Compound
The composition of 1 capsule of the drug includes dabigatran etexilate mesylate 172.95 mg (150 mg in terms of dabigatran etexilate ) and additional substances: tartaric acid, dimethicone , acacia gum, hypromellose, talc, hydroxypropylcellulose, potassium chloride, E407, E171, E132, E110 , water, butanol, ethanol, isopropanol , shellac, pylene glycol, E172.
There is also a dosage form containing dabigatran etexilate 75 mg and 110 mg.
Pharmacodynamics and pharmacokinetics
The active substance of the tablet, after conversion to dabigatran , inhibits the activity of the enzyme thrombin , which in turn is responsible for the process of converting fibrinogen into fibrin and the formation of a blood clot . Dabigatran also has the ability to reduce the activity of already formed blood clots, free thrombin, fibrin-bound thrombin , subsequent platelet aggregation does not occur.
The active component effectively reduces the prothrombin index , in direct proportion to its concentration in the blood plasma achieved while taking the drug.
Almost immediately after taking the drug, a hydrolysis , converting dabigatran etexilate into dabigatran. The bioavailability of dabigatran is about 6%, the maximum concentration of the active substance will be observed within an hour or two after administration. Regardless of the dose taken, the half-life is from 11 to 14 hours. In patients with renal failure, changes in some pharmacokinetic parameters occur.
Laboratory monitoring of the effect of dabigatran
Dabigatran was created as a drug that does not require laboratory control due to the high predictability of its anticoagulant effect. However, there are situations where such control is necessary. These include life-threatening bleeding (including intracranial hemorrhage), drug overdose, and the need for emergency surgery.
Since dabigatran interacts with thrombin to prevent fibrin clot formation, it would seem that conventional coagulation tests such as activated partial thromboplastin time (aPTT) and thrombin time are applicable.
In patients receiving continuous therapy with dabigatran at a dose of 150 mg 2 times a day, the aPTT is approximately 2 times higher than normal values. At the same time, an increase in the dose and, accordingly, the concentration of the drug in plasma does not lead to a proportional prolongation of the aPTT. In other words, APTT is poorly suited for detecting drug overdose.
Taking dabigatran has little effect on the value of prothrombin time and, accordingly, on the level of international normalized ratio (INR), and therefore it is also not possible to use this test.
A particularly sensitive test for determining the effect of dabigatran is the thrombin time. It is directly proportional to the plasma concentration of dabigatran. But this test also has its limitations. It detects even minimal concentrations of dabigatran, but at high concentrations of the drug in the blood (over 600 ng/ml), the duration of clot formation in the coagulometer cuvette becomes so long that it exceeds the upper limit of detection capability. Thus, this test is not informative in cases of dabigatran overdose. In addition, we should not forget that the test is poorly standardized.
Measuring ecarin time allows monitoring the effect of dabigatran, which inhibits the activity of mesothrombin, which is formed from prothrombin under the influence of ecarin. Thus, the activity of dabigatran is measured directly. When taking dabigatran at a dose of 150 mg 2 times a day, the ecarin time is extended by 2–4 times. A direct correlation was found between the test results and the concentration of the blood product.
Currently, this test is not routinely used or standardized. It is used only for research purposes [5]. The drug is contraindicated if the glomerular filtration rate is less than 30 ml/min.
Contraindications
Pradaxa is contraindicated:
- in case of drug allergy to the active substance, its derivatives and other components;
- in cases of liver dysfunction;
- severe renal failure;
- high probability of bleeding due to stomach ulcers , malignant neoplasms , damage to the brain or spinal cord, vascular aneurysm and other pathologies;
- artificial valve in the heart;
- when combined with other anticoagulants , Ketoconazole , Cyclosporine , Itraconazole .
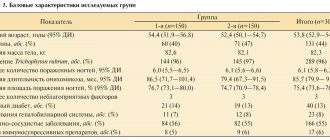
Use of dabigatran to prevent thromboembolic complications
This problem has been studied in phase II and III studies following hip and knee replacement. The clinical efficacy of dabigatran and enoxaparin has been shown to be comparable. The frequency of hemorrhagic complications and cases of increased activity of alanine aspartate aminotransferase (ALT and AST) did not differ significantly between groups [6, 7]. At the same time, experience with ximelagatran forced researchers to strictly monitor the activity of liver enzymes. The studies did not include patients whose ALT or AST activity was 2 or more times higher than normal.
