Cimzia®
Rheumatoid arthritis
In placebo-controlled and open-label studies, Cimzia® was administered to 4,049 patients with rheumatoid arthritis. The duration of treatment was up to 92 months.
In placebo-controlled studies, the duration of exposure to Cimzia® was 4 times greater than the duration of exposure in the placebo group. This difference is due to the higher dropout rate of patients in the placebo group. In addition, the RA-I and RA-II studies required attrition of patients who did not achieve a response at week 16, most of whom received placebo.
The proportion of patients who discontinued treatment due to adverse events during controlled trials was 4.4% among those receiving Cimzia® and 2.7% in the placebo groups.
The most frequently observed adverse reactions were those belonging to the group of “infections and infestations” - in 14.4% of patients receiving Cimzia® and in 8.0% of patients in the placebo group, “general disorders and reactions at the injection site” in 8. 8% of patients treated with Cimzia® and 7.4% on placebo, as well as “skin and subcutaneous tissue disorders” in 7.0% of patients treated with Cimzia® and 2.4% on placebo.
Crohn's disease
In patients with Crohn's disease in placebo-controlled studies, serious adverse events were observed in 10.8% of cases when treated with Cimzia®, and 8.6% in the placebo group. The most common adverse reactions were nasopharyngitis (11.1% and 6.7%, respectively), nausea (8% and 6.7%, respectively), urinary tract infections (5.1% and 4.4%, respectively) , abdominal pain (9.3% and 8.8%, respectively), arthralgia (6.7% and 3.9%, respectively), headache (14.8% and 13.8%, respectively).
Due to adverse reactions, 11.3% of patients receiving Cimzia® discontinued therapy and 12.6% of patients receiving placebo. In placebo-controlled clinical trials, the most common adverse reactions leading to discontinuation of Cimzia® or placebo were: diarrhea (0.5% and 0.2%, respectively), abdominal pain (0.9% and 0.4% , respectively) and nausea (0.4% and 0.2%, respectively).
Axial spondyloarthritis
Study AS001, a 4-year study that included a 24-week placebo-controlled phase followed by a 24-week dose-blind period and a 156-week open-label period, assessed the safety profile of Cimzia® in 325 patients with active axial spondyloarthritis. (including ankylosing spondylitis and non-radiographic axial spondylitis). Cimzia® was also studied in 317 patients with non-radiographic axial spondyloarthritis in a 52-week placebo-controlled study (AS0006). In both studies, the tolerability profile in patients with axial spondyloarthritis was consistent with that in rheumatoid arthritis and previous experience with Cimzia®.
Psoriatic arthritis
The 4-year PsAOOl study, which included a 24-week placebo-controlled phase followed by a 24-week dose-blind period and a 168-week open-label period, assessed the safety profile of Cimzia® in 409 patients with psoriatic arthritis. The safety profile of Cimzia® when used in patients with psoriatic arthritis was consistent with that in rheumatoid arthritis and previous experience with the drug.
Plaque psoriasis
The tolerability profile of Cimzia® was assessed in 1112 patients with psoriasis in controlled and open-label studies lasting up to 18 months. The safety profiles of different dosing regimens of Cimzia® (400 mg every 2 weeks and 200 mg every 2 weeks) were similar.
During the 16-week placebo-controlled study phases, serious adverse events occurred in 3.5% of patients receiving Cimzia® and in 3.7% of patients receiving placebo. The proportion of patients who discontinued treatment due to adverse events during controlled studies was 1.5% in patients receiving Cimzia® and 1.4% in patients receiving placebo.
The most common adverse reactions observed during the first 16 weeks of the study were those in the group of “infections and infestations” - in 6.1% of patients receiving Cimzia® and in 7% of patients in the placebo group, “general disorders and reactions at the injection site "in 4.1% of patients receiving the drug Cimzia®, and in 2.3% - placebo, as well as "disorders of the skin and subcutaneous tissue" in 3.5% of patients receiving the drug Cimzia®, and in 2.8 % - placebo.
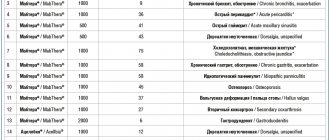
Adverse reactions are grouped by frequency of occurrence: very often (≥1/10); often (≥1/100, <1/10); uncommon (≥1/1000, <1/100); rare (≥1/10000, <1/1000); very rare (<1/10000); the frequency has not been established (it is impossible to estimate from the available data).
