Cardiopulmonary failure is a decompensated stage of cor pulmonale, which occurs with acute or chronic right ventricular heart failure. The occurrence of pathology is associated with impaired blood circulation in the vessels of the lungs, which is accompanied by a decrease in blood oxygen saturation.
There are two main forms of cardiopulmonary failure - acute and chronic. The acute form in most cases occurs as a result of asthma, emphysema or massive thromboembolism. Clinical signs appear several hours after a sharp increase in arterial pressure. The chronic form is characterized by slow development with an increasing clinical picture (it can develop over several months or years).
There are several types of cardiac pulmonary failure, which differ in their characteristic symptoms. Among them: cerebral, anginal, respiratory, abdominal and collaptoid type of pathology. The cerebral type is characterized by signs of encephalopathy (for example, drowsiness and lethargy or, on the contrary, excitability and aggressiveness). Some patients complain of headaches and dizziness.
The anginal type is characterized by the appearance of severe pain in the area (with no irradiation) and a feeling of lack of oxygen. The progression of the respiratory type is accompanied by the appearance of shortness of breath, cough and cyanosis of the skin. The abdominal type is characterized by painful sensations and a feeling of nausea. Without further treatment, stomach ulcers may occur. The collaptoid type is accompanied by a persistent increase in blood pressure, tachycardia and general weakness. In this case, patients experience pallor of the skin.
Circulatory failure depends on two main factors: a decrease in the contractile force of the muscular membrane of peripheral vessels and a decrease in the contractility of the muscular organ. If the first factor significantly predominates, then we are talking about vascular circulatory failure, and if the second predominates, we are talking about chronic heart failure.
The left and right sections of the muscular organ are responsible for blood circulation. When one of these sections is damaged, isolated or predominant lesions appear, respectively, on the left or right half of the muscular organ. Based on this, left ventricular failure and right ventricular failure are distinguished.
From an anatomical and functional point of view, the lungs and heart have a close relationship. This explains the fact that when one organ is damaged, negative consequences subsequently affect the other. Depending on which of these organs is more affected, pulmonary-cardiac and cardiopulmonary failure are distinguished.
There are two main phases – compensation and decompensation. In the compensation stage, the muscular organ is able to cope with its load and work. But this does not always happen: over time, a period comes when its internal reserves are completely exhausted, resulting in a decompensation phase. In this phase, the muscular organ is no longer able to cope with the load.
First aid for pulmonary edema
Unlike the chronic form, the acute form of the pathology requires immediate assistance during an attack. A person is not able to help himself, so he needs help from the outside. First of all, you should call an emergency team. While waiting for her, the person should be seated on a chair and given a Nitroglycerin tablet. If the attack occurs indoors, be sure to open all windows to provide fresh air flow.
If a person gets worse, cardiopulmonary resuscitation methods are required. To do this, rhythmically press on the chest area or do 30 presses and mouth-to-mouth breathing (alternating these actions). The main goals of these measures are to normalize blood circulation and restore respiratory function. If you lack the skills, you can simply massage the sternum.
Functional classes
During the examination, it is necessary to establish the functional class of manifestations of cor pulmonale.
- Class 1 - the main symptoms are diseases of the bronchi and lungs, hypertension in the pulmonary circle is detected only with instrumental examination and stress tests;
- Class 2 - in addition to the listed symptoms, there is respiratory failure due to narrowing of the bronchi;
- Class 3 - respiratory failure is severe, followed by cardiac failure. Constant shortness of breath, tachycardia, dilatation of the neck veins, cyanosis. Studies reveal persistent hypertension in the pulmonary circulation;
- Class 4 - decompensation, all clinical manifestations are pronounced, there are congestion, respiratory and heart failure of the third degree.
Doppler examination allows you to quantify the pressure in the pulmonary artery, measure the reverse flow of blood (regurgitation) from the right ventricle into the atrium
Causes of cardiopulmonary failure
Cardiopulmonary failure never occurs without a reason. As a rule, several reasons lead to its development. There are three main groups of causes that can provoke pathology:
1. Bronchopulmonary diseases. According to statistics, they act as a provoking factor in more than 70% of all cases. Among the most common diseases are bronchial asthma, pulmonary tuberculosis, chronic bronchitis and other severe disorders of the respiratory system (for example, cystic fibrosis).
2. Thoradiaphragmatic diseases. They are directly related to pronounced deformation of the chest and limited mobility of the diaphragm. The appearance is caused by severe curvatures of the spinal column (in particular, kyphoscoliosis), ankylosing spondylitis, and restrictions on the expansion of the lungs (pleuritis).
3. Vascular diseases. This group includes diseases that affect lesions of the pulmonary bed. These include sickle cell anemia, pulmonary vasculitis, compression of the pulmonary veins and arteries by neoplasms.