It has been proven that in the treatment of pulmonary embolism, the effectiveness and safety of dabigatran and warfarin are comparable, while therapy with dabigatran does not require laboratory monitoring [8].
Side effects
Possible:
- thrombocytopenia and anemia , intracranial bleeding ;
- formation of hematomas , the occurrence of bleeding of various origins and locations, including from postoperative wounds, nose, stomach and intestines;
- bronchospasm hypersensitivity reactions such as urticaria , itching and rash ;
- diarrhea , abdominal pain, indigestion , nausea , dysphagia , liver dysfunction;
- hemarthrosis , hematuria;
- bleeding , poor healing, formation of hematomas and discharge from wounds, drainage from wounds.
Interaction
Do not combine with drugs that affect hemostasis, vitamin K antagonists , P-glycoprotein inhibitors ( Verapamil , Ketoconazole , Clarithromycin , Amiodarone , Quinidine ).
Use with caution in combination with dronedarone , St. John's wort , Carbamazepine and Pantoprazole .
Acetylsalicylic acid in combination with Pradaxa may significantly increase the risk of bleeding.
Actions for dabigatran overdose and bleeding
In in vitro models, dabigatran was inactivated by activated charcoal. Although these data have not been confirmed in patients, if an overdose of dabigatran is suspected, activated charcoal should be given within 1-2 hours after taking it. If an overdose is detected at a later date, hemofiltration using carbon filters is used. Additionally, dabigatran can be removed by hemodialysis.
If bleeding develops while taking dabigatran, it should be borne in mind that the concentration of the drug decreases quite quickly after its discontinuation. Since the drug is excreted through the kidneys, diuretics can speed up its excretion.
In case of severe bleeding, it is possible to use eptacog alfa (activated), which can independently activate thrombin without the participation of tissue factor. It should be noted that this recommendation is based on extrapolation of data obtained for other thrombin inhibitors.
It is possible to prescribe prothrombin complex concentrate [5].
Analogues of Pradaxa
There are practically no analogues of Pradaxa, the closest in effect to the medicine are Warfarin and Xarelto .
Which is better: Pradaxa or Warfarin?
Warfarin is the most used vitamin K antagonist , and has many restrictions on its use. Constant monitoring of the INR is required; the drug is not compatible with all foods and medications. Not everyone is able to maintain the required INR level, which leads to unwanted side effects or a decrease in the effectiveness of the drug. Unlike Warfarin, Pradaxa is a new generation drug, the risk of bleeding is lower with the drug, and there are fewer restrictions on its use.
In any case, which drug should be used, Pradaxa or Warfarin, must be decided by the attending physician.
Pradaxa, 30 pcs., 75 mg, capsules
Inside
, regardless of the time of meal, with a glass of water to facilitate the passage of the drug into the stomach, 1 or 2 times a day. The capsule should not be opened.
Special instructions when removing capsules from the blister:
— tear off one individual blister from the blister package along the perforation line;
— remove the capsule from the blister, peeling off the foil;
- do not squeeze capsules through the foil.
Use in adults
Prevention of venous thromboembolism (VTE) in patients after orthopedic surgery:
The recommended dose is 220 mg 1 time per day (2 capsules of 110 mg each).
In patients with moderate renal impairment due to risk of bleeding
The recommended dose is 150 mg 1 time per day (2 capsules of 75 mg).
Prevention of VTE after knee replacement:
The use of Pradaxa® should be started 1–4 hours after completion of the operation with 1 capsule. (110 mg) followed by increasing the dose to 2 caps. (220 mg) once daily for the next 10 days. If hemostasis is not achieved, treatment should be delayed. If treatment has not started on the day of surgery, therapy should begin with 2 caps. (220 mg) once a day.
Prevention of VTE after hip replacement:
The use of Pradaxa® should be started 1–4 hours after completion of the operation with 1 capsule. (110 mg) followed by increasing the dose to 2 caps. (220 mg) once daily for the next 28–35 days. If hemostasis is not achieved, treatment should be delayed. If treatment has not started on the day of surgery, therapy should begin with 2 caps. (220 mg) once a day.
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation:
It is recommended to use Pradaxa® in a daily dose of 300 mg (1 capsule of 150 mg 2 times a day). Therapy should continue for life.
