Introduction
The drug tofacitinib is registered in the Russian Federation under the trade name Yaquinus (ATC code - L04AA29).
Belongs to the group Antineoplastic and immunomodulatory agents / immunosuppressants / selective immunosuppressants [13][14]. Tofacitinib is a selective and reversible inhibitor of Janus kinase 1 and 3 (JAK1 and JAK3). The selectivity for JAK2 in tofacitinib, in contrast to baricitinib, is less pronounced. The drug is approved for use in the treatment of rheumatoid and psoriatic arthritis, plaque psoriasis and ulcerative colitis [15]. Clinical studies are studying the effectiveness of tofacitinib therapy in patients with juvenile idiopathic arthritis, systemic lupus erythematosus, systemic scleroderma, vitiligo, alopecia, atopic dermatitis, etc. [7].
It should be taken into account that tofacitinib is a substrate of MDR1, but when prescribed in therapeutic doses it does not inhibit it; it is metabolized mainly by the CYP3A4 isoenzyme and, to a lesser extent, by CYP2C19. The dose of the drug requires adjustment in patients with impaired renal function [15][16].
Yaquinus, 5 mg, film-coated tablets, 56 pcs.
Serious infections
Serious and sometimes fatal infections due to bacterial, mycobacterial, fungal, viral, or other opportunistic pathogens have been reported in patients with rheumatoid arthritis receiving immunomodulators, including biologics and Jaquinus. The most common serious infections reported with use of Jaquinus include pneumonia, subcutaneous inflammation, herpes zoster, and urinary tract infection. Among the opportunistic infections when using the drug Yaquinus, cases of the development of tuberculosis and other mycobacterial infections, cryptococcosis, esophageal candidiasis, herpes zoster with damage to various dermatomes, cytomegalovirus infection, and BK virus infection were noted. Some patients have had disseminated disease, most often with the simultaneous use of immunomodulators - methotrexate or corticosteroids, which themselves and in addition to the underlying disease rheumatoid arthritis can predispose to the development of infections. It is also possible to develop other serious infections that were not reported in clinical studies (for example, histoplasmosis, coccidioidomycosis and listeriosis).
Jaquinus should not be used in patients with active infection, including localized infections. Before using Yaquinus, the risk/benefit ratio of therapy should be assessed in patients with chronic or recurrent infection, after contact with a patient with tuberculosis, a history of severe or opportunistic infection, in patients who have lived in or recently visited areas where tuberculosis or mycoses are endemic, and in patients with a predisposition to developing infection. Patients should be closely monitored for the development of signs and symptoms of infection during and after therapy with Jaquinus. Jaquinus should be temporarily discontinued if the patient develops a serious infection, opportunistic infection, or sepsis. If a new infection develops while using the drug Yaquinus, the patient is subject to a rapid and complete diagnostic examination, similar to a patient suffering from immunodeficiency. The appointment of appropriate antibacterial therapy, as well as careful dynamic monitoring, is indicated.
Since older patients usually have a higher incidence of infections, caution should also be exercised in such cases.
Tuberculosis
Before using Yaquinus, you should be screened for signs of latent or active tuberculosis infection.
Before initiating therapy with Yaquinus in patients with a history of latent or active tuberculosis, in the absence of confirmation of an adequate course of anti-tuberculosis therapy, as well as in patients with a negative test result for latent tuberculosis, but the presence of risk factors for tuberculosis infection, appropriate anti-tuberculosis therapy should be administered. When making a decision regarding the need for anti-tuberculosis therapy for each individual patient, it is recommended to consult with a TB specialist.
Patients should be closely monitored for development of signs of tuberculosis, including patients who test negative for latent tuberculosis before initiating therapy.
The incidence of tuberculosis with the use of the drug Yaquinus in the global clinical development program was 0.1-0.2%. Patients with latent tuberculosis are subject to standard antimycobacterial therapy before starting therapy with Yaquinus.