Infectious and parasitic diseases
: often - bacterial infections (including abscess), viral infections (including those caused by herpes virus, influenza virus, papillomavirus); uncommon - sepsis (including multiple organ failure and septic shock), tuberculosis (including miliary, disseminated and extrapulmonary), fungal infections (including opportunistic).
Benign tumors, malignant neoplasms and unspecified neoplasms (including cysts and polyps):
uncommon - malignant diseases of the blood and lymphatic system, including lymphoma and leukemia, solid organ tumors, non-melanocytic skin cancer, precancerous lesions (leukoplakia of the oral mucosa, melanocytic nevus), benign tumors and cysts (including skin papilloma); rarely - neoplasms of the gastrointestinal tract, melanoma.
Blood and lymphatic system disorders:
often - eosinophilia, leukopenia (including lymphopenia and neutropenia); uncommon - anemia, thrombocytopenia, lymphadenopathy, thrombocytosis; rarely - pancytopenia, splenomegaly, erythrocytosis, morphological changes in leukocytes.
Immune system disorders:
uncommon - vasculitis, SLE (systemic lupus erythematosus), increased drug sensitivity, including anaphylactic shock, allergic reactions, positive test for autoantibodies; rarely - angioedema, sarcoidosis, serum sickness, panniculitis (including erythema nodosum).
Endocrine system disorders:
rarely - dysfunction of the thyroid gland.
Metabolic and nutritional disorders
: infrequently - electrolyte disturbances, dyslipidemia, loss of appetite, changes in body weight; rarely - changes in plasma glucose concentration, hypoalbuminemia, hypoproteinemia, hemosiderosis.
Mental disorders:
uncommon - anxiety (including mental stress), mood changes (and associated symptoms); rarely - suicide attempts, delirium, decreased mental activity, aggression.
Nervous system disorders:
often - headache (including migraine), sensitivity disorders; uncommon - peripheral neuropathy, dizziness, tremor; rarely - demyelinating diseases, including neuritis of the cranial nerves, convulsions, extrapyramidal disorders, trigeminal neuralgia, impaired coordination of movements and sense of balance, dysphonia, mask-like facial expression, sleep disturbance.
Visual disorders
: uncommon - visual disturbances (including decreased visual acuity), inflammation of the eye and eyelid, impaired lacrimation.
Hearing and labyrinth disorders:
infrequently - vertigo, tinnitus.
Cardiovascular system disorders:
often - increased blood pressure; uncommon - cardiomyopathy, heart failure, coronary heart disease, arrhythmias (including atrial fibrillation (atrial fibrillation)), palpitations, hemorrhage, bleeding, venous thromboembolism (pulmonary embolism (PE), thrombophlebitis), fainting, decreased blood pressure, edema ( face, limbs), ecchymoses (hematomas, petechiae); rarely - pericarditis, atrioventricular block, shock, stroke, atherosclerosis, Raynaud's syndrome, livedo reticularis, telangiectasia.
Disorders of the respiratory system, chest and mediastinal organs:
uncommon - pleural effusion (and associated symptoms), bronchial asthma and its manifestations, shortness of breath, congestive and inflammatory changes in the lungs, cough; rarely - interstitial lung diseases, pneumonitis, ulceration of the nasal mucosa.
Gastrointestinal disorders:
often - nausea, vomiting; uncommon - ascites, symptoms of Crohn's disease (stenosis), ulcerative lesions and perforation (of various parts of the gastrointestinal tract), inflammation of the gastrointestinal mucosa, dyspepsia, stomatitis, bloating, dry mucous membrane of the oral cavity and pharynx; rarely - intestinal obstruction, painful swallowing, anal fissures, increased intestinal motility.
Disorders of the liver and biliary tract:
often - hepatitis, increased activity of liver enzymes; uncommon - liver diseases, including liver cirrhosis, cholestasis, increased concentration of bilirubin in the blood plasma; rarely - cholelithiasis.