Treatment of acute DVT and/or PE and prevention of deaths caused by these diseases:
It is recommended to use Pradaxa® in a daily dose of 300 mg (1 capsule of 150 mg 2 times a day) after parenteral treatment with an anticoagulant for at least 5 days. Therapy should continue for up to 6 months.
Prevention of recurrent DVT and/or PE and deaths caused by these diseases:
It is recommended to use Pradaxa® in a daily dose of 300 mg (1 capsule of 150 mg 2 times a day). Therapy can be continued for life, depending on individual risk factors.
Use in special patient groups
Children.
The effectiveness and safety of Pradaxa® have not been studied in patients under 18 years of age, so use in children is not recommended (see “Contraindications”).
Renal dysfunction.
Before therapy, in order to avoid prescribing the drug to patients with severe renal impairment (Cl creatinine <30 ml/min), it is necessary to first assess creatinine clearance. Due to the lack of data on the use of the drug in patients with severe renal impairment (Cl creatinine <30 ml/min), the use of Pradaxa® is contraindicated (see “Contraindications”).
Renal function should be assessed during treatment when there is a suspicion of a possible decrease or deterioration in renal function (for example, with hypovolemia, dehydration, simultaneous use of certain medications).
During the clinical development of Pradaxa®, the calculation of creatinine clearance using the Cocroft-Gault formula was used as a method for assessing renal function .
.
Dabigatran is eliminated by hemodialysis; however, clinical experience with hemodialysis patients is limited.
When using Pradaxa® for the prevention of VTE in patients after orthopedic surgery
in case of moderate renal dysfunction (creatinine clearance 30–50 ml/min), the daily dose of the drug should be reduced to 150 mg (2 capsules of 75 mg 1 time per day).
When using Pradaxa® to prevent stroke, systemic thromboembolism and reduce cardiovascular mortality in patients with atrial fibrillation
for moderate renal dysfunction (creatinine clearance 30–50 ml/min), no dose adjustment is required. It is recommended to use the drug in a daily dose of 300 mg (1 capsule 150 mg 2 times a day). Kidney function should be assessed at least once a year.
When using Pradaxa® for the treatment of acute DVT and/or PE and the prevention of deaths caused by these diseases
when creatinine Cl <30 ml/min, no dose adjustment is required. It is recommended to use the drug in a daily dose of 300 mg (1 capsule 150 mg 2 times a day).
When using Pradaxa® for the prevention of recurrent DVT and/or PE and deaths caused by these diseases
, with moderate renal dysfunction (Cl creatinine 30–50 ml/min), no dose adjustment is required. It is recommended to use the drug in a daily dose of 300 mg (1 capsule 150 mg 2 times a day). Kidney function should be assessed at least once a year.
Elderly age.
Due to the fact that increased drug exposure in elderly patients (over 75 years of age) is often due to decreased renal function, renal function should be assessed before prescribing the drug. Renal function should be assessed at least once a year or more frequently depending on the clinical situation. Dose adjustment of the drug should be carried out depending on the severity of renal dysfunction (see “Renal dysfunction”).
Prevention of VTE in elderly patients (over 75 years of age) after orthopedic surgery:
Application experience is limited. The recommended dose is 150 mg (2 capsules of 75 mg once).
When using Pradaxa® in elderly patients over 80 years of age to prevent stroke, systemic thromboembolism and reduce cardiovascular mortality in patients with atrial fibrillation
it should be taken in a daily dose of 220 mg (1 capsule of 110 mg 2 times a day).
Treatment of acute DVT and/or PE and prevention of deaths caused by these diseases in patients over 75 years of age:
no dose adjustment is required. It is recommended to use the drug in a daily dose of 300 mg (1 capsule 150 mg 2 times a day).
Prevention of recurrent DVT and/or PE and deaths caused by these diseases in patients over 75 years of age:
no dose adjustment is required. It is recommended to use the drug in a daily dose of 300 mg (1 capsule 150 mg 2 times a day).
Effect of body weight
Prevention of VTE in patients after orthopedic surgery:
in patients weighing less than 50 and more than 110 kg, experience with use is limited. In accordance with pharmacokinetic and clinical data, no dose adjustment is required. However, it is recommended to monitor such patients.