Reactivation of viral infections
Reactivation of viral infections has been described with DMARD therapy. Cases of reactivation of the herpes virus (for example, herpes zoster) have also been described in clinical studies of the drug Jaquinus. The effect of Yaquinus on the reactivation of chronic viral hepatitis is unknown. Patients testing positive for hepatitis B and C were excluded from clinical studies. Screening for the presence of viral hepatitis should be performed before initiating therapy with Yaquinus.
Malignant and lymphoproliferative diseases (except non-melanoma skin cancer)
There is a possibility that Jaquinus affects the body's defense against malignant neoplasms. The effect of therapy with Yaquinus on the development and course of malignant neoplasms is unknown, however, in clinical studies of this drug, cases of the development of malignant neoplasms were recorded.
Non-melanoma skin cancer (NSMC)
Cases of development of SCNM have been reported in patients receiving tofacitinib therapy. Periodic skin examination is recommended in patients at increased risk of developing skin cancer.
Cases of perforation of the gastrointestinal tract
Clinical studies of patients with rheumatoid arthritis have reported cases of gastrointestinal perforation, although the role of Janus kinase inhibition in these events is unknown. Such cases have mainly been described as diverticulum perforation, peritonitis, abscess and appendicitis. All patients who developed perforation of the gastrointestinal tract received concomitant therapy with NSAIDs and/or corticosteroids. The relative contribution of concomitant therapy and the use of Yaquinus in the development of gastrointestinal perforation is unknown.
Jaquinus should be used with caution in patients at increased risk of gastrointestinal perforation (eg, patients with a history of diverticulitis). Patients with new GI symptoms should be immediately evaluated for early detection of GI perforation.
Laboratory indicators
Neutrophils: Treatment with Yaquinus was associated with an increased incidence of neutropenia (less than 2000/mcL) compared to placebo. Treatment with Yaquinus in patients with low neutrophil concentrations (ANC less than 1000/mcL) is not recommended. In patients with a persistent decrease in ANC to 500-1000 cells/µl, the dose of Yaquinus should be reduced or treatment should be discontinued until the ANC concentration reaches more than 1000 cells/µl. In patients with an absolute neutrophil count less than 500/µl, treatment is not recommended. Neutrophil levels should be monitored after 4-8 weeks of therapy and then every 3 months.
Hemoglobin: It is not recommended to initiate therapy with Yaquinus in patients with low hemoglobin levels (less than 90 g/l). Treatment with Yaquinus should be discontinued in patients with a hemoglobin level of less than 80 g/L, or if the hemoglobin level decreases by 20 g/L or more during treatment. Hemoglobin should be monitored initially, after 4-8 weeks of therapy, and then every 3 months.
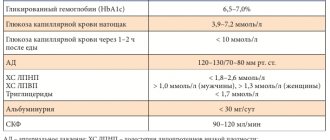
Lipids: treatment with Yaquinus is accompanied by an increase in blood lipid levels - total cholesterol, LDL cholesterol, and HDL cholesterol. Maximum effect was usually observed within 6 weeks. Assessment of lipid parameters should be performed approximately 4-8 weeks after the start of therapy. The use of statins in patients with elevated concentrations of total cholesterol and LDL cholesterol during therapy with Yaquinus allows achieving baseline values.
Vaccination
Information on vaccination response or secondary transmission of infection when live vaccines are administered to patients receiving Jaquinus is not yet available. It is not recommended to administer live vaccines at the same time as Jaquinus. It is recommended that all patients receive required immunizations in accordance with current vaccination recommendations before starting Yaquinus.
Patients with impaired renal function
In clinical studies, Yaquinus was not studied in patients with initial creatinine clearance <40 ml/min.
Impact on the ability to drive vehicles and operate machinery
Studies of the effect of the drug Yaquinus on the ability to drive a car and operate machinery have not been conducted.
