliography
1. WHO Global Health Estimates
2. Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2022 global survey. Geneva: World Health Organization; 2022. License: CC BY-NC-SA 3.0 IGO
Treatment of COPD
Treatment of COPD is a long and consistent process that should be carried out under the supervision of a pulmonologist. The main groups of medications used in our clinic:
- Bronchodilators.
Their task is to expand the bronchi as much as possible and keep them in an expanded state for as long as possible. This gives relief in breathing. Modern drugs have a 24 hour effect. In combination with short-acting bronchodilators, they can reduce shortness of breath, shortness of breath, wheezing and whistling. - Expectorants or mucolytics
- thin the mucus and do not allow it to linger in the bronchi. If a mucus plug forms in a narrowed bronchus, the person will not be able to breathe normally. He will be choking and coughing constantly. Modern expectorants reduce the viscosity of sputum, and some prevent pulmonary fibrosis. The drugs are administered through a nebulizer, using tablets or intravenously. - Antibiotics
are necessary to treat exacerbations of COPD. They must act quickly and reliably. Patients often have antibiotic-resistant microflora in their bronchi. Then the pulmonologist must prescribe the correct antibiotic or combination of antibiotics. - Hormonal drugs
are effective in patients with concomitant asthma (loop syndrome). Sometimes, during exacerbation of severe COPD, they are used in the form of intravenous administration or tablets.
The objectives of all of the above remedies are to restore breathing, reduce cough and sputum production, reduce shortness of breath, restore strength for work and life, and prevent complications.
Causes of obstructive disease
The main cause of the development of pathology is chronic smoking. There are a number of other factors that can trigger the onset of COPD:
- abundance of exhaust gases, smoke, dust;
- air pollution from industrial waste;
- work in hazardous conditions (coal mine, hot shop, chemical industry);
- climatic features (dampness, constantly high humidity);
- infectious microorganisms (influenza virus, pneumococcus, mycoplasma bacteria and others);
- development of concomitant pathologies of the bronchi and lungs, especially bronchial asthma (including inherited).
Pulmonary rehabilitation for COPD
Our Pulmonology Department has developed a “Pulmonary Rehabilitation Program for Patients with Chronic Obstructive Pulmonary Disease.”
A course of complex therapy can replace bronchoscopic sanitation in patients with bronchiectasis.
- sputum becomes easily coughed up, coughing occurs naturally, medications are poured into the smallest bronchi, including antimicrobial agents.
- the introduction of drugs into the bronchus and removal of sputum is not invasive and traumatic.
- Due to the positive effect of drainage techniques and special exercises included in the course, lymphatic drainage of the bronchi and their blood supply improve. As a result, the protective properties of the mucous membrane of damaged bronchi and surrounding lung tissue are enhanced.
- There are no risks inherent in bronchoscopy: the risk of bleeding, damage and allergic reaction to anesthesia.
Chronical bronchitis
| Long-term inflammation of the airways is characterized by excessive mucus production and a persistent cough. Damage to the bronchial tubes causes chronic bronchitis. Bronchitis occurs when the bronchi become irritated and swollen. This causes coughing and shortness of breath. If phlegm appears when you cough, and the cough continues for at least three months for two years in a row, bronchitis is called chronic. There are hair-like fibers lining the bronchi. These tiny hairs are called cilia. The cilia help move mucus down the bronchi so it can be coughed up. With chronic bronchitis, eyelashes lose their mobility. This makes it more difficult to cough up mucus from the lungs, causing a more severe cough. Mucus may accumulate in the lungs. Smoking interferes with the normal functioning of eyelashes. |
FAQ
Can asthma develop into COPD?
No. Quite a common misconception. These are two completely different diseases. They are united by one syndrome - broncho-obstructive. In both cases, the pulmonologist is faced with narrowing of the bronchi - broncho-obstruction. In the case of COPD it is not reversible, in the case of asthma it is reversible. Disease outcomes are also different. The treatment of diseases has common features, but is still completely different. Many therapists and pulmonologists immediately prescribe medications used for asthma and COPD to a patient with COPD. But this is completely wrong.
