Published: 10/22/2021 15:15:00 Updated: 10/25/2021
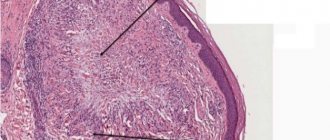
Sore throat is a disease of an infectious nature, manifested by acute inflammation of the lymphoid tissue of the pharynx. Most often the process affects the palatine tonsils, but other structures of the lymphadenoid pharyngeal ring can also be affected - the lingual and pharyngeal tonsils, lateral ridges or granules of the posterior pharyngeal wall.
The pathology in question is characterized by symptoms of intoxication, increased general temperature, sore throat that worsens during swallowing, enlarged and painful cervical lymph nodes. The palatine tonsils and arches are swollen, enlarged, bright red, and may have a white or dirty yellow coating.
Treatment of sore throat includes local treatment with antiseptics, painkillers and anti-inflammatory drugs, antibiotic therapy and detoxification measures. If complications develop or the process becomes chronic, surgical intervention may be required.
Causes of sore throat
Most often, inflammation is caused by the activity of beta-hemolytic streptococcus group A. Among the possible causative agents of the disease are also adenovirus, staphylococci, pneumococci, parainfluenza virus, mycoplasma, chlamydia, rhinovirus, respiratory syncytial virus, spirochete, Epstein-Barr virus, diphtheria bacillus, enterovirus Coxsackie B, fungi.
The risk of developing a sore throat increases when exposed to the following factors:
- general or local hypothermia;
- weakened immunity due to acute respiratory infections;
- fungal diseases;
- chronic pathologies of the nasopharynx, difficulty in nasal breathing, purulent processes and inflammation in the paranasal sinuses;
- caries;
- systematic exposure to irritating substances on the body, work in a smoky or dusty room;
- increased air dryness;
- regular drinking of alcohol, smoking;
- acute and chronic intoxication;
- poor nutrition, lack of vitamins in the diet.
Types and symptoms of sore throat
Depending on the cause, angina may be primary if the site of inflammation is initially localized in the tonsils.
A secondary or symptomatic type of pathology is considered a manifestation of another disease - infectious mononucleosis, diphtheria, scarlet fever, tularemia, typhoid fever, leukemia, alimentary-toxic aleukia, agranulocytosis. Inflammatory damage to the palatine tonsils is called tonsillitis, and to the nasopharyngeal tonsils - adenoiditis. There is also tonsillitis of the lingual tonsil, lateral ridges of the pharynx and laryngeal tonsillitis.
Based on the depth and nature of inflammation of the lymphoid tissue, the following forms of the disease are distinguished:
- catarrhal;
- lacunar;
- follicular;
- ulcerative-membranous;
- necrotic;
- combined.
Characteristic manifestations of any form of angina are general symptoms of intoxication, including increased body temperature, weakness, decreased appetite, headache, as well as enlarged and painful regional lymph nodes.
The incubation period depends on the type of pathogen and the state of immunity, ranging from several hours to a week or more. Other signs of angina, such as sore throat and external changes in the tonsils, may have varying severity depending on the form of the disease.
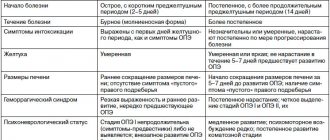
Catarrhal
The inflammatory process primarily involves the mucous membrane of the tonsils.
The disease begins acutely. The temperature during catarrhal tonsillitis rises within 37.1-38.0 °C, symptoms of intoxication and sore throat during swallowing are moderate. Characterized by enlargement of the lymph nodes located in front of the sternocleidomastoid muscle at the level of the angle of the lower jaw. The palatine tonsils are moderately swollen, their mucosa, as well as the surface of the palatine arches and the soft palate, are brightly hyperemic. The duration of the disease is 2-3 days, after which recovery occurs or a transition to a more severe form occurs.
Viral sore throat occurs with symptoms of ARVI - runny nose, cough. When infected with Coxsackie enterovirus, blistering rashes are observed on the mucous membrane of the palate and tonsils.
Lacunar and follicular
The clinical course of both lacunar and purulent tonsillitis is severe.