Studies of tofacitinib as a pathogenetic therapy for COVID-19
The prerequisites for studying the role of tofacitinib in COVID-19 were observations of the significant role of various cytokines, and primarily IL-6, in the pathogenesis of patient decompensation and the development of cytokine storm and acute respiratory distress syndrome (ARDS). It is known that after the binding of cytokines to the corresponding membrane receptors, the intracellular signaling pathway JAK-STAT (Signal Transducer and Activator of Transcription) is activated, which regulates the effects of more than 50 cytokines, interferons and growth factors [7]. Tofacitinib can also significantly reduce the number of pathological natural killer cells, which some authors assign to one of the leading roles in the development of acute damage to internal organs during a cytokine storm [8]. A certain impetus for discussing the role of tofacitinib in the treatment of coronavirus infection was provided by research data and the start of a clinical trial (CT) of another JAK kinase inhibitor - baricitinib, however, unlike it, tofacitinib does not have the ability to block AP-2-associated protein kinase 1 and cyclin G- associated kinase, which are responsible for the endocytosis of the SARS-CoV-2 virus [11].
We did not find any experimental studies of the effectiveness of tofacitinib in COVID-19 or other ARDS.
A search for clinical trials in the ClinicalTrias.gov registry identified 2 studies: NCT04390061 and NCT04332042. Both studies are declared as open-label. Recruitment of patients has not begun. The randomized trial NCT04390061 (TOFACoV-2) will evaluate the efficacy of two weeks of tofacitinib 10 mg twice daily and hydroxychloroquine 200 mg three times daily versus hydroxychloroquine alone. Enrollment of 116 patients is planned, with evaluation results expected in October 2022. The second study, registration number NCT04332042, is a prospective cohort study that will enroll 50 patients. In this case, it is planned to study the preventive effect of tofacitinib at a dose of 10 mg 2 times a day, prescribed on the first day after hospitalization, on the severity of COVID-19, primarily on the risk of ARDS, mortality, and the safety of the drug.
Some conclusions may be drawn from a subgroup analysis of CT NCT04330495 (Santander, Spain), which is billed as a high-quality study and will be aimed at studying the prophylactic effect of hydroxychloroquine in patients receiving biological anti-inflammatory therapy, including tofacitinib. As with the above-mentioned CTs, patient recruitment for this CT has not begun (a total of 800 participants are planned to be recruited), and preliminary results are expected no earlier than November 2020.
A search in the CT registries ISRCTN, DRKS (Germany), ANZCTR (Australia and New Zealand), the European Clinical Trials Registry, the Chinese ChiCTR registry, UMIN-CTR (Japan), the national registries of Thailand, the Netherlands, India and Singapore did not find any CTs other than mentioned above.
An expert review by Italian experts, published on May 5, recommends use, including tofacitinib, in patients with rheumatic diseases and autoimmune lesions of the gastrointestinal tract when COVID-19 infection is detected [10]. A similar recommendation for discontinuation of tofacitinib in patients with ulcerative colitis with SARS-CoV-2 infection is contained in a recent article by American gastroenterologists [2]. “Clinical caution” in the use of tofacitinib is recommended by the authors of the British guidelines for the management of patients with inflammatory bowel disease. They do not make recommendations for discontinuation of the drug in uninfected patients, but classify them as an “average risk” group in which stricter adherence to nonspecific prophylaxis (social distancing) is required [4].
Safety of tofacitinib
It should be noted that, according to the instructions for medical use, tofacitinib is contraindicated in patients with creatinine clearance less than 40 ml per minute, infection with hepatitis B and C viruses, patients receiving therapy with IL-6 receptor antagonists, which include tocilizumab and sarilumab, with severe and active infections, children, lactating and pregnant women, and administration at a dose of 10 mg 2 times a day is contraindicated if there is a history of venous thromboembolism (deep veins, pulmonary embolism), hereditary blood clotting disorders, patients with heart failure (without indication of severity) [15]. This circumstance significantly limits the use of tofacitinib in patients with COVID-19. The instructions for medical use provide recommendations for reducing the daily dose of the drug from 20 mg to 10 mg (5 mg 2 times a day) in patients with rheumatoid arthritis and the presence of at least one cardiovascular risk factor, as well as discontinuing the drug in patients at risk [17].