Why does one patient need one inhaler, and another three?
Prescribing therapy for COPD is a very delicate matter. It all depends on the stage of the disease, its form (phenotype), and the frequency of exacerbations. This is clarified during an examination and consultation with a pulmonologist. In addition, COPD is a disease in which there are concomitant diseases. For example, heart or vascular diseases, diabetes.
All of them aggravate the course of the disease and drugs prescribed for the treatment of COPD can worsen the course of concomitant diseases. And this must be taken into account. COPD should only be treated by pulmonologists. Do not self-medicate and contact only specialists. Beware of ignoramuses and charlatans!
Do you need to breathe oxygen if you have COPD?
Prescribing oxygen therapy is no less complex than prescribing drug treatment for a disease. Not every patient with COPD needs oxygen. It is possible to correctly prescribe inhalation therapy, expectorant medications and antibiotics to increase oxygen in the blood, without the use of oxygen.
Incorrectly prescribed oxygen therapy can worsen the prognosis of the disease or fail to achieve the desired effect. Many doctors, seeing reduced oxygen levels in a COPD patient, rush to prescribe oxygen therapy without finding out whether it is necessary or safe?!
In order to find out whether an oxygen concentrator is needed, long-term (night, daily) pulse oximetry is used. The study is carried out either at night or during the day. The test measures blood oxygen concentration and heart rate continuously over many hours. Based on the results of pulse oximetry, the pulmonologist will select the oxygen supply mode - the frequency, the speed of its supply, and the duration.
Is there any surgical treatment for COPD?
Yes, surgical treatment is available for some forms of the disease. First of all, this is bullous emphysema. This is a variant of emphysema in which cysts and bullae (cavities in the form of large bubbles) form in the lungs. Surgery is performed using modern endoscopic technology.
Also, according to indications, in case of extremely severe COPD, a lung transplant is possible.
In both cases, lung surgery is a dangerous and complex procedure that requires high skill from thoracic surgeons.
Is COPD bronchitis or emphysema?
The term chronic obstructive pulmonary disease is often used along with diseases such as bronchitis and/or emphysema because they are the most common clinical forms of this disease (COPD). In other words, emphysema or chronic obstructive bronchitis is COPD.
Moreover, the treatments for COPD, chronic obstructive bronchitis, and emphysema are similar. But the outcomes of simple chronic bronchitis and COPD are different. This is why it is so important to make a correct diagnosis.
Emphysema
| Destruction of lung tissue in the alveoli (air sacs), which causes respiratory failure. The walls inside the alveoli collapse, turning many small sacs into one large bubble (larger sacs). These larger sacs do not carry oxygen from the air into the blood. In addition, when the alveoli are damaged, the lungs stretch and lose their elasticity; The airways become flabby, some of the air is retained in the lungs, as a result of which the supply of oxygen to the blood and the removal of carbon dioxide are disrupted. |
Our specialists
Chikina Svetlana Yurievna
Candidate of Medical Sciences, pulmonologist of the highest category. Official doctor, expert at Russian congresses on pulmonology.
30 years of experience
Kuleshov Andrey Vladimirovich
Chief physician, candidate of medical sciences, pulmonologist, somnologist, member of the European Respiratory Society (ERS).
Experience 26 years
Meshcheryakova Natalya Nikolaevna
Candidate of Medical Sciences, pulmonologist of the highest category, associate professor of the Department of Pulmonology named after. N.I. Pirogov.
Experience 26 years
Nikitina Natalia Vladimirovna
Deputy chief physician, pulmonologist, allergist of the highest category. Full member of the European Academy of Allergy and Immunology.
