Azithromycin Forte-OBL tab.pp.o.500mg No. 3 103571
Indications
Infectious and inflammatory diseases caused by microorganisms sensitive to azithromycin: infections of the upper respiratory tract and ENT organs (sinusitis, tonsillitis, pharyngitis, otitis media); infections of the lower respiratory tract (acute bronchitis, exacerbation of chronic bronchitis, pneumonia, including those caused by atypical pathogens); infections of the skin and soft tissues (acne vulgaris of moderate severity, erysipelas, impetigo, secondary infected dermatoses); uncomplicated urinary tract infections caused by Chlamydia trachomatis (urethritis and/or cervicitis); the initial stage of Lyme disease (borreliosis) is erythema migrans.
pharmachologic effect
An antibiotic of the macrolide group, a representative of the azalides. Has a wide spectrum of antimicrobial action. The mechanism of action of azithromycin is associated with the suppression of protein synthesis in microbial cells. By binding to the 50S ribosomal subunit, it inhibits peptide translocase at the translation stage, suppresses protein synthesis, and slows down the growth and reproduction of bacteria. In high concentrations it has a bactericidal effect.
It is active against a number of gram-positive, gram-negative, anaerobic, intracellular and other microorganisms.
Sensitive to azithromycin
gram-positive cocci: Streptococcus pneumoniae (penicillin-sensitive strains), Streptococcus pyogenes, Staphylococcus aureus (methicillin-sensitive strains); aerobic gram-negative bacteria: Haemophilus influenzae, Haemophilus parainfluenzae, Legionella pneumophila, Moraxella catarrhalis, Pasteurella multocida, Neisseria gonorrhoeae; some anaerobic microorganisms: Clostridium perfringens, Fusobacterium spp., Prevotella spp., Porphyriomonas spp.; as well as Chlamydia trachomatis, Chlamydia pneumoniae, Chlamydia psittaci, Mycoplasma pneumoniae, Mycoplasma hominis, Borrelia burgdorferi.
Microorganisms with acquired resistance
to azithromycin: aerobic gram-positive microorganisms - Streptococcus pneumoniae (penicillin-resistant strains and strains with intermediate sensitivity to penicillin).
Microorganisms with natural resistance:
aerobic gram-positive microorganisms - Enterococcus faecalis, Staphylococcus aureus, Staphylococcus epidermidis (methicillin-resistant strains), anaerobic microorganisms - Bacteroides fragilis.
Cases of cross-resistance
between Streptococcus pneumoniae, Streptococcus pyogenes (group A beta-hemolytic streptococcus), Enterococcus faecalis and Staphylococcus aureus (methicillin-resistant strains) to erythromycin, azithromycin, other macrolides and lincosamides.
Drug interactions
Simultaneous use of macrolide antibiotics, incl. azithromycin, with P-glycoprotein substrates such as digoxin, leads to increased concentrations of P-glycoprotein substrate in the blood serum. With the simultaneous use of digoxin or digitoxin with azithromycin, a significant increase in the concentration of cardiac glycosides in the blood plasma and the risk of developing glycoside intoxication are possible.
With simultaneous use of azithromycin with warfarin, cases of increased effects of the latter have been described.
Azithromycin interacts weakly with isoenzymes of the cytochrome P450 system.
Given the theoretical possibility of ergotism, the simultaneous use of azithromycin with ergot alkaloid derivatives is not recommended.
Concomitant use of atorvastatin (10 mg daily) and azithromycin (500 mg daily) did not cause changes in atorvastatin plasma concentrations (based on an HMC-CoA reductase inhibition assay). However, in the post-marketing period, isolated case reports of rhabdomyolysis have been received in patients receiving concomitant azithromycin and statins.
In pharmacokinetic studies of the effect of a single dose of cimetidine on the pharmacokinetics of azithromycin, no changes in the pharmacokinetics of azithromycin were detected when cimetidine was administered 2 hours before azithromycin.
Potentiation of the anticoagulant effect has been reported after simultaneous use of azithromycin and indirect anticoagulants (coumarin derivatives). The need for frequent monitoring of prothrombin time should be taken into account when using azithromycin in patients receiving indirect oral anticoagulants (coumarin derivatives).
Caution should be exercised when used concomitantly with cyclosporine. If concomitant use is necessary, monitor plasma concentrations of cyclosporine and adjust the dose accordingly.
It has been found that the simultaneous use of terfenadine and macrolides can cause arrhythmia and prolongation of the QT interval.
When used simultaneously with disopyramide, a case of the development of ventricular fibrillation has been described.
When used simultaneously with lovastatin, cases of rhabdomyolysis have been described.
When used simultaneously with rifabutin, the risk of developing neutropenia and leukopenia increases.
Dosage regimen
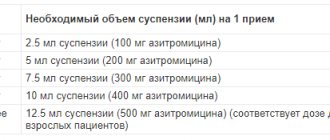
Inside. The dosage regimen is set individually, depending on the diagnosis, severity of the disease, the age of the patient and the dosage form used.