Among the adverse reactions of tofacitinib, the development of anemia, lymphopenia and neutropenia should be noted, which, when laboratory values reach below 500 cells/ml (for lymphocytes and neutrophils) or 90 g/l (for hemoglobin), require discontinuation of the drug. In this context, it should be noted that some authors consider lymphopenia a risk factor for the development of ARDS and negative outcome of COVID-19 [12].
Another complication of drug therapy is the development of respiratory tract infections. This fact is reflected in the instructions for use and confirmed by a meta-analysis by Khoo JK et al., published in May 2022 on the website of the journal Rheumatology [5][15]. The literature reports a case of SARS-CoV-2 infection in a 33-year-old patient with ulcerative colitis while taking tofacitinib (10 mg twice daily) [3].
The association of tofacitinib use with the risk of thromboembolic complications and death from them has also been shown in a number of clinical trials [6][9].
The presence of these risks (risk of developing infections, lymphomas and other malignant tumors, arterial or venous thrombosis, increased mortality from cardiovascular accidents in people over 50 years of age with at least one cardiovascular risk factor) when using tofacitinib led to the appearance of a special safety notice - black box warning - in the instructions for use of the drug in the USA [1][16] and the release of a special EMA notice that restricts the use of the drug [17][18].
Jakvinus
Serious infections
Serious and sometimes fatal infections due to bacterial, mycobacterial, fibrous, viral, or other opportunistic pathogens have been reported in patients with rheumatoid arthritis receiving immunomodulators, including biologics and Jaquinus. The most common serious infections reported with use of Jaquinus include pneumonia, subcutaneous inflammation, herpes zoster, and urinary tract infection. Among the opportunistic infections when using the drug Yaquinus, cases of the development of tuberculosis and other mycobacterial infections, cryptococcosis, esophageal candidiasis, herpes zoster with damage to various dermatomes, cytomegalovirus infection, and BK virus infection were noted. Some patients have had disseminated disease, most often with the simultaneous use of immunomodulators - methotrexate or corticosteroids, which themselves and in addition to the underlying disease rheumatoid arthritis can predispose to the development of infections. It is also possible to develop other serious infections that were not reported in clinical studies (for example, histoplasmosis, coccidioidomycosis and listeriosis).
Jaquinus should not be used in patients with active infection, including localized infections. Before using Yaquinus, the risk/benefit ratio of therapy should be assessed in patients with chronic or recurrent infection, after contact with a patient with tuberculosis, a history of severe or opportunistic infection, in patients who have lived in or recently visited areas where tuberculosis or mycoses are endemic, and in patients with a predisposition to developing infection. Patients should be closely monitored for the development of signs and symptoms of infection during and after therapy with Jaquinus. Jaquinus should be temporarily discontinued if the patient develops a serious infection, opportunistic infection, or sepsis. If a new infection develops while using the drug Yaquinus, the patient is subject to a rapid and complete diagnostic examination, similar to a patient suffering from immunodeficiency. The appointment of appropriate antibacterial therapy, as well as careful dynamic monitoring, is indicated.
Since older patients usually have a higher incidence of infections, caution should also be exercised in such cases.
Tuberculosis
Before using Yaquinus, you should be screened for signs of latent or active tuberculosis infection.
Before initiating therapy with Yaquinus in patients with a history of latent or active tuberculosis, in the absence of confirmation of an adequate course of anti-tuberculosis therapy, as well as in patients with a negative test result for latent tuberculosis, but the presence of risk factors for tuberculosis infection, appropriate anti-tuberculosis therapy should be administered. When making a decision regarding the need for anti-tuberculosis therapy for each individual patient, it is recommended to consult with a TB specialist.
