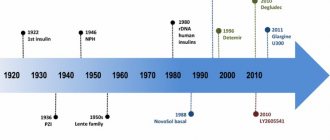
Insulin aspart biphasic
International name of the medicinal substance:
Insulin aspart biphasic (Insulin aspart biphasic) The list of drugs containing the active substance Insulin aspart biphasic is given after the description.
Pharmacological action:
Hypoglycemic agent, an analogue of human insulin with an average duration of action.
Interacts with a specific receptor on the outer cell membrane and forms an insulin-receptor complex that stimulates intracellular processes, incl. synthesis of a number of key enzymes (hexokinase, pyruvate kinase, glycogen synthetase). The decrease in the concentration of glucose in the blood is due to an increase in its intracellular transport, increased absorption by tissues, stimulation of lipogenesis, glycogenogenesis, and a decrease in the rate of glucose production by the liver. Has the same activity as human insulin in molar equivalent. Substitution of the amino acid proline at position B28 with aspartic acid reduces the tendency of molecules to form hexamers in the soluble fraction of the drug, which is observed in soluble human insulin. In this regard, insulin aspart is absorbed from subcutaneous fat faster than soluble insulin contained in biphasic human insulin. Insulin aspart protamine takes longer to be absorbed. After subcutaneous administration, the effect develops after 10-20 minutes, the maximum effect after 1-4 hours. The duration of action reaches 24 hours (depending on the dose, injection site, blood flow intensity, body temperature and physical activity). Pharmacokinetics:
When administered subcutaneously at a dose of 0.2 U/kg body weight, Cmax is 108-172 pmol/l, TCmax is 60-95 minutes. T1/2, reflecting the rate of absorption of the protamine-bound fraction, is 8-9 hours. The concentration of insulin in the serum returns to its original level after 15-18 hours. Indications for use. Diabetes mellitus type 1. Diabetes mellitus type 2 (in case of resistance to oral hypoglycemic agents, partial resistance to these drugs during combination therapy, intercurrent diseases).
Indications:
Diabetes mellitus type 1. Diabetes mellitus type 2 (in case of resistance to oral hypoglycemic agents, partial resistance to these drugs during combination therapy, intercurrent diseases).
Contraindications:
Hypersensitivity, hypoglycemia, age under 18 years.
Side effects:
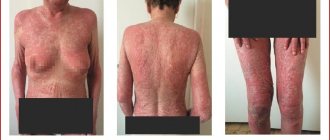
At the beginning of treatment - swelling, refractive error (usually temporary).
Local allergic reactions: hyperemia, swelling, itching of the skin at the injection site. Generalized allergic reactions: skin rash, itchy skin, increased sweating, gastrointestinal dysfunction, angioedema, difficulty breathing, tachycardia, decreased blood pressure. Lipodystrophy at the injection site. Interaction:
The hypoglycemic effect of insulin is enhanced by oral hypoglycemic drugs, MAO inhibitors, ACE inhibitors, carbonic anhydrase inhibitors, non-selective beta-blockers, bromocriptine, octreotide, sulfonamides, anabolic steroids, tetracyclines, clofibrate, ketoconazole, mebendazole, pyridoxine, theophylline, cyclophosphamide, fenfl uramine, drugs Li+, ethanol and ethanol-containing drugs.
The hypoglycemic effect of insulin is weakened by oral contraceptives, corticosteroids, thyroid hormones, thiazide diuretics, heparin, tricyclic antidepressants, sympathomimetics, danazol, clonidine, BMCC, diazoxide, morphine, phenytoin, nicotine. Under the influence of reserpine and salicylates, it is possible to both weaken and enhance the effect of the drug. Special instructions:
Do not administer intravenously.
Insufficient dosage of the drug or cessation of treatment, especially in type 1 diabetes mellitus, can lead to the development of hyperglycemia or diabetic ketoacidosis. Typically, symptoms of hyperglycemia appear gradually over several hours or days. Symptoms of hyperglycemia are nausea, vomiting, drowsiness, redness and dryness of the skin, dry mouth, increased urine output, thirst and loss of appetite, as well as the smell of acetone in the exhaled air. Without appropriate treatment, hyperglycemia can lead to death. After compensation of carbohydrate metabolism, for example, with intensive insulin therapy, patients may experience changes in their typical symptoms that are precursors of hypoglycemia, of which patients should be informed. In patients with diabetes mellitus, with optimal metabolic control, late complications of diabetes develop later and progress more slowly. In this regard, it is recommended to carry out measures aimed at optimizing metabolic control, including monitoring blood glucose concentrations. The drug should be administered in direct connection with food intake. The high rate of onset of the drug's effect should be taken into account when treating patients with concomitant diseases or taking drugs that slow down the absorption of food. In the presence of concomitant diseases, especially of an infectious nature, the need for insulin, as a rule, increases. Impaired kidney or liver function may reduce insulin requirements. Skipping meals or unplanned exercise can lead to hypoglycemia. Compared with biphasic human insulin, administration of the drug has a stronger hypoglycemic effect in the first 6 hours after administration. In this regard, in some cases, adjustment of the insulin dose and/or diet may be required. Transferring a patient to a new type of insulin or an insulin preparation from another manufacturer must be carried out under strict medical supervision; Dose adjustment may be required. Patients switching to treatment with insulin aspart may require a dose change compared to the doses of previously used insulin preparations. If necessary, dose adjustment can be made already at the first administration of the drug or during the first weeks or months of treatment. In addition, a change in the dose of the drug may be required when changing the diet and with increased physical activity. Exercise performed immediately after eating may increase the risk of hypoglycemia. The drug should not be used in insulin pumps. Clinical experience with the use of insulin aspart during pregnancy is limited. Animal studies have shown no differences between the embryotoxicity and teratogenicity of insulin aspart and human insulin. During the period of possible pregnancy and throughout its entire duration, it is necessary to monitor the condition of patients with diabetes mellitus and monitor the concentration of glucose in the blood. The need for insulin, as a rule, decreases in the first trimester and gradually increases in the second and third trimesters of pregnancy. During and immediately after childbirth, insulin requirements may decrease sharply, but quickly return to pre-pregnancy levels. During lactation, it may be necessary to adjust the dose. Patients' ability to concentrate and reaction speed may be impaired with the development of hypoglycemia and hyperglycemia, which can pose a danger when driving or working with machinery. Patients should be advised to take measures to prevent the development of hypoglycemia and hyperglycemia when driving a car and working with machinery. This is especially important for patients with the absence or decrease in the severity of symptoms that are warning signs of developing hypoglycemia or with frequent episodes of hypoglycemia. In these cases, the feasibility of performing such work should be considered. Preparations containing the active substance Insulin aspart biphasic:
NovoMix 30 Penfill, NovoMix 30 FlexPen, NovoMix 50 FlexPen, NovoMix 70 FlexPen
The information provided in this section is intended for medical and pharmaceutical professionals and should not be used for self-medication. The information is provided for informational purposes only and cannot be considered official.