Characterized by fever from 38.0 to 40.0 °C, severe intoxication syndrome: headache, general weakness, aches in joints and muscles, pain in the projection of the heart, chills, sleep and appetite disturbances. The pain in the throat during swallowing is sharp, often radiating to the ear. Severe inflammatory changes lead to dysphonia - the voice takes on a nasal tone. Swelling of the tonsils may be accompanied by difficulty breathing and temporary hearing loss. When a child has a sore throat, there may be increased salivation, drowsiness, vomiting, convulsions, and abnormal bowel movements. In the first 2-4 days, the symptoms increase rapidly, and then disappear just as quickly. In the lacunar form of the disease, in addition to swelling and pronounced redness of the mucous membrane, white, irregularly shaped overlays with a yellowish tint appear on the tonsils, which can be easily removed with tweezers. In the case of follicular tonsillitis, suppuration of the follicles occurs; individual pinpoint yellowish formations of regular shape, no larger than a pinhead, appear through the epithelium. The tongue is dry, covered with a white coating. On the 4-5th day, the surface of the lacuna begins to clear, and the purulent blisters gradually disappear.
Necrotic
The most severe form of the disease. A pronounced intoxication syndrome is characterized by persistent fever, impaired consciousness, and repeated vomiting that does not bring relief. Dirty yellow spots with a greenish tint, ulcers and ulcers appear on the surface of the tonsils.
Ulcerative-membranous
Simanovsky-Plaut-Vincent angina is caused by a spirochete and a spindle-shaped rod that constantly live in the oral cavity.
With exhaustion, a pronounced decrease in immunity or hypovitaminosis, opportunistic microorganisms can become active, causing inflammation. The difference between ulcerative membranous tonsillitis and other forms is the one-sidedness of the process. An ulcer with a gray-yellow coating on the surface appears on the tonsil mucosa. Characterized by a putrid odor from the mouth, moderate sore throat and enlarged regional lymph nodes on the same side as the inflammation. Symptoms of intoxication may be absent or mild. The duration of the disease is from 7 to 12 days. After cleansing of plaque, the ulcerative defect heals without scar formation. Extensive ulcerations can lead to bleeding, damage to the periosteum, and perforation of the palate.
Antibiotics in the treatment of tonsillar pathology
A.I. KRYUKOV, Doctor of Medical Sciences, Professor, N.L. KUNELSKAYA
, Doctor of Medical Sciences, Professor,
G.Yu.
TSARAPKIN , Doctor of Medical Sciences,
A.S.
TOVMASYAN , Ph.D.,
O.A.
KISELEV ,
Research Clinical Institute of Otorhinolaryngology named after.
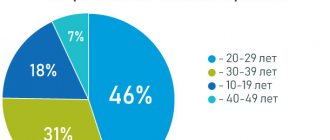
L.I. Sverzhevsky Department of Health, Moscow Tonsillar pathology is one of the most common pathologies throughout the world. People of all ages are susceptible to it, but inflammatory diseases of the tonsils are most relevant in childhood due to the risk of severe complications. Algorithms for the treatment of tonsillar pathology are described in various international and national guidelines, however, the practical choice of antimicrobial agents often causes difficulties for practitioners.
Up to 80% of acute and exacerbations of chronic respiratory diseases are accompanied by the symptom of sore throat, which is one of the most common reasons for patients to visit a pediatrician, therapist, otolaryngologist and doctors of other specialties. Acute inflammation of the pharynx is the cause of 1.1% of the total number of patient visits to doctors; 6% of all visits to the pediatrician; acute tonsillopharyngitis is among the 20 most frequently diagnosed diseases [1, 2]. In this case, sore throat can be a dominant problem, inevitably affecting the patient’s quality of life [3]. The relevance of the tonsillar problem is determined not only by the high prevalence of the disease, but also by the significant risk of developing associated systemic diseases, such as acute rheumatic fever, bacterial endocarditis, glomerulonephritis, toxic shock, etc.