Patients should be closely monitored for development of signs of tuberculosis, including patients with a negative test result for latent tuberculosis, before initiating therapy.
The incidence of tuberculosis with the use of the drug Yaquinus within the framework of the global clinical development program was 0.1 - 0.2%. Patients with latent tuberculosis are subject to standard antimycobacterial therapy before starting therapy with Yaquinus.
Reactivation of viral infections
Reactivation of viral infections has been described with DMARD therapy. Cases of reactivation of the herpes virus (for example, herpes zoster) have also been described in clinical studies of the drug Jaquinus. The effect of Yaquinus on the reactivation of chronic viral hepatitis is unknown. Patients testing positive for hepatitis B and C were excluded from clinical studies.
Malignant and lymphoproliferative diseases
There is a possibility that Jaquinus affects the body's defense against malignant neoplasms. The effect of therapy with Yaquinus on the development and course of malignant neoplasms is unknown, however, in clinical studies of this drug, cases of the development of malignant neoplasms were recorded.
Cases of perforation of the gastrointestinal tract
Clinical studies of patients with rheumatoid arthritis have reported cases of gastrointestinal perforation, although the role of Janus kinase inhibition in these events is unknown. Such cases have mainly been described as diverticulum perforation, peritonitis, abscess and appendicitis. All patients who developed gastrointestinal perforation received concomitant therapy with nonsteroidal anti-inflammatory drugs (NSAIDs) and/or glucocorticoids. The relative contribution of concomitant therapy and the use of Yaquinus in the development of gastrointestinal perforation is unknown.
Jaquinus should be used with caution in patients at increased risk of gastrointestinal perforation (eg, patients with a history of diverticulitis). Patients with new GI symptoms should be immediately evaluated for early detection of GI perforation.
Laboratory indicators
Neutrophils: Treatment with Yaquinus was associated with an increased incidence of neutropenia (<2000/mm3) compared to placebo. Treatment with Yaquinus in patients with low neutrophil concentrations (ANC less than 1000/mm3) is not recommended. In patients with a persistent decrease in ANC to 500-1000/mm3, the dose of Yaquinus should be reduced or treatment should be discontinued until the ANC concentration reaches more than 1000 cells/mm3. In patients with an absolute neutrophil count less than 500/mm3, treatment is not recommended. Neutrophil levels should be monitored after 4-8 weeks of therapy, and then every 3 months (see sections “Dosage and Administration”, “Side Effects”).
Hemoglobin: It is not recommended to initiate therapy with Yaquinus in patients with low hemoglobin levels (less than 90 g/l). Treatment with Yaquinus should be discontinued in patients with a hemoglobin level of less than 80 g/L, or if the hemoglobin level decreases by 20 g/L or more during treatment. Hemoglobin should be monitored at the initial stage of therapy, after 4-8 weeks of therapy, and then every 3 months (see section "Dosage and Administration").
Lipids: treatment with Yaquinus is accompanied by an increase in blood lipid levels - total cholesterol, LDL cholesterol, and high-density lipoprotein cholesterol (HDL). Maximum effect was usually observed within 6 weeks. Assessment of lipid parameters should be performed approximately 4-8 weeks after the start of therapy. The use of statins in patients with elevated concentrations of total cholesterol and LDL cholesterol during therapy with Yaquinus allows achieving baseline values.
Vaccinations
Information on vaccination response or secondary transmission of infection when live vaccines are administered to patients receiving Jaquinus is not yet available. It is not recommended to administer live vaccines at the same time as Jaquinus. It is recommended that all patients receive required immunizations in accordance with current vaccination recommendations before starting Yaquinus.
Patients with impaired renal function
In clinical studies, Yaquinus was not studied in patients with initial creatinine clearance less than 40 ml/min (see section "Contraindications").
Impact on the ability to drive a car and other complex mechanisms
Studies of the effect of the drug Yaquinus on the ability to drive a car and operate machinery have not been conducted.