4. Vascular diseases. Often, the development of cardiopulmonary failure is provoked by aneurysms, atherosclerosis and blood clots in the arteries of the lungs.
What happens in the body
In patients of groups 1 and 2, all changes develop due to spasm of small arterioles in the lung tissue as a reaction to insufficient oxygen supply. In group 3, in addition to spasm, there is a narrowing or blockage of the vascular bed. The pathogenesis of the disease is associated with the following mechanisms.
- Alveolar hypoxia (lack of oxygen in the alveoli) - scientists associate vascular spasm in response to hypoxia with disturbances in sympathoadrenal regulation. There is a contraction of vascular muscles, an increase in angiotensin-converting enzyme (ACE), calcium in the blood, and a decrease in relaxation factors of the pulmonary vessels.
- Hypercapnia - an increase in the concentration of carbon dioxide in the blood does not directly affect the vascular wall, but through acidification of the environment and a decrease in the sensitivity of the respiratory center of the brain. This mechanism enhances the production of aldosterone (adrenal hormone), which retains water and sodium ions.
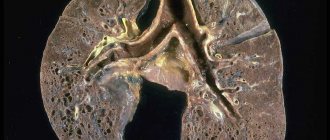
- Changes in the vascular bed of the lungs - compression and emptying of capillaries due to developing fibrous tissue is important. Thickening of the muscular walls of the pulmonary vessels contributes to the narrowing of the lumen and the development of local thrombosis.
- An important role is played by the development of anastomoses (connections) between the bronchial arteries, belonging to the systemic circulation, and the pulmonary vessels.
- The pressure in the systemic circle is higher than in the lungs, so the redistribution goes towards the pulmonary vascular bed, which further increases the pressure in it.
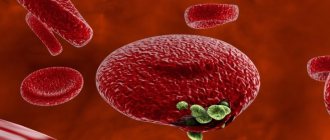
- In response to hypoxia, blood cells that carry hemoglobin and erythrocytes change. Their number increases simultaneously with platelets. Favorable conditions for thrombus formation are created and blood viscosity increases.
All taken together leads to increased load on the right ventricle, hypertrophy, and then failure of the right heart. An enlarged right atrioventricular orifice contributes to insufficient closure of the tricuspid valve.
Diagnosis of pathology
The diagnosis of cardiopulmonary failure is established based on the results of a comprehensive examination. During the initial examination, the doctor collects anamnesis (listens about symptoms, chronic pathologies in the patient and immediate family), performs a visual examination (possible swelling of the feet and legs), conducts a physical examination and standard measures (measuring blood pressure, listening to breathing using a phonendoscope). Upon palpation, a cardiac impulse is detected, and upon percussion, an expansion of the boundaries of the region of the muscular organ, which is partially covered by the lungs, is detected.
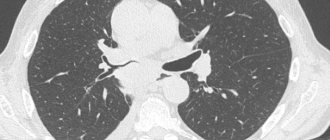
Among the laboratory diagnostic methods for making a diagnosis, an analysis of the gas composition of arterial blood is required. If there are problems, patients experience a decrease in P02 and SAO2 P02, and an increase in PC02. Additionally, a general blood test is prescribed to detect an infectious process in the body (by increasing the level of leukocytes). The most informative ways to detect cardiopulmonary failure are instrumental diagnostic methods. Depending on the symptoms, the patient may be prescribed:
- study of respiratory function (external respiration function). With the help of this examination, it is possible to establish the nature and severity of pulmonary ventilation impairment;
- electrocardiography (ECG). This is an accessible method that does not require additional preparation from the patient. The essence of electrocardiography is to record the electrical potentials of a muscle organ, which makes it possible to detect changes in rhythm and electrolyte deficiency. If the disease occurs in an acute form, it is possible to detect signs of overload in the right parts of the muscular organ. If the disease is chronic, it is possible to detect markers (both direct and indirect) of right ventricular hypertrophy;
- echocardiography (EchoCG). It is often prescribed in addition to an ECG, since the information content of this examination regarding cardiopulmonary failure is very high. This is the main non-invasive method with which it is possible to assess intracardiac hemodynamics, determine the size of the cavities of the muscular organ and the degree of pulmonary hypertension. EchoCG allows you to detect a number of possible disturbances in the functioning of the heart, differentiate it from heart disease and other pathologies;
- chest x-ray. This is a simple technique with which it is possible to assess the condition of the respiratory system (detect damage to the internal organ and notice signs of pulmonary hypertension);
- transbronchial lung biopsy. These methods are rarely resorted to, in particularly advanced clinical cases. A puncture biopsy of the lung is performed under ultrasound or X-ray guidance using a local anesthetic.