In domestic practice, in case of acute infection involving the tonsils, the term “tonsillitis” or “tonsillitis” is usually used, and inflammation of the lymphoid follicles of the posterior pharyngeal wall is usually characterized by the term “pharyngitis”. In clinical practice, a combination of tonsillitis and pharyngitis is often observed, especially in childhood, therefore in the literature, especially in English, the term “tonsillopharyngitis” is widely used, suggesting inflammation of the walls of the oropharynx. In particular, the development of bacterial tonsillitis is often caused by an infection caused by beta-hemolytic streptococcus group A (GABHS), pharyngitis is usually caused by respiratory viruses, adenoiditis by viruses, Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Moraxella catarrhalis
, epiglottitis -
H. influenzae
.
Acute tonsillitis is classified into primary (banal) tonsillitis (catarrhal, follicular, lacunar, mixed, phlegmonous), secondary, arising from infectious diseases (scarlet fever, measles, diphtheria, syphilis, etc.), from blood diseases (leukemia, agranulocytosis, monocytosis), atypical (Simanovsky - Plaut - Vincent, viral, fungal). In clinical practice, the most common epidemic form of the disease is when the infection is transmitted by airborne droplets or contact and causes primary sore throats. In childhood, up to 30% of sore throats are bacterial in nature; in the vast majority of cases, the etiological factor is GABHS. Much more often, the development of acute tonsillitis is caused by a viral infection, primarily adenoviruses, respiratory syncytial viruses, and the Epstein-Barr virus. Viral forms of acute tonsillitis predominantly occur in the autumn-winter period and predominate in children of the first 3 years of life (up to 90%), and over the age of 5 years the frequency of bacterial forms increases (up to 50%) [4]. Intracellular pathogens also play a significant role in the development of the disease in childhood - Mycoplasma pneumoniae, Chlamydia pneumoniae, which are inoculated in 10-24 and 5-21% of cases, respectively, and the entire pharyngeal epithelium is infected with chlamydia, which may cause the process to become chronic [5, 6 ].
It is believed that the development of sore throat occurs as a hyperergic allergic reaction, and the sensitization of the body is caused by a variety of microflora of tonsil lacunae and protein breakdown products, and the trigger for the development of the disease can be various factors of an exogenous or endogenous nature. An allergic factor can serve as a prerequisite for the occurrence of infectious and allergic diseases, such as rheumatism, glomerulonephritis, nonspecific infectious polyarthritis, which are quite often a complication of tonsillitis, especially induced by GABHS, since they have a high adhesive ability to the membranes of the mucous membranes, resistance to phagocytosis, emit numerous exotoxins that cause a strong immune response contain antigens that cross-react with the myocardium, and the immune complexes that include them are involved in kidney damage [7, 8].
Treatment of acute tonsillitis and pharyngitis is complex and includes irrigation therapy, the use of local antibacterial drugs and systemic antibiotics.
With the viral etiology of tonsillitis and pharyngitis, it is possible to limit oneself to the prescription of irrigation therapy and local antiseptics, however, the bacterial etiology of the disease, especially GABHS, requires the mandatory use of systemic antibiotics.
In this regard, it is extremely important to follow the principles of rational antibacterial therapy, namely: prescribing the drug with the aim of maximizing clinical and bacteriological recovery; the spectrum of action of the drug must correspond to the probable causative agent of the infection, overcome possible resistance mechanisms and create a maximum concentration at the site of infection. What is especially important in pediatric practice is that the prescribed drug should be easy to use.
Adequate interpretation of the leading etiological factor (bacteria, viruses, fungi, protozoa), the clinical form of tonsillitis (primary or secondary), the severity of the disease (in acute tonsillitis there is usually one pathogen, in exacerbation of chronic tonsillitis - a mixed flora) [9] make it possible to prescribe therapy empirically, with taking into account information about sensitivity to antibiotics, the ability of the drug to create adequate concentrations at the site of infection and the proven effectiveness and safety of its use.
Traditionally, the drugs of choice for GABHS tonsillitis are semi-synthetic broad-spectrum penicillins. They are effective against the most likely pathogens of tonsillitis (GABHS), belong to a safe group of antibiotics, and all have oral forms. With a typical picture of the disease, they are considered as the drugs of choice.
