Chronic pain syndrome continues to be one of the important medical and social problems of modern society, since it significantly affects the functional activity and ability to work of patients, significantly maladjusts and reduces the quality of life of 15% to 40% of people in economically developed countries [1] and is associated with an increase in mortality and increased morbidity [2–6]. Neurological diseases are one of the leading causes of pain occurrence and chronicity.
Neuropathic pain (NP) is one of the common types of chronic pain syndrome [7], observed due to damage or disease of the central or peripheral somatosensory nervous system at any level and occurs in the population in 7–10% of cases [8]. NP is distinguished by a characteristic clinical pattern and variety of sensory manifestations and symptoms, greater intensity and duration of pain, a chronic and often relapsing course and is accompanied by a variety of comorbid pathological conditions, which ultimately forms a polymorphic picture of pain that is difficult to diagnose. At the same time, an analysis of the complaints, a history of damage or disease of the somatosensory nervous system, examination data of the patient, as well as the results of additional examination methods that objectively confirm damage to the somatosensory system, which can lead to the occurrence of NP, make it possible to identify this variant of the pain syndrome.
Basic principles of clinical diagnosis of NB [as amended. 9, 10]:
Listen carefully to how
the patient describes the pain - characteristic verbal characteristics: “burning”, “burning”, “shooting”, “electric shocks”, “tingling”, “numbness”, “burning”, etc.
During a neurological examination, pay attention to whether there is
The patient has characteristic sensitivity disturbances - a combination of “positive” (symptoms of irritation - hypesthesia, anesthesia, hypalgesia, analgesia) and “negative” (symptoms of loss - spontaneous pain, dysesthesia, paresthesia, allodynia, hyperalgesia) sensory phenomena.
When analyzing the pain syndrome , correlate
does the area of the pain being presented coincide with the identified sensory disturbances; the localization of the described pain syndrome corresponds to a certain neuroanatomical zone - the zone of innervation of the corresponding nervous structure.
A patient with chronic pain syndrome always presents a difficult clinical task for doctors, which is also due to the presence of various comorbid pathologies, in particular anxiety and depressive disorders, which negatively affect the effectiveness of the treatment and significantly reduce the compliance of this category of patients. Particularly difficult and “inconvenient” patients in this regard are patients with chronic NP, since this variant of the pain syndrome is diagnosed late, is less responsive to treatment, has a recurrent course, and only a few patients manage to completely relieve pain. In the vast majority of cases, patients with chronic NB have comorbid conditions and diseases that significantly aggravate the already painful existence of these patients [10].
The most effective and strategically justified in the management of patients with chronic NB is an integrated and multidisciplinary approach, which involves pharmacological therapy with drugs with proven effectiveness, non-drug treatment methods and treatment of comorbid disorders, especially anxiety, depressive symptoms and sleep disorders. Only if these areas of therapy are insufficiently effective, minimally invasive and surgical treatment methods are used. It should be noted that pharmacotherapy for chronic NP should be carried out long-term and continuously, taking into account nosology, comorbidity and the choice of the safest drug. Therapy should be started with minimal doses of the drug with gradual titration to therapeutically effective ones, tolerability analysis and parallel monitoring of side or undesirable effects should be carried out [11]. First-line therapy includes drugs from the group of anticonvulsants (gabapentin and pregabalin), selective serotonin and norepinephrine reuptake inhibitors (SNRIs) (duloxetine and venlafaxine) and tricyclic antidepressants (amitriptyline, nortriptyline and imipramine) [10].