Experience 15 years
Publications in the media
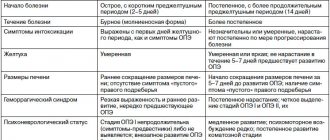
Chronic obstructive pulmonary disease (COPD) is a disease characterized by a partially irreversible, steadily progressive limitation of airflow caused by an abnormal inflammatory response of lung tissue to damaging environmental factors. The term “COPD” refers to a combination of chronic bronchitis and secondary pulmonary emphysema. Classification of COPD is based on the severity of the disease • Stage 0 (increased risk of developing COPD): normal spirometry, chronic symptoms (cough, sputum production) • Stage I (mild): FEV1/FVC <70%. OVF1³80% of due. Presence/absence of chronic symptoms (cough, sputum production) • Stage II (moderate): FEV1/FVC <70%. 30% £OVF1 £80% of due (IIA 50% £OVF1 £80%). (IIB 30% £OVF1 £50%). Presence/absence of chronic symptoms (cough, sputum production) • Stage III (severe): FEV1/FVC <70%. RVF1 <30% of predicted or RVF1 <50% of predicted, in combination with respiratory failure (PaO2 less than 8.0 kPa [60 mm Hg] with or without PaCO2 more than 6.7 kPa [50 mm Hg. ] when breathing at sea level) or clinical signs of right ventricular failure.
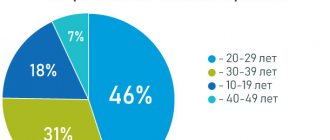
Statistical data. 1849.2 cases per 100,000 population over 18 years of age; 548.8 cases - 15–17 years; 307.7 cases are under 14 years of age. According to WHO, the prevalence of COPD among men is 9.34/1000, and among women - 7.33/1000. People over 40 years predominate. COPD is in 6th place among the leading causes of death in the world, in 5th place in developed countries of Europe, and 4th in the USA.
Etiology. The development of COPD is promoted by smoking, occupational hazards (dust, irritants, smoke, fumes, etc.), air pollution (at home - products of fossil fuel combustion, odors of cooked food, heating appliances). Severe respiratory infections in childhood predispose to the development of COPD throughout life. The risk of developing COPD is inversely proportional to socioeconomic status.
Genetic features. COPD does not develop in all individuals who have antitrypsin defects, leading to the early development of panlobular emphysema. Emphysema due to deficiency of: • a1-antitrypsin (*107400, mutations of the PI, AAT, 14q32.1, Â genes) - liver cirrhosis, absence of a1-globulin peak in serum protein electrophoresis, a small amount of serum a1-antitrypsin and panlobular (covering all departments) emphysema, more pronounced in the basal parts of the lungs • Insufficiency of a2-macroglobulin. (*103950, 12p13.3–p12.3, Â).
Pathogenesis . The inflammatory process is induced by various pollutants and gases. Tobacco smoke has a direct damaging effect on lung tissue and the ability to cause inflammatory changes. Chronic inflammatory process of the respiratory tract, pulmonary parenchyma and blood vessels is characterized by an increased number of macrophages, T-lymphocytes and neutrophils. Activated inflammatory cells release a large number of inflammatory mediators (leukotriene B4, IL-8, TNF-a, etc.) that can damage the structure of the lungs and maintain inflammation. In addition to inflammation, an imbalance of proteolytic enzymes and antiproteinases, oxidative stress are essential in the pathogenesis of COPD • Bronchitic component •• At an early stage, bacterial contamination, inflammation, mucus blockage, peribronchiolar fibrosis and obliteration are detected in small bronchi (diameter <2 mm) •• With formed pathology - hyperplasia of the mucous glands, serous inflammation and edema; bronchospasm and blockage of the airways with secretions lead to bronchial obstruction • Emphysematous component •• Destruction of the alveolar walls and supporting structures leads to the formation of significantly expanded air spaces •• Increased airiness of the lung tissue leads to narrowing of the airways during dynamic collapse during exhalation (expiratory bronchial collapse) •• Destruction of the alveolar-capillary membrane reduces the diffusion capacity of the lungs.