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation:
According to pharmacokinetic and clinical data, no dose adjustment is required. However, patients weighing less than 50 kg are recommended to be monitored.
Treatment of acute DVT and/or PE and prevention of deaths caused by these diseases
: No dose adjustment is required depending on body weight.
Prevention of recurrent DVT and/or PE and deaths caused by these diseases:
no dose adjustment is required depending on body weight.
Concomitant use of Pradaxa® with active P-gp inhibitors (amiodarone, quinidine, verapamil) for the prevention of venous thromboembolism in patients after orthopedic surgery
When used simultaneously with amiodarone, quinidine or verapamil, the dose of Pradaxa® should be reduced to 150 mg once a day (2 capsules of 75 mg each) (see “Interactions”).
Patients taking Pradaxa® after orthopedic surgery are not recommended to simultaneously start using verapamil and connect it to therapy in the future.
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation:
no dose adjustment is required; patients are recommended to use the drug in a daily dose of 300 mg (1 capsule of 150 mg 2 times a day).
Treatment of acute DVT and/or PE and prevention of deaths caused by these diseases:
no dose adjustment is required. It is recommended to use the drug in a daily dose of 300 mg (1 capsule 150 mg 2 times a day).
Prevention of recurrent DVT and/or PE and deaths caused by these diseases:
no dose adjustment is required. It is recommended to use the drug in a daily dose of 300 mg (1 capsule 150 mg 2 times a day).
Use in patients at increased risk of bleeding
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation:
the presence of factors such as age 75 years or older, moderately reduced renal function (Cl creatinine 30–50 ml/min), simultaneous use of P-gp inhibitors, antiplatelet agents, or a history of gastrointestinal bleeding may increase the risk of bleeding (see " Special instructions"). In patients with one or more of these risk factors, at the discretion of the physician, the daily dose of Pradaxa® may be reduced to 220 mg (take 1 capsule 110 mg 2 times a day).
Treatment of DVT and/or PE and prevention of deaths caused by these diseases:
the presence of factors such as age 75 years or older, moderate decrease in renal function (Cl creatinine 30-50 ml/min) or a history of gastrointestinal bleeding may increase the risk of bleeding (see "Special Instructions"). In patients with one risk factor, no dose adjustment is required. For patients with multiple risk factors, clinical data are limited. In such patients, the drug should be used only in cases where the expected benefit outweighs the risk of bleeding.
Prevention of recurrent DVT and/or PE and deaths caused by these diseases:
the presence of factors such as age 75 years or older, moderate decrease in renal function (Cl creatinine 30-50 ml/min) or a history of gastrointestinal bleeding may increase the risk of bleeding (see "Special Instructions"). In patients with one risk factor, no dose adjustment is required. For patients with multiple risk factors, clinical data are limited. In such patients, the drug should be used only in cases where the expected benefit outweighs the risk of bleeding.
Transition from the use of Pradaxa® to parenteral use of anticoagulants
Prevention of VTE in patients after orthopedic surgery:
Parenteral administration of anticoagulants should begin 24 hours after taking the last dose of Pradaxa®.
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation:
Parenteral use of anticoagulants should be started 12 hours after taking the last dose of Pradaxa®.
Treatment of acute DVT and/or PE and prevention of deaths caused by these diseases:
Parenteral use of anticoagulants should be started 12 hours after taking the last dose of Pradaxa®.
Prevention of recurrent DVT and/or PE and deaths caused by these diseases:
Parenteral use of anticoagulants should be started 12 hours after taking the last dose of Pradaxa®.
Transition from parenteral use of anticoagulants to the use of Pradaxa®
The first dose of Pradaxa® is prescribed instead of a discontinued anticoagulant in the interval 0-2 hours before the next injection of alternative therapy or simultaneously with the cessation of a continuous infusion (for example, intravenous use of unfractionated heparin).
Switching from vitamin K antagonists to Pradaxa®
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation:
the use of vitamin K antagonists is discontinued; the use of Pradaxa® is possible with an INR <2.
Treatment of acute DVT and/or PE and prevention of deaths caused by these diseases:
the use of vitamin K antagonists is discontinued; the use of Pradaxa® is possible with an INR <2.
Prevention of recurrent DVT and/or PE and deaths caused by these diseases:
the use of vitamin K antagonists is discontinued; the use of Pradaxa® is possible with an INR <2.
