Introduction
Baricitinib (trade name Olumiant) is a selective immunosuppressant, a reversible inhibitor of Janus kinase 1 and 2 (JAK1 and JAK2) [1].
Janus kinases (JAKs) are enzymes that transduce intracellular signals from cellular receptors for a number of cytokines and growth factors involved in hematopoiesis, inflammation and the immune response. As part of the intracellular signaling pathway, Janus kinases phosphorylate and activate STATs (signal transporters and activators of transcription), which in turn activate gene expression in the cell. Baricitinib modulates these signaling cascades by partially inhibiting the enzymatic activity of JAK1 and JAK2, thereby reducing STAT phosphorylation and activation. Indication for medical use of baricitinib, according to the instructions for medical use: treatment of active moderate or severe rheumatoid arthritis in adult patients intolerant of or lack of adequate response to treatment with one or more disease-modifying antirheumatic drugs.
Taking into account the effect of baricitinib on the immune response by disrupting the transduction of intracellular signals from cellular receptors for a number of cytokines (IL-6) and growth factors, the presumed effectiveness of baricitinib in the “cytokine storm” observed in severe COVID-19 is discussed.
A cytokine storm is a cascading uncontrolled increase in the level of cytokines in the blood, which can lead to an excessive immune response and damage to organs and tissues [2]. It has been established that with COVID-19, lymphohistiocytolysis also occurs, which leads to a cytokine storm, subsequently to multiple organ failure [3]. In 50% of cases, acute respiratory distress syndrome develops [3].
Side effects
Connective tissue, musculoskeletal system:
- swelling in the joint area;
- pain in the cervical spine;
- arthralgia;
- lockjaw;
- muscle spasm;
- bone pain;
- pain in the limbs;
- backache.
Parasitic, infectious lesions:
- urinary tract;
- upper respiratory tract;
- mucous membranes of the oral cavity.
sepsis , fungal diseases, septic shock, meningococcal shock, inflammation in the subcutaneous tissue, skin abscesses, infectious lesions of the gums and dental tissues, and sinusitis is possible .
Disturbances at the site of drug administration, general disorders:
- chest pain;
- weakness;
- chills;
- nonspecific responses at the injection site;
- influenza-like syndrome;
- discomfort in the chest area;
- swelling;
- paresthesia.
Instrumental, laboratory data:
- increased glutamate transferase;
- increase in liver enzymes ALT, AST.
Other reactions:
- red blood cell agglutination ;
- thrombocytopenia;
- coagulopathy;
- melanoma;
- myelodysplastic syndrome;
- hematomas;
- dizziness;
- tinnitus;
- feeling of “tides” of blood flow;
- cardiopalmus;
- blurred visual perception;
- irritation on the conjunctiva;
- anorexia;
- appetite disorders;
- hyperthyroidism;
- jaundice;
- fainting;
- paresthesia;
- dysgesia;
- gastroesophageal reflux;
- diarrhea syndrome;
- constipation;
- pain in the gums;
- bloating;
- epigastric pain syndrome;
- dysuria;
- hemoptysis;
- swelling of the mucous membranes of the nose;
- cough;
- anxiety;
- mood swings;
- depression;
- hyperhidrosis;
- alopecia;
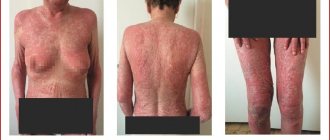
- allergic responses;
- menstrual irregularities;
- spontaneous erection.
Analysis of clinical guidelines, protocols for managing patients with COVID-19
According to the Temporary Guidelines of the Ministry of Health of the Russian Federation for the prevention, diagnosis and treatment of new coronavirus infection (COVID-19), version 6 (04/08/2020), as a pathogenetic treatment for moderate forms of pneumonia in order to suppress hyperinflammation and the development of serious lesions of the lungs and other organs caused by COVID-19, the administration of the tablet drug baricitinib (belongs to the group of Janus kinase inhibitors) can be considered as additional therapy (recommended dose: 4 mg once a day for 7-14 days). Baricitinib is included in treatment regimens for moderate forms of COVID-19 (pneumonia without respiratory failure) in patients over 60 years of age or patients with concomitant chronic diseases:
- Regimen 1: Hydroxychloroquine + azithromycin +/- baricitinib;
- Regimen 2: Mefloquine + azithromycin +/- baricitinib;
- Regimen 3: Lopinavir/ritonavir + recombinant interferon beta-1b +/- baricitinib.
Baricitinib is not mentioned in the treatment protocol for patients with COVID-19 provided by the COVID-19 Information Center at the University of Washington School of Medicine [16].
In Yale New Haven Health System's treatment algorithms for COVID-19 patients [17], baricitinib is included in the list of drugs not recommended as first-line treatment for COVID-19 (but may be considered in some clinical settings after discussion with clinical pharmacologists and specialists in the treatment of infectious diseases). In addition, there is a risk of developing severe infections with the use of baricitinib.
Contraindications
- Neisseria meningitides bacteria carriage;
- congenital complement deficiency (established diagnosis or suspected disease);
- lack of vaccination against Neisseria meningitides;
- active infection with Neisseria meningitides;
- individual hypersensitivity to mouse proteins, Eculizumab, and other components of the drug.
Relative contraindications:
- pathology of the kidneys, hepatic system (lack of clinical experience confirming the safety of Soliris use in people in this group);
- systemic active infectious lesions.