Pathomorphology. Pathological changes in large and peripheral bronchi, pulmonary parenchyma and pulmonary vessels. In the trachea, bronchi and bronchioles with a diameter of more than 2–4 mm, inflammatory cells infiltrate the surface epithelium. Hypersecretion of mucus is also observed. Damage and restoration of the bronchial wall are repeated cyclically, its structural remodeling occurs, the collagen content increases and the formation of scar tissue narrows the lumen and leads to fixed airway obstruction. Microdestruction of the pulmonary parenchyma leads to the development of centrilobular emphysema, hence dilatation and destruction of the respiratory bronchioles. Thickening of the vascular intima is their first structural change with a further increase in the content of smooth muscle elements and infiltration of the vascular wall with inflammatory cells. As COPD progresses, the accumulation of large amounts of SMC, proteoglycans and collagen contributes to further thickening of the vascular wall.
Clinical manifestations
• Complaints: epidemiological criterion for COPD is a chronic productive cough lasting more than 3 months a year for 2 or more years in a row; shortness of breath of an expiratory nature, increasing over time, intensifying during an exacerbation.
• Physical examination: upon examination (in later stages) the participation of accessory respiratory muscles; on auscultation - prolonged exhalation, dry scattered wheezing with quiet breathing, wheezing with forced exhalation, moist wheezing more often with exacerbation; during percussion - from a boxy tint to a distinct boxy sound. Tachycardia, accent of the second tone over the pulmonary artery.
• Laboratory data: during the period of exacerbation, leukocytosis, increased ESR, neutrophil band shift; in severe cases - polycythemia (erythrocytosis), hypercapnia, hypoxemia, decreased levels of a1-antitrypsin in the serum and the absence of an a1-globulin peak in serum protein electrophoresis; bacteriological examination of sputum makes it possible to identify the causative agent of exacerbation of chronic bronchitis and exclude tuberculosis.
• Instrumental data •• Spirometry is a criterion for diagnosis and severity (decrease in forced expiratory volume in 1 s (FEV1) with a concomitant decrease in the Tiffno index, minimal dynamics of parameters (less than 15% of the original) after the introduction of bronchodilators; forced vital capacity within normal limits or reduced; increase in residual lung volume; diffusion capacity within normal limits or reduced •• ECG: increasing signs of pulmonary hypertension, hypertrophy of the right heart, chronic pulmonary heart disease •• EchoCG: signs of pulmonary hypertension •• Chest X-ray in COPD reveals increased and deformation of the bronchopulmonary pattern, with emphysema - a heart of normal size, increased airiness of the lung tissue, flattening of the diaphragm and bullous changes
Types of COPD. There are 2 classic types of COPD, which have different names. Emphysematous patients with shortness of breath (COPD type A) are classified as “pink puffers”, bronchitis patients with a characteristic cough (COPD type B) are referred to as “blue puffers”.
• “Pink puffers” suffer predominantly from emphysema with a slowly progressive course, more often after 60 years •• Loss of body weight •• Progressive shortness of breath on exertion •• Productive cough •• Auscultation: weakened breathing, isolated wheezing •• Hypoxemia and hypercapnia are moderately expressed •• The diffusion capacity of the lungs is reduced •• The respiratory function indicators improve little after inhalation of bronchodilators.
• “Blue edema” suffer predominantly from chronic bronchitis •• Productive cough •• Episodic shortness of breath •• Weight gain at a young age •• Auscultation: dry rales •• Cor pulmonale often develops with signs of right ventricular failure •• Severe hypoxemia and hypercapnia as a result of fatigue respiratory muscles or decreased central stimulation of breathing •• Polycythemia •• Improved respiratory function after inhalation of bronchodilators •• The diffusion capacity of the lungs is slightly affected.
• Mixed variants are more often observed, combining the signs of “pink puffs” and “blue puffs”.
Diagnostic tactics. The basis of diagnosis when contacting is to identify patients with chronic cough and exclude other causes of cough (sputum examination, radiography); optimal diagnosis is detection of FVD during a screening study (reduction of FVD1).
Concomitant diseases that aggravate the course and worsen the prognosis of COPD: obesity, sleep apnea syndrome, heart failure, diabetes, arterial hypertension.