When choosing a drug, it is important to take into account the pathogenetic mechanisms of the formation and maintenance of chronic pain syndrome, among which an undoubted and important role is played by the disturbed interaction of the nociceptive and antinociceptive systems and the phenomenon of disinhibition, observed with insufficient functional activity of descending antinociceptive influences. And the longer this pathological process exists and the more pronounced, the more excruciating the nature of recurrent pain can be observed in the patient [12]. The main mediators of the antinociceptive system are biogenic amines: endorphins, serotonin, norepinephrine and dopamine, therefore drugs that activate and normalize their metabolism thus enhance the functional activity of the antinociceptive system, which leads to a decrease in the intensity and frequency of pain. These are narcotic analgesics, tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs) and SNRIs, and it is the antidepressants from the SNRIs group that have proven to be effective and most promising for the treatment of patients with chronic pain syndrome. It should be noted that of the drugs from this group existing on the Russian market, duloxetine has a high affinity for norepinephrine receptors, which suggests greater effectiveness of this drug in the treatment of chronic pain [13]. Studies [14–16] have convincingly demonstrated the pronounced effect of duloxetine on the serotonergic and noradrenergic systems, which increases the functional activity of the descending pain suppression system and has an analgesic effect regardless of its antidepressant effect. That is why duloxetine, initially considered as an antidepressant [17], quickly began to be used in the treatment of chronic pain syndrome in a wide range of different diseases. Numerous clinical studies have shown a pronounced therapeutic effect of duloxetine in the treatment of patients with osteoarthritis [18–20], low back pain [19, 21–23], painful diabetic neuropathy [19, 24–28], fibromyalgia [19, 24] , as well as other diseases and pathological conditions accompanied by chronic pain [29–32].
Painful form of diabetic neuropathy
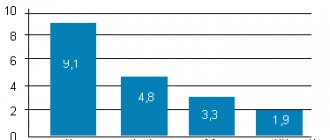
In the painful form of diabetic neuropathy, a number of pharmacological agents are used to treat chronic NP, the comparison of the effectiveness of which in one of the latest meta-analyses [24] of randomized controlled trials (RCTs) demonstrated a high result of duloxetine. The clinical efficacy of duloxetine has been convincingly demonstrated in a large number of studies of patients with chronic pain caused by diabetic neuropathy [19, 24–28, 30]. In particular, a Cochrane review of 8 studies of duloxetine at a daily dose of 60 mg in 2728 patients demonstrated its effect even with short-term therapy for 12 weeks. in the form of a reduction in pain severity by 50% or more (OR 1.73, 95% CI 1.44–2.08) [24]. However, side effects did not differ significantly from those in the placebo group, and no serious adverse reactions were observed [24]. In another multicenter 6-month comparative prospective study of the effectiveness of duloxetine, gabapentin and pregabalin, higher effectiveness in relieving pain, according to the Brief Pain Inventory (BPI), was found with duloxetine, as well as a significant decrease in severity when taking it. anxiety and depression, according to the Hospital Anxiety and Depression Scale (HADS) [25].
It should be noted that the analgesic effect of duloxetine develops much earlier than the antidepressant effect, as demonstrated in a multicenter, double-blind, placebo-controlled study of 348 patients with painful diabetic neuropathy in both types of diabetes mellitus; in addition, the drug had no effect on the control of diabetes mellitus and was good was tolerated [26]. The results obtained prove the significant influence of duloxetine on the main pathogenetic mechanisms of the formation of chronic pain - the processes of disinhibition, thus normalizing the descending control of pain, and not reducing the severity of the pain syndrome by treating only depressive disorders, which are almost obligately observed in patients with long-term pain syndrome. Patients should be informed about these features of duloxetine before starting therapy, which will improve adherence to this therapy and further doctor-patient relationships. It is important to note that most patients with diabetes have cardiovascular disorders, so the use of duloxetine is safer and preferable, in particular, compared to amitriptyline [26, 33].