Contraindications for use
Hypersensitivity to azithromycin, erythromycin, other macrolides or ketolides; severe liver dysfunction; simultaneous use with ergotamine and dihydroergotamine; children up to 6 months of age (for the dosage form, powder for the preparation of a suspension); children under 3 years of age (for the dosage form of tablets 125 mg), children under 12 years of age with a body weight of less than 45 kg (for the dosage form of tablets 500 mg).
Carefully:
myasthenia gravis; mild to moderate liver dysfunction; end-stage renal failure with GFR less than 10 ml/min; patients with the presence of proarrhythmogenic factors (especially in old age) - with congenital or acquired prolongation of the QT interval, patients receiving therapy with antiarrhythmic drugs of classes IA (quinidine, procainamide) and III (dofetilide, amiodarone and sotalol), cisapride, terfenadine, antipsychotic drugs ( pimozide), antidepressants (citalopram), fluoroquinolones (moxifloxacin and levofloxacin), with water and electrolyte imbalance, especially with hypokalemia or hypomagnesemia, with clinically significant bradycardia, arrhythmia or severe heart failure; simultaneous use of digoxin, warfarin, cyclosporine.
Use in children
Contraindicated for use in children under 6 months of age (for the dosage form, powder for preparing a suspension); under 3 years of age (for the 125 mg tablet dosage form), under 12 years of age with a body weight of less than 45 kg (for the 500 mg tablet dosage form).
Restrictions for children
Use with caution
Use in elderly patients
In elderly patients, pro-arrhythmogenic conditions may be present; azithromycin should be used with caution due to the high risk of developing arrhythmias, incl. ventricular ar.
Restrictions for elderly patients
Use with caution
Use for liver dysfunction
Use is contraindicated in severe liver dysfunction.
Use with caution in mild to moderate liver dysfunction.
Restrictions for liver dysfunction
Use with caution
Use during pregnancy and breastfeeding
Use during pregnancy is possible only in cases where the expected benefit to the mother outweighs the potential risk to the fetus. If it is necessary to use azithromycin during lactation, the issue of stopping breastfeeding should be decided.
Restrictions when breastfeeding
Contraindicated
Restrictions during pregnancy
Use with caution
Use for renal impairment
Use with caution in patients with end-stage renal failure with GFR less than 10 ml/min.
Restrictions for impaired renal function
Use with caution
special instructions
Use with caution in patients with mild to moderate liver dysfunction due to the possibility of developing fulminant hepatitis and severe liver failure. If there are symptoms of liver dysfunction, such as rapidly increasing asthenia, jaundice, darkening of urine, bleeding tendency, hepatic encephalopathy, azithromycin therapy should be discontinued and a study of the functional state of the liver should be performed.
As with the use of other antibacterial drugs, during therapy with azithromycin, patients should be regularly examined for the presence of non-susceptible microorganisms and signs of the development of superinfections, incl. fungal.
Azithromycin should not be used for longer courses than indicated in the instructions, because The pharmacokinetic properties of azithromycin allow us to recommend a short and simple dosage regimen.
With long-term use of azithromycin, the development of pseudomembranous colitis caused by Clostridium difficile, both in the form of mild diarrhea and severe colitis, is possible. If antibiotic-associated diarrhea develops during the use of azithromycin, as well as 2 months after the end of therapy, pseudomembranous colitis caused by Clostridium difficile should be excluded. Drugs that inhibit intestinal motility are contraindicated.
When treated with macrolides, incl. azithromycin, prolongation of cardiac repolarization and QT interval was observed, increasing the risk of developing cardiac arrhythmias, incl. ari.
The use of azithromycin may provoke the development of myasthenic syndrome or cause an exacerbation of myasthenia gravis.
There have been isolated cases of serious allergic reactions, including angioedema and anaphylaxis (rarely fatal), dermatological reactions, including acute generalized exanthematous pustulosis, Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, drug rash with eosinophilia and systemic manifestations (DRESS- syndrome). Some of the reactions were recurrent and required longer monitoring and treatment.
Impact on the ability to drive vehicles and machinery
With the development of undesirable effects on the nervous system and organ of vision, patients should be careful when performing actions that require increased concentration and speed of psychomotor reactions.
Side effect
From the hematopoietic system:
uncommon - leukopenia, neutropenia, eosinophilia; very rarely - thrombocytopenia, hemolytic anemia.
Allergic reactions:
rarely - skin rash, angioedema and anaphylaxis (in rare cases with fatal outcome), erythema multiforme, drug rash with eosinophilia and systemic manifestations (DRESS syndrome). Some of these reactions that developed during the use of azithromycin acquired a recurrent course and required long-term treatment and observation.