The most famous representative of this group is amoxicillin, which has a pronounced bactericidal effect. The mechanism of action of the drug is associated with inhibition of the synthesis of peptidoglycan (a substance that is the basis of the bacterial membrane), which leads to disruption of the integrity of bacterial cell membranes and their death. Amoxicillin is active against strains of Staphylococcus spp. and Streptococcus spp.
., as well as
Neisseria meningitidis, Neisseria gonorrhoeae, Escherichia coli, Salmonella spp., Shigella spp., Klebsiella spp.
Therapeutic concentrations of amoxicillin are maintained in plasma for 8 hours after oral administration. Amoxicillin is rapidly absorbed from the digestive tract and reaches peak plasma concentrations within 1-2 hours after administration. Food intake has virtually no effect on the bioavailability and rate of absorption of amoxicillin. The active component is stable in the acidic environment of the stomach. High concentrations of the active substance are created in bronchial secretions, sputum, blood plasma, peritoneal and pleural fluid, as well as in lung tissue. Concentrations of amoxicillin in tissues and biological fluids are proportional to the dose taken.
During the metabolism of amoxicillin, pharmacologically inactive substances are formed. About 50-70% of the dose taken is excreted unchanged by the kidneys, about 10-20% by the liver, the rest of amoxicillin is excreted in the form of metabolites. Amoxicillin produced in Russia, Amosin (JSC Sintez, Kurgan), is currently available. The drug is intended for oral use. Capsules are taken before or after meals at regular intervals. As a rule, adults and children over 10 years of age (with a body weight of more than 40 kg) are prescribed 500 mg of amoxicillin three times a day. In severe cases of the disease, the dose of amoxicillin is increased to 750-1,000 mg three times a day. For children from 5 to 10 years of age, the therapeutic dose is 250 mg of amoxicillin three times a day. The average course of therapy lasts from 5 to 12 days (as a rule, therapy is continued for 2-3 days after the disappearance of clinical manifestations of the disease).
However, it should be taken into account that H. influenzae
, as well as
M. catarrhalis
are active producers of β-lactamases. This dictates the need to use protected aminopenicillins as initial therapy drugs, which are rightfully considered the “gold standard” for the treatment of acute purulent-inflammatory pathology of the ENT organs. One of the most commonly used antibiotics in the treatment of tonsillar pathology is a combination drug containing semisynthetic penicillin - amoxicillin and an irreversible lactamase inhibitor - clavulanic acid. Amoxicillin clavulanate is represented on the market by a number of trade names, among which the Russian drug Arlet® can be distinguished. Clavulanic acid, due to the presence of a β-lactam ring in its structure, forms stable complexes with bacterial lactamases and protects amoxicillin from destruction by these enzymes. This combination of components ensures high bactericidal activity of the drug. Arlet® is active against both amoxicillin-sensitive microorganisms and strains producing β-lactamases:
• gram-positive aerobes: Streptococcus pneumoniae
, GABHS,
Staphylococcus aureus
(except methicillin-resistant strains),
S. epidermidis
(except methicillin-resistant strains),
Listeria spp., Enteroccocus spp.;
• gram-negative aerobes:
Bordetella pertussis, Brucella spp., Campylobacter jejuni, Escherichia coli, Gardnerella vaginalis, Haemophilus influenzae, H. ducreyi, Klebsiella spp., Moraxella catarrhalis, Neisseria gonorrhoeae, N. meningitidis, Pasteurela multocida, Proteus spp., Salmonella spp. ., Shigella spp., Vibrio cholerae, Yersinia enterocolitica
;
• anaerobes: Peptococcus spp., Peptostreptococcus spp., Clostridium spp., Bacteroides spp., Actinomyces israelii
.
The pharmacokinetics of amoxicillin and clavulanic acid have many similarities. Both components are well absorbed from the gastrointestinal tract; food intake does not affect the degree of their absorption. Peak plasma concentrations are reached approximately one hour after taking the drug. Amoxicillin and clavulanic acid are characterized by good distribution in body fluids and tissues, creating therapeutic concentrations in areas of upper respiratory tract infections (tonsils, pharyngeal mucosa, paranasal sinuses, tympanic cavity, etc.). Amoxicillin is excreted unchanged from the body by the kidneys through tubular secretion and glomerular filtration. Clavulanic acid is eliminated through glomerular filtration, partially in the form of metabolites. Small amounts may be excreted through the intestines and lungs. The half-life is 1–1.5 hours. In patients with severe renal failure, the half-life of amoxicillin increases to 7.5 hours, clavulanic acid - to 4.5.