Special instructions for the use of Duloxetine
Patients with a high risk of suicide during the treatment period should be under strict supervision, since before the onset of pronounced remission, the possibility of suicide attempts cannot be excluded. Duloxetine has not been studied in patients under 18 years of age and should not be used in this age group. As with other drugs that act on the central nervous system, duloxetine should be used with caution in patients with mania or a history of seizures. There have been reports of mydriasis in association with duloxetine, so duloxetine should be used with caution in patients with elevated intraocular pressure or at risk of developing acute narrow-angle glaucoma. Increased plasma concentrations of duloxetine have been reported in patients with severe renal impairment (creatinine clearance ≤30 mL/min) or severe hepatic impairment. It is recommended that such patients be given duloxetine at a lower initial dose. In some patients, taking duloxetine leads to an increase in blood pressure. In patients with hypertension (arterial hypertension) and/or other diseases of the cardiovascular system, it is recommended to monitor blood pressure. In clinical studies, an increase in the activity of liver enzymes in the blood was noted. In most patients receiving duloxetine, this increase was transient and disappeared after discontinuation of duloxetine treatment. Significant elevations in liver enzymes (more than 10 times normal) or liver damage with cholestasis, or significant increases in liver enzymes in combination with liver damage have occurred rarely and have been associated with alcohol abuse in some cases. Duloxetine did not have a mutagenic effect in experiments in vitro and in vivo . Adequate and controlled studies of the effects of duloxetine in pregnant women have not been conducted, therefore its use during pregnancy is not recommended. Duloxetine is excreted in breast milk. The approximate daily dose for an infant is 0.14% of the dose for a nursing woman (mg/kg). The safety of duloxetine in a nursing infant has not been established and breastfeeding while taking duloxetine is not recommended. During treatment with duloxetine, patients should refrain from potentially hazardous activities that require increased attention and speed of psychomotor reactions.
Chronic pain syndrome in the lower back
Pain in the lower back continues to be one of the most pressing problems of modern people and a common reason for visiting a doctor. Among patients with chronic low back pain (CLBP), signs of neuropathic pain are observed in an average of 37% of cases [21], however, the low diagnosis of LP observed in clinical practice suggests a much higher percentage of its presence.
Analysis of data from 4 multicenter, double-blind, randomized, placebo-controlled studies of duloxetine for the treatment of chronic headache disorder in 1295 patients at a daily dose of 60 mg for 12–14 weeks. showed the greatest effectiveness of this drug in the form of more patients who experienced a reduction in pain of 30% or more at the end of treatment relative to baseline (59.7% compared with 47.8% in the placebo group, p < 0.001), and also a greater reduction in pain severity - by 50% or more (48.6% compared to the placebo group 35.1%; p <0.001) [21]. It should be noted that these patients had minimal depressive disorders (low scores on the Beck Depression Rating Scale). It is important to note that the predictors of the greatest effectiveness of duloxetine, according to the researchers, were an early response to therapy - in the first 2 weeks. from its onset (improvement of at least 15%, according to the BPI questionnaire), use at a daily dose of 60 mg and the presence of pain in several areas [21]. It is interesting that other researchers, in addition to the early response when taking duloxetine at a daily dose of 60 mg, noted the occurrence of adverse reactions at the initial stage of therapy as a predictor of its further clinical effect in patients with CLBP [22].
Another analysis of data from 3 double-blind, placebo-controlled studies of the clinical use of duloxetine in patients with chronic LBP found that the significantly superior analgesic effect of duloxetine at a daily dose of 60 mg superior to placebo was associated with 91% of its direct analgesic effect and only 9% with an antidepressant effect. i.e., an indirect effect [23]. The results obtained prove the important role of duloxetine in the treatment of chronic pain (including NB), the use of which is aimed at restoring the functional activity of the descending noradrenergic and serotonergic antinociceptive systems, which leads to a decrease in the severity of pain, as well as anxiety, depressive disorders and sleep disturbances. In contrast, a systematic analysis of studies of the effectiveness of drugs in the treatment of patients with chronic LBP [34] found no difference in the analgesic effect between tricyclic antidepressants or SSRI drugs compared with placebo. In clinical practice, treatment of patients with chronic musculoskeletal pain, including CLBP, begins with a daily dose of 30 mg, after 7–10 days the dose is 60 mg, and a number of researchers, if necessary, increase the daily dose to 120 mg [23].
A meta-analysis of 9 RCTs [20] of the effectiveness and safety of duloxetine in the treatment of patients with chronic pain syndrome demonstrated not only its effect on the severity of pain, but also a significant improvement in the functional component, daily activity, emotional background and quality of life, and there was no statistically significant difference in serious adverse events of duloxetine compared with the placebo group.