Switching from Pradaxa® to vitamin K antagonists
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation:
with Cl creatinine ≥50 ml/min, the use of vitamin K antagonists is possible 3 days, and with Cl creatinine 30–50 ml/min - 2 days before discontinuation of Pradaxa®.
Treatment of acute DVT and/or PE and prevention of deaths caused by these diseases:
with Cl creatinine ≥50 ml/min, the use of vitamin K antagonists is possible 3 days, and with Cl creatinine 30–50 ml/min - 2 days before discontinuation of Pradaxa®.
Prevention of recurrent DVT and/or PE and deaths caused by these diseases:
with Cl creatinine ≥50 ml/min, the use of vitamin K antagonists is possible 3 days, and with Cl creatinine 30–50 ml/min - 2 days before discontinuation of Pradaxa®.
Cardioversion
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation.
Carrying out planned or emergency cardioversion does not require discontinuation of Pradaxa® therapy.
Missed dose
Prevention of venous thromboembolism in patients after orthopedic surgery:
It is recommended that you take your usual daily dose of Pradaxa® at your usual time the next day. If you miss individual doses, you should not take a double dose of the drug.
Prevention of stroke, systemic thromboembolism and reduction of cardiovascular mortality in patients with atrial fibrillation:
a missed dose of Pradaxa® can be taken if there are 6 hours or more left before taking the next dose of the drug; If the period is less than 6 hours, the missed dose should not be taken. If you miss individual doses, you should not take a double dose of the drug.
Treatment of acute DVT and/or PE and prevention of deaths caused by these diseases:
a missed dose of Pradaxa® can be taken if there are 6 hours or more left before taking the next dose of the drug; If the period is less than 6 hours, the missed dose should not be taken. If you miss individual doses, you should not take a double dose of the drug.
Prevention of recurrent DVT and/or PE and deaths caused by these diseases:
a missed dose of Pradaxa® can be taken if there are 6 hours or more left before taking the next dose of the drug; If the period is less than 6 hours, the missed dose should not be taken. If you miss individual doses, you should not take a double dose of the drug.
Pradaxa price (where to buy)
The price of Pradaxa 110 mg is about 3,200 rubles for 60 pieces.
You can buy Pradaxa in Moscow for 2000 rubles for 30 capsules of 75 mg.
The price of Pradaxa 150 mg is within 2000 rubles for 30 pieces.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
ZdravCity
- Pradaxa capsules 150 mg 30 pcs.
Boehringer IngelheimBoehringer Ingelheim Pharma GmbH and Co.KG 1850 rub.order - Pradaxa capsules 110 mg 30 pcs. Boehringer Ingelheim Pharma GmbH and Co. KG
RUR 1,847 order
- Pradaxa capsules 75 mg 30 pcs.Boehringer Ingelheim
RUR 1,877 order
- Pradaxa capsules 110 mg 60 pcs.Boehringer Ingelheim
RUB 3,239 order
- Pradaxa capsules 150 mg 60 pcs.Boehringer Ingelheim
RUB 3,231 order
Pharmacy Dialogue
- Pradaxa (caps. 150 mg No. 60) Boehringer Ingelheim
RUR 3,179 order
- Pradaxa (caps. 110 mg No. 60) Boehringer Ingelheim
RUB 3,199 order
- Pradaxa (caps. 110 mg No. 30) Boehringer Ingelheim
RUB 1,772 order
- Pradaxa (caps. 75 mg No. 30) Boehringer Ingelheim
RUB 1,772 order
- Pradaxa (caps. 150 mg No. 30)Boehringer Ingelheim
RUB 1845 order
show more
Pharmacy24
- Pradaxa 110 mg No. 60 capsules Boehringer Ingelheim Pharma GmbH & Co.
KG, Nimechchina 2148 UAH. order - Pradaxa 110 mg No. 60 capsules Promotion Boehringer Ingelheim Pharma GmbH & Co. KG, Nimechchina
1030 UAH. order
- Pradaxa 150 mg No. 60 capsules Boehringer Ingelheim Pharma GmbH & Co. KG, Nimechchina
2148 UAH order
- Pradaxa 150 mg No. 60 capsules Promotion Boehringer Ingelheim Pharma GmbH & Co. KG, Nimechchina
1030 UAH. order