Analysis of completed and planned clinical studies
Currently, 5 clinical trials of baricitinib for the treatment of COVID-19 are registered on clinicaltrials.gov [4]: 1 completed (NCT04358614), 4 planned (NCT04340232, NCT04320277, NCT04346147, NCT04362943).
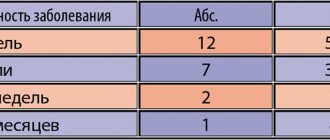
The completed study NCT04358614 [5] examined the use of baricitinib in combination with standard therapy. The study is not randomized, sequential. Researchers assessed the safety of baricitinib in combination with lopinavir-ritonavir for moderate viral pneumonia in patients with COVID-19. The study included 12 people who were prescribed baricitinib. The control group included 12 patients with COVID-19, moderate pneumonia, who received standard therapy (lopinavir + ritonavir 250 mg 2 times a day in combination with hydroxychloroquine 400 mg/day orally for 2 weeks) and hospitalized in the period immediately before the first patient who was prescribed baricitinib. Baricitinib was administered at a dose of 4 mg/day. Baricitinib treatment was well tolerated with no serious side effects. Fever, SpO2, PaO2/FiO2, CRP and MEWS scores improved significantly in the baricitinib group compared with the control group (p<0.05 in all comparisons). ICU transfer was observed in 33% (4/12) of control patients and in none of the baricitinib-treated patients (p=0.093). At week 2 of treatment, 58% (7/12) of baricitinib-treated patients and only 8% (1/12) of controls were discharged (p=0.027). The main limitations of this pilot study were the lack of blinding, lack of randomization and the small number of patients included in the study; additional studies are required to evaluate the effectiveness of baricitinib in patients with COVID-19.
The planned trial NCT04340232 plans to evaluate the efficacy and safety of baricitinib 2 mg once daily for 14 days in 80 patients with COVID-19 [6].
The Covid-19HUF trial (NCT04346147) is planned to evaluate the effectiveness of 3 treatment regimens for pneumonia in COVID-19:
1) hydroxychloroquine 200 mg 2 times a day orally + lopinavir/ritonavir (200/50 mg 2 times a day orally);
2) hydroxychloroquine 200 mg twice a day orally + imatinib 400 mg daily orally;
3) hydroxychloroquine 200 mg 2 times a day orally + baricitinib 4 mg daily orally [7].
The BARI-COVID trial (NCT04320277) [8] plans to evaluate the effectiveness of baricitinib 4 mg per day orally in combination with antiviral therapy lopinavir/ritonavir in patients with mild to moderate COVID-19. Efficacy is planned to be assessed by the proportion of patients who require transfer to the ICU during treatment.
During the retrospective clinical-epidemiological study COVID-AGE (NCT04362943), carried out on elderly patients over 70 years of age, hospitalized at the Perpetuo Socorro Hospital (Albacete, Spain) from 03/09/2020 to 04/20/2020, it is planned to analyze the clinical and epidemiological characteristics of patients with COVID -19 who were treated with baricitinib or anakinra and assessed their effectiveness [9].
According to the clinical trial registration website in the European Union (https://www.clinicaltrialsregister.eu), 3 studies of baricitinib are planned in patients with COVID-19.
The double-blind, randomized, placebo-controlled study 2020-001367-88 [10] plans to evaluate the effectiveness and safety of convalescent plasma (anti-SARS-CoV-2), hydroxychloroquine, sarilumab and baricitinib compared with placebo in combination with standard medical care for the treatment of patients with COVID-19 with moderate to severe pneumonia. The composite endpoint of this study was all-cause mortality or need for invasive mechanical ventilation recorded within 28 days. Study doses of baricitinib: 4 and 2 mg per day orally.
Study 2020-001321-31 corresponds to the previously described NCT04346147.
A cohort randomized controlled trial 2020-001246-18 is planned to identify immunomodulatory drugs with the best benefit/risk ratio in patients with COVID-19 [11]. The following drugs were included in the study: sarilumab (200 mg subcutaneous), tocilizumab (400 mg IV), anakinra (100 mg / 0.67 ml IV), hydroxychloroquine (200 mg orally), azithromycin (250 mg orally) , eculizumab (300 mg IV), baricitinib (2 mg orally), secukinumab (150 mg), bevacizumab (dosage 25 mg/ml, dose not reported).
Analysis of other publications
Stebbing J et al. [13] reviewed registered drugs from the perspective of potential use in COVID-19 and inhibition of clathrin-dependent endocytosis and thereby inhibition of viral infection of cells, predicted by artificial intelligence in silico. Drug targets include members of the insensitive kinase (NAK) family, including AAK1 and GAK, the inhibition of which has been shown to reduce viral infection in vitro [14][15]. Baricitinib was identified as a NAK inhibitor with particularly high affinity for AAK1, a master regulator of clathrin-dependent endocytosis. The authors suggested that this drug may be useful in counteracting SARS-CoV-2 infections, subject to appropriate clinical trials. Next, the authors identified and compared 3 drugs: baricitinib, ruxolitinib and fedratinib. After comparison, the authors conclude that although the three candidates have similar JAK (Janus kinase) inhibitor potencies, the high affinity for AAK1 suggests baricitinib is the best of the group, especially given its once-daily oral dosing and acceptable safety profile. .