Amoxicillin/clavulanate is well tolerated. Adverse events are relatively rare and include diarrhea, nausea and skin rash. Arlet® tablets should be taken orally, without chewing, during meals, with a small amount of water. For adults and children over 12 years of age (or with a body weight of more than 40 kg), the usual dose for mild to moderate infections is 1 tablet of 250/125 mg 3 times a day. For severe infections, a tablet of 500/125 mg is prescribed 3 times a day; if necessary, tablets of the drug Arlet® are prescribed at a dose of 875/125 mg or 1 tablet of 500/125 mg 3 times a day. The course of treatment lasts up to 5-14 days. The duration of treatment is determined by the attending physician. Treatment should not continue for more than 14 days without repeated medical examination.
For atypical manifestations of the disease (mycoplasma and chlamydophilic infections), macrolides are the drugs of choice. They are recommended for use in children as initial therapy in the treatment of atypical forms of tonsillitis, as well as in cases where there is intolerance to beta-lactam antibiotics. Macrolides are considered as alternative antibacterial agents that can be prescribed in the event of a lack of effect from initial therapy, with the development of side and undesirable events associated with the use of first-line drugs [10, 11].
Literature
1. Nash DR, Harman J, Wald ER, Kelleher KJ. Antibiotic prescribing by primary care physicians for children with upper respiratory tract infections. Arch Pediatr Adolesc Med 2002. 156. 11: 1114-1119. 2. Panasiuk L, Lukas W, Paprzycki P. Empirical first-line antibioticotherapy in adult rural patients with acute respiratory tract infections. Ann Agric Environ Med 2007. 14. 2: 305-311. 3. Babiyak V.I., Govorukhin M.I., Mitrofanov V.V. Some psychological aspects of the problem of human “quality of life”. Russian Otorhinol., 2004. 1(8): 3-6. 4. Tatochenko V.K., Bakradze M.D., Darmanyan A.S. Acute tonsillitis in childhood: diagnosis and treatment. Farmateka, 2009. 14: 65-69. 5. Garashchenko T.I., Strachunsky L.S. Antibacterial therapy of ENT diseases in childhood. In the book: Pediatric otorhinolaryngology: A guide for doctors. Ed. M.R. Bogomilsky, V.R. Chistyakova. T. II. M.: Medicine, 2005: 275-317. 6. Linkov V.I., Tsurikova G.P., Nuralova I.V., Pankina N.A. The significance of chlamydial infection in the development of chronic inflammatory diseases of the pharynx. News of otolaryngology and speech pathology, 1995. 3(4): 146-146. 7. Kryukov A.I. Clinic, diagnosis and treatment of tonsillar pathology (Manual for doctors). M., 2011. 32 p. 8. Luchikhin L.A. Angina. Otorhinolaryngology: national guidelines. Ed. V.T. Palchuna. M.: GEOTAR-Media, 2008: 652–673. 9. Garashchenko T.I. Macrolides in the treatment of acute tonsillitis and its complications in children. RMJ, 2001. 9., 19: 812-816.
Source
: Medical Council, No. 11, 2015
Complications of sore throat
During the disease, the infection can spread to neighboring organs, causing otitis media, lymphadenitis, sinusitis, and peritonsillitis. Among the local purulent complications of tonsillitis, one can note the formation of an abscess or phlegmon in the inflamed tissues. Their occurrence is accompanied by a new wave of fever, increasing sore throat, problems with swallowing and breathing. In the case where the pathology is caused by streptococcus, 3-4 weeks after clinical recovery, glomerulonephritis, reactive arthritis or rheumatic carditis may develop due to subsequent autoimmune processes.
Diagnosis of sore throat
At the patient’s initial visit, the doctor collects complaints and anamnesis, specifying the duration and circumstances of the onset of symptoms, and the nature of the pain.