All of these numerous studies led to the inclusion of duloxetine in the treatment algorithm for chronic LBP in the recommendations of the American College of Physicians [35].
Use of the drug Duloxetine
For depression and diabetic neuropathy, it is prescribed orally at a dose of 60 mg 1 time per day daily, regardless of meals. Some patients may be advised to take a higher dose (up to a maximum of 120 mg/day in 2 divided doses). The possibility of prescribing doses exceeding 120 mg/day has not been studied. The initial dosage for patients with end-stage renal failure (creatinine clearance ≤30 ml/min) is 30 mg once daily. Patients with liver cirrhosis are prescribed a lower initial dose or with longer intervals between doses. No dose adjustment of duloxetine is required in elderly or elderly patients. The effect of duloxetine has not been studied in patients under 18 years of age.
Chronic pain syndrome in osteoarthritis
Osteoarthritis (OA) is the most common joint disease, its leading manifestation is chronic pain, the clinical analysis of which often demonstrates characteristic sensory manifestations of NP [20]. OA of the knee joints is most often observed.
The results of a double-blind, placebo-controlled study [36] of the use of duloxetine in patients with chronic pain due to knee OA showed a significant reduction in pain severity and improvement in quality of life compared with placebo, regardless of which non-steroidal anti-inflammatory drugs (NSAIDs) were previously used . According to the researchers, duloxetine can be considered as an alternative to the use of NSAIDs for knee OA if their use is not indicated due to existing cardiovascular or other risks [37]. The effectiveness of duloxetine in relieving pain and improving function in OA was also supported by a systematic review of 4 randomized trials [20]. A meta-analysis of 3 RCTs [18] involving 1011 patients demonstrated a statistically significant effect of duloxetine on the level and frequency of OA pain, improvement in functional activity, and the absence of significant adverse or side effects compared with placebo after 10–13 weeks. therapy.
Another randomized, double-blind, placebo-controlled study [38] of patients with knee OA showed a significant reduction in pain, stiffness, functional impairment and improvement in quality of life when taking duloxetine for 14 weeks. The 2022 OARSI (Osteoarthritis Research Society International) guidelines [39] consider duloxetine as a treatment for knee OA in patients with widespread chronic pain and depressive disorders.
Side effects of the drug Duloxetine
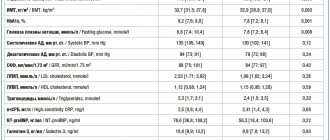
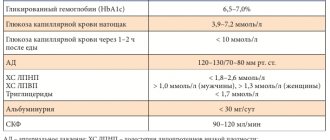
During clinical trials, side effects such as constipation, nausea, dry mouth, dizziness, fatigue, insomnia and headache (≥10%) were observed. Less commonly (with a frequency of ≤10%, but ≥1%) - tachycardia, dyspepsia, vomiting, loss of appetite, drowsiness, tremor, lethargy, sweating, feeling hot, yawning. From the reproductive system, disorders of ejaculation and erection were noted (with a frequency of ≤10%, but ≥1%), decreased libido and anorgasmia. Rarely (≤1%, but ≥0.1%) - gastroenteritis, stomatitis, increased blood pressure, weight gain, muscle tension, taste and vision disturbances, agitation, urinary retention. Treatment with duloxetine in placebo-controlled clinical trials was associated with nonsignificant increases in ALT, AST, and CK levels compared with placebo. In clinical trials of duloxetine for the treatment of diabetic neuropathy, the mean duration of diabetes mellitus was approximately 11 years, the mean initial fasting serum glucose concentration was up to 163 mg/dL, and the mean initial glycosylated hemoglobin concentration was 7.80%. In these studies, there was a nonsignificant increase in initial fasting blood glucose concentrations at 12 weeks in patients treated with duloxetine compared with placebo, followed by a usual regimen of 52 weeks. There were no changes in glycosylated hemoglobin, patient body weight, lipid concentrations (C, LDL, HDL, TG) or any side effects associated with diabetes. According to post-marketing studies, the following side effects were noted: on the part of the visual organ: very rarely (≤0.01%) - glaucoma; from the hepatobiliary system: very rarely (≤0.01%) - hepatitis, jaundice; from the immune system: very rarely (≤0.01%) - anaphylactic reactions; from laboratory parameters: very rarely (≤0.01%) - increased activity of ALT, AST, alkaline phosphatase, bilirubin level in the blood; from the metabolic side: very rarely (≤0.01%) - hyponatremia; from the skin: rarely (0.01–0.1%) - rash; very rarely (≤0.01%) - angioedema, Stevens-Johnson syndrome, urticaria; from the cardiovascular system: very rarely (≤0.01%) - orthostatic hypotension and syncope (especially at the beginning of treatment).