For the skin and subcutaneous tissues:
uncommon - skin rash, itching, urticaria, dermatitis, dry skin, sweating; rarely - photosensitivity reaction; frequency unknown - Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme.
From the nervous system:
often - headache; infrequently - dizziness, disturbance of taste, paresthesia, drowsiness, insomnia, nervousness; rarely - agitation; frequency unknown - hypoesthesia, anxiety, aggression, fainting, convulsions, psychomotor hyperactivity, loss of smell, perversion of smell, loss of taste, myasthenia gravis, delirium, hallucinations.
From the side of the organ of vision:
infrequently - visual impairment.
Hearing and labyrinth disorders:
uncommon - hearing loss, vertigo; frequency unknown - hearing impairment up to deafness and/or tinnitus.
From the cardiovascular system:
infrequently - palpitations, flushing of the face; frequency unknown - decreased blood pressure, increased QT interval on ECG, ari, ventricular tachycardia.
From the respiratory system:
infrequently - shortness of breath, nosebleeds.
From the digestive system:
very often - diarrhea; often - nausea, vomiting, abdominal pain; uncommon - flatulence, dyspepsia, constipation, gastritis, dysphagia, bloating, dry oral mucosa, belching, ulcers of the oral mucosa, increased secretion of the salivary glands; very rarely - change in tongue color, pancreatitis.
From the liver and biliary tract:
uncommon - hepatitis; rarely - impaired liver function, cholestatic jaundice; frequency unknown - liver failure (in rare cases with death, mainly due to severe liver dysfunction), liver necrosis, fulminant hepatitis.
From the musculoskeletal system:
uncommon - osteoarthritis, myalgia, back pain, neck pain; frequency unknown - arthralgia.
From the kidneys and urinary tract:
uncommon - dysuria, pain in the kidney area; frequency unknown - interstitial nephritis, acute renal failure.
From the reproductive system:
infrequently - metrorrhagia, testicular dysfunction.
Infectious diseases:
infrequently - candidiasis (including the mucous membrane of the oral cavity and genitals); frequency unknown - pseudomembranous colitis.
From the laboratory parameters:
often - a decrease in the number of lymphocytes, an increase in the number of eosinophils, an increase in the number of basophils, an increase in the number of monocytes, an increase in the number of neutrophils, a decrease in the concentration of bicarbonates in the blood plasma; infrequently - increased activity of AST, ALT, increased concentration of bilirubin in the blood plasma, increased concentration of urea in the blood plasma, increased concentration of creatinine in the blood plasma, change in the potassium content in the blood plasma, increased activity of alkaline phosphatase in the blood plasma, increased chlorine content in the blood plasma, increased blood glucose concentration, increased platelet count, increased hematocrit, increased plasma bicarbonate concentration, change in plasma sodium content.
Other:
uncommon - asthenia, malaise, anorexia, feeling of fatigue, facial swelling, chest pain, fever, peripheral edema.
Comparison of the effectiveness of Azithromycin forte-obi and Azithromycin-obi
The effectiveness of Azithromycin forte-obi is quite similar to Azithromycin-ob - this means that the ability of the drug substance to provide the maximum possible effect is similar.
For example, if the therapeutic effect of Azithromycin forte-obi is more pronounced, then using Azithromycin-obi even in large doses will not achieve this effect.
Also, the speed of therapy is an indicator of the speed of therapeutic action; Azithromycin forte-obi and Azithromycin-obi are approximately the same. And bioavailability, that is, the amount of a drug reaching its site of action in the body, is similar. The higher the bioavailability, the less it will be lost during absorption and use by the body.
Comparison of ease of use of Azithromycin forte-obi and Azithromycin-obi
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Azithromycin forte-obi is approximately the same as Azithromycin-obi. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2020-12-04 13:48:21
Comparison of side effects of Azithromycin forte-obi and Azithromycin-obi
Side effects or adverse events are any adverse medical event that occurs in a subject after administration of a drug.
Azithromycin forte-obi has almost the same side effects as Azithromycin-obi. They both have few side effects. This implies that the frequency of their occurrence is low, that is, the indicator of how many cases of an undesirable effect of treatment are possible and registered is low. The undesirable effect on the body, the strength of influence and the toxic effect of Azithromycin forte-obi are similar to Azithromycin-ob: how quickly the body recovers after taking it and whether it recovers at all.
Comparison of addiction between Azithromycin forte-obi and Azithromycin-obi
Like safety, addiction also involves many factors that must be considered when evaluating a drug.
Thus, the totality of the values of such parameters as “syndrome o” in Azithromycin-obi is less than the similar values in Azithromycin forte-obi. Withdrawal syndrome is a pathological condition that occurs after the cessation of intake of addictive or dependent substances into the body. And resistance is understood as initial immunity to a drug; in this it differs from addiction, when immunity to a drug develops over a certain period of time. The presence of resistance can only be stated if an attempt has been made to increase the dose of the drug to the maximum possible.