Treatment
Cor pulmonale is difficult to treat. The main measure is to eliminate the cause, thereby slowing down the progression or reducing hypoxia. If the patient has peripheral edema, the doctor prescribes diuretics. But they have the desired effect only if there is insufficiency of the left ventricle and, at the same time, overload of the lungs with fluid.
Diuretics can cause worsening of the condition, because even a slight decrease in preload can cause worsening of the manifestations of cor pulmonale. Pulmonary vasodilators do not produce results in cor pulmonale , although they are relevant for the treatment of primary pulmonary hypertension (calcium channel blockers, hydralazine, prostacyclin and dinitrogen oxide).
Digoxin gives the desired effect only if there is concomitant left ventricular dysfunction. This medication is prescribed with caution because patients diagnosed with COPD are extremely sensitive to the effects of digoxin. With hypoxic cor pulmonale, some doctors have suggested performing a venotomy, but the effect of reducing blood viscosity cannot cancel out the negative consequences of reducing the volume of blood that carries oxygen, with the exception of cases of polycythemia major. In patients with chronic cor pulmonale, long-term use of anticoagulants reduces the risk of venous thromboembolism.
Symptomatic treatment includes the use of:
- mucolytic agents
- bronchodilators
- oxygen therapy
- respiratory analeptics
If cor pulmonale is decompensated against the background of bronchial obstruction, the patient is prescribed constant use of drugs from the glucocorticoid group (for example, prednisolone may be effective). If, in the chronic form of cor pulmonale, the patient experiences a persistent increase in blood pressure, aminophylline can be prescribed (orally, intravenously or rectally); at the onset of the disease, nifedipine (Corinfar, Adalat) can be prescribed. In case of decompensated course, nitrates (nitroglycerin, nitrosorbide) are prescribed; monitoring of blood gas composition is mandatory, because there is a danger of worsening hypoxemia.
For symptoms of heart failure with cor pulmonale, cardiac glycosides and diuretics are prescribed. Caution must be exercised because glycosides have a highly toxic effect on the myocardium, especially under conditions of hypoxia and hypokalemia. Hypokalemia can be corrected with potassium supplements, such as potassium chloride or panangin. If diuretics are prescribed, first of all consider potassium-sparing drugs, including aldactone, triampur, etc.
In cases of severe erythrocytosis, bloodletting of 200-250 ml of blood is performed, after which low-viscosity infusion solutions, for example, rheopolyglucin, are administered intravenously. Also, therapy for cor pulmonale will include prostaglandins, especially those with antiproliferative, cytoprotective, and antiaggregation effects.
In some cases, endothelin receptor antagonists are relevant. Endothelin is a powerful vasoconstrictor of endothelial origin, the level of which increases in various forms of cor pulmonale. If acidosis develops, intravenous infusion of sodium bicarbonate solution is necessary. Treatment of circulatory failure of the right ventricular type is carried out with potassium-sparing diuretics, for example, veroshpiron or triamterene. Cardiac glycosides are effective for the treatment of left ventricular failure. In order to improve the metabolism of the heart muscle in cor pulmonale, it is recommended to prescribe mildronate (0.25 g 2 times a day orally), as well as potassium orotate or panangin (asparkam).
Therapy for cor pulmonale, as already noted, must be comprehensive (not only medications are used). The following methods are effective:
- massage
- physiotherapy
- hyperbaric oxygen therapy
- breathing exercises
Disease prevention
In order to prevent pathology, all risk factors that can provoke it should be eliminated. If any negative symptoms appear, it is important to consult a doctor in order to promptly diagnose and treat lung or heart disease. Also, experts recommend leading a healthy lifestyle (not smoking or drinking alcohol), engaging in moderate physical activity and eating right. The diet should be balanced with a predominance of fresh vegetables and fruits.
In order to prevent the development of acute cor pulmonale, patients diagnosed with varicose veins and atrial fibrillation are prescribed indirect anticoagulants. If there are blood clots in the veins, a vena cava filter is often installed. It is a small device that is installed into the lumen of the inferior vena cava. With its help, detached blood clots do not enter parts of the heart muscle and the pulmonary artery system.
Classification
Today there are several classifications, including such authors as B. E. Votchal (pulmonary heart disease) and N. R. Paleev (pulmonary hypertension in COPD). They are successfully combined, and three stages are distinguished.
- Stage I - transient - an increase in pulmonary arterial pressure is observed during physical activity, often the condition is caused by an exacerbation of the inflammatory process in the lungs or worsening bronchial obstruction
- Stage II - stable - pulmonary arterial hypertension is now observed not only during exercise, but also at rest, and is not associated with exacerbations of pulmonary pathology
- Stage III - pulmonary hypertension is stable, circulatory failure also develops