Duloxetine overdose, symptoms and treatment
Clinical data on duloxetine overdose are limited. There have been cases of drug overdose (up to 1400 mg), including in combination with other drugs, but they did not lead to death. In animal experiments, the main manifestations of toxicity in case of overdose were observed in the central nervous system and gastrointestinal tract. These included symptoms such as tremor, clonic seizures, ataxia, vomiting and anorexia. A specific antidote is not known. Immediately after an overdose, gastric lavage and the administration of activated charcoal are indicated. The airway must be kept open. It is recommended to monitor vital signs, primarily cardiac activity, and, if necessary, provide symptomatic and supportive therapy. Duloxetine has a large volume of distribution, and therefore forced diuresis, hemoperfusion and exchange perfusion are ineffective in case of overdose.
List of pharmacies where you can buy Duloxetine:
- Moscow
- Saint Petersburg
Drug interactions Duloxetine
Duloxetine should not be co-administered with MAO inhibitors or for at least 14 days after stopping treatment with MAO inhibitors. Given the half-life of duloxetine, MAO inhibitors should also not be administered for at least 5 days after stopping treatment with duloxetine. In clinical studies, with the simultaneous administration of theophylline, a CYP1A2 substrate, with duloxetine at a dose of 60 mg 2 times daily, no significant changes in their pharmacokinetics were observed. These results suggest that duloxetine is unlikely to have a clinically significant effect on the metabolism of CYP 1A2 substrates. Since CYP 1A2 is involved in the metabolism of duloxetine, concomitant use of duloxetine with active CYP 1A2 inhibitors may lead to increased plasma concentrations of duloxetine. Fluvoxamine (at a dose of 100 mg 1 time per day), being an active inhibitor of CYP 1A2, reduces the clearance of duloxetine from blood plasma by approximately 77%. In this regard, when prescribing duloxetine with CYP1A2 inhibitors (some quinolone antibacterial agents), it is advisable to prescribe duloxetine at a lower dose. Duloxetine is a moderate CYP2D6 inhibitor. When duloxetine is administered at a dose of 60 mg 2 times a day with a single dose of desipramine, which is a CYP2D6 substrate, the AUC of desipramine increases 3-fold. Co-administration of duloxetine (at a dose of 40 mg 2 times a day) increases the steady-state AUC of tolterodine (2 mg 2 times a day) by 71%, but does not affect the pharmacokinetics of the 5-hydroxyl metabolite. In this regard, caution must be exercised when prescribing duloxetine with CYP2D6 inhibitors, which have a narrow therapeutic index. Since CYP 2D6 is involved in the metabolism of duloxetine, simultaneous use of duloxetine with active CYP 2D6 inhibitors can lead to increased duloxetine blood concentrations. Paroxetine (20 mg once daily) reduces the plasma clearance of duloxetine by approximately 37%. In this regard, caution should be used when prescribing duloxetine with CYP2D6 inhibitors. When prescribing duloxetine in combination with other drugs that affect the central nervous system, especially those with a similar mechanism of action, caution should be exercised. Duloxetine is bound to plasma proteins (90%), therefore the administration of duloxetine to a patient taking other drugs that are significantly bound to plasma proteins may lead to an increase in the free concentration of any of these drugs.