This is followed by a general examination of the patient, a visual assessment of the mucous membranes of the mouth and throat, and palpation of regional lymph nodes. An endoscopic examination of the ENT organs – pharyngoscopy – is mandatory. It allows you to examine the tonsils in detail and thus determine the form of the disease. For angina, the following tests are prescribed:
- Clinical blood test. Inflammation is indicated by neutrophilic leukocytosis with a shift to the left and accelerated ESR.
- General urine analysis. It is possible that protein may appear in the biomaterial.
- Rapid test from the tonsils using diagnostic strips to detect group A beta-hemolytic streptococcus.
- Bacteriological examination of a smear for beta-hemolytic streptococcus and diphtheria. Material is collected from the surface of the palatine tonsils and the posterior wall of the oropharynx before using local antiseptic drugs and taking antibiotics.
- If a patient is suspected of having infectious mononucleosis, a blood test is performed to test for IgM antibodies or to identify the genetic material of the Epstein-Barr virus.
- As part of the diagnosis of herpetic sore throat, enterovirus RNA is determined in the blood and throat smear using the PCR method.
Diagnosis of complications of angina after clinical recovery includes the following laboratory and instrumental studies:
- Control general analysis of blood and urine.
- Rheumatic test. Determination of rheumatoid factor, C-reactive protein, antistreptolysin-O, seromucoid in the blood.
- ECG. The electrocardiogram may show signs of hypoxia and conduction disturbances.
Sources
- Clinical recommendations (treatment protocol) for the provision of medical care to children with tonsillitis (acute streptococcal tonsillitis) FSBI NIIDI FMBA RUSSIA, State Budgetary Educational Institution of Higher Professional Education Krasnoyarsk State Medical University named after. prof. V.F. Voino-Yasenetsky, Ministry of Health of the Russian Federation, Municipal Budgetary Institution of the City Children's Clinical Hospital No. 1 (Krasnoyarsk).
- Modern possibilities of antibacterial therapy in children with chronic tonsillitis. / E.P. Karpova, M.P. Bozhatova. // Russian. Medical journal. – 2010. – T. 18, No. 1. – P. 8-10.
- Acute tonsillitis in childhood: diagnosis and treatment. /VC. Tatochenko, M.D. Bakradze, A.S. Darmanyan. // Pharmateka. - 2009. - No. 14. - P. 65-69.
Treatment of sore throat
Depending on the severity of the patient’s condition, treatment of angina occurs under the supervision of a doctor at home or in a hospital.
Bed rest is mandatory, a gentle dairy-vegetable diet enriched with vitamins, and plenty of warm drinks are recommended. For bacterial sore throat, broad-spectrum antibiotics are prescribed. If the disease is caused by streptococcus, penicillin drugs are used. In case of severe intoxication syndrome, intravenous infusion of glucose-saline solutions is performed. Non-steroidal anti-inflammatory drugs are used as antipyretics and pain relievers.
For sore throat, gargling with alkaline and water-salt solutions and irrigating the pharynx with painkillers and antiseptics are recommended. The use of drugs in the form of a spray for the treatment of sore throat is possible only in adults and children over 3 years of age. With the development of purulent complications of the disease, hospitalization of the patient followed by surgical intervention is required.
Author:
Pugonina Tatyana Alekseevna, Therapist
General information about the disease
With this type of sore throat, inflammation of the follicles of the palatine tonsils occurs. A follicle is a collection of lymphatic cells that look like small tubercles. It is in them that the protective cells of the immune system - leukocytes - are produced.
The main function of the palatine tonsils is to protect the body of any person, both adults and children, from infection entering the lower respiratory tract. The tonsils are an organ of the immune system. As soon as contact occurs between pathogenic microorganisms and the surface of the tonsil, the follicles begin to intensively produce leukocytes, which are sent to fight the enemy agent. As soon as the enemy is defeated, the dead bacteria, along with the dead leukocytes, are eliminated from the body. But if, for a number of reasons, the immune system is weakened, the tonsils cease to fully perform their functions. The inflammatory process spreads to the palatine tonsils.
If inflammation affects the lacunae of the tonsils, we talk about lacunar angina, if the follicles of the tonsils - about follicular angina, respectively.