Treatment • General tactics: cessation of exposure to harmful factors on the lungs • Regimen and diet: stay in the fresh air, avoid hypothermia, contact with patients with respiratory infections; annual anti-influenza and anti-pneumococcal vaccination; physical training programs • Drug treatment outside of exacerbation: anticholinergic bronchodilators (ipratropium bromide) or combinations with b2-agonists (inhalation from a can, through a spacer or nebulizer), long-acting theophyllines. Inhaled GCs with the effectiveness of an initial two-week course of systemic steroids (improved respiratory function parameters). Expectorants with antioxidant properties (acetylcysteine, ambroxol). Regular use of cough suppressants and narcotic drugs for COPD is contraindicated. a1-Antitrypsin - in case of its deficiency. Long-term oxygen therapy at stage III for hypoxia (paO2 less than 60 mm Hg) • Drug treatment for exacerbation: short-acting inhaled β2-agonists (salbutamol) during therapy with anticholinergic drugs (ipratropium bromide), methylxanthines with caution (monitoring serum concentrations) . GC intravenously or orally (30–40 mg 10–14 days per os). Antibiotics only in the presence of purulent sputum (aminopenicillins, cephalosporins of II-IV generations, new macrolides, pneumotropic fluoroquinolones of III-IV generations). At stage III, oxygen therapy is supplemented with auxiliary ventilation • Surgical treatment: bullectomy, surgical correction of lung volume, lung transplantation • Peculiarities of treatment in old age are determined by the presence of concomitant diseases (limitation of xanthines, sympathomimetics, combination with cardiovascular drugs) • Peculiarities of management of pregnant and lactating women are associated with increasing hypoxemia in COPD (oxygenation control), possible teratogenicity of the drugs used.
Complications and their treatment. Frequent infections (antibacterial therapy); secondary pulmonary hypertension and cor pulmonale (oxygenotheria, decreased pulmonary pressure); secondary polycythemia (oxygen therapy); acute or chronic respiratory failure.
Prevention. Fighting smoking, improving production and the environment.
Course and prognosis of the disease. The course is steadily progressing. The prognosis depends on the rate of decline in FEV1.
Synonyms: chronic obstructive bronchitis, obstructive emphysema.
Abbreviations EF1 - forced expiratory volume in the first second • FVC - forced vital capacity.
ICD-10 • J43 Emphysema • J44 Other chronic obstructive pulmonary disease
Recommendations for patients with COPD
An important factor in the effectiveness of COPD therapy is its regularity, so it is necessary to continue treatment even with a significant reduction in the symptoms of the disease.
In addition to drug therapy for COPD, you should eat a balanced diet rich in animal proteins and maintain a sufficient level of physical activity.
Author:
Akulkina Larisa Anatolyevna pulmonologist
Prevention of influenza and pneumococcal pneumonia
Because pulmonary infection is common in patients with COPD and can lead to deterioration of lung function and respiratory failure, annual influenza vaccination is recommended for patients who are not allergic to egg whites. Its effectiveness reaches 60-80%. Unvaccinated patients at high risk of influenza A and at an early stage are prescribed amantadine. For patients over 50 years of age, a single immunization with the pneumococcal vaccine is also recommended. Revaccination is now carried out after five or more years, if at the time of vaccination the patient’s age did not exceed 65 years.
Physiotherapy
Removing mucus from the respiratory tract can significantly improve the patient’s well-being, especially with the bronchitis type of COPD. There are many ways to clear mucus from your airways and prevent it from accumulating. Cough in patients with COPD, as a rule, does not remove sputum and is only exhausting. Such patients can be advised to use a simple and effective method of coughing up sputum, which, unfortunately, is often neglected. Its essence is as follows: after a couple of slow deep breaths, you need to hold your breath for 5-10 seconds to increase intrathoracic pressure and then, as you exhale, cough with an open glottis.
Postural drainage, vibration and percussion massage
facilitate the removal of mucus from the lower parts of the lungs due to the action of gravity and the oscillatory movements of the chest imparted to it during percussion or using a vibrator. Upon completion of the procedure, the patient should cough well, as described above.
All of the described methods facilitate the removal of sputum in one way or another, but only coughing with an open glottis can still move sputum into the trachea and large bronchi, from where it can be removed by coughing or by aspiration.