Disorders of the skin and subcutaneous tissues:
often - rash; uncommon - alopecia, the onset of psoriasis or worsening of its symptoms (including palmoplantar pustular psoriasis), dermatitis, eczema, dysfunction of the sweat glands, skin ulcerations, increased photosensitivity, acne, skin pigmentation disorders, dry skin, lesions of the nail plate and nail box; rarely - acute febrile neutrophilic dermatosis, exfoliation and desquamation of the skin, bullous dermatitis, hair structure disorder, lichenoid reactions.
Musculoskeletal disorders:
infrequently - muscle disorders.
Urinary system disorders:
uncommon - renal dysfunction, hematuria, nephrolithiasis, urethritis, cystitis; rarely - nephropathy, nephritis.
Reproductive system and breast disorders:
uncommon - menstrual irregularities, uterine bleeding, amenorrhea, breast dysfunction, azoospermia; rarely - spontaneous abortion, vaginal discharge, sexual dysfunction, balanitis.
General disorders and reactions at the injection site:
often - hyperthermia, pain (unspecified localization), asthenia, itching (unspecified localization), reactions at the injection site; infrequently - chills, flu-like syndrome, impaired temperature sensitivity, night sweats, hot flashes; skin damage, slow wound healing; rarely - formation of fistulas (unspecified localization).
Laboratory and instrumental data:
uncommon - increased activity of creatinine phosphokinase (CPK), alkaline phosphatase, total bilirubin, increased blood clotting time, changes in general urinalysis; rarely - increased concentration of uric acid in the blood.
The following adverse reactions have been associated with the use of drugs from the TNF-α inhibitor class: Merkel cell carcinoma, multiple sclerosis, Guillain-Barré syndrome, but the frequency of their occurrence with the use of Cimzia® is unknown.
The following are rare
Adverse reactions are associated with the use of drugs from the class of TNF-α inhibitors: Stevens-Johnson syndrome, erythema multiforme, worsening symptoms of dermatomyositis.
Infections
In controlled studies in patients with rheumatoid arthritis , new cases of infectious diseases were observed at a rate of 1.03 cases per 1 patient-year in those treated with Cimzia® and with a rate of 0.92 cases per 1 patient-year in those receiving placebo. Infections were represented mainly by diseases of the upper and lower respiratory tract, diseases of the urinary system and herpetic diseases.
In placebo-controlled studies, there were more cases of serious infectious diseases in the group treated with Cimzia® (0.07 per 1 patient-year, across all dosing regimens) than in the placebo group (0.02 per 1 patient-year).
The most common serious infections were pneumonia and tuberculosis. There was no evidence of an increase in the risk of developing infections with increasing duration of use of the drug Cimzia®.
The incidence of infections in controlled studies in patients with Crohn's disease was 38.6% in patients treated with Cimzia® and 30.6% in patients treated with placebo. Infectious diseases of the respiratory tract were mainly observed (18.9% in patients treated with Cimzia® and 12.4% with placebo).
The incidence of clinically significant serious infections in controlled studies was 2.6% among those treated with Cimzia® and 1.3% with placebo. Serious infections included both bacterial and viral diseases, pneumonia, and pyelonephritis.
Incidence of new infections in placebo-controlled clinical trials of Cimzia® for psoriasis
was 1.37 per 1 patient-year in patients treated with Cimzia®, and 1.59 per 1 patient-year in patients treated with placebo. These were mainly upper respiratory tract infections and viral infections (including herpesvirus). The incidence of serious infections during the use of Cimzia® was 0.02 per patient-year. No serious infections were reported among patients receiving placebo. There was no evidence of an increase in the risk of developing infections with increasing duration of use of the drug Cimzia®.
Tuberculosis
The use of drugs from the TNF-α inhibitor group may be accompanied by the development of active tuberculosis. There are reports of severe and fatal cases of tuberculosis during treatment with Cimzia®. In completed and ongoing clinical studies for all known indications among 5118 patients treated with Cimzia®, the incidence of tuberculosis was approximately 0.61 per 100 patient-years. The greatest number of cases was observed in countries where tuberculosis is endemic. Reports have included cases of pulmonary, disseminated and extrapulmonary tuberculosis, as well as rare cases of opportunistic infections. Rare cases of tuberculosis and opportunistic infections have been fatal.
Malignant and lymphoproliferative diseases
In controlled studies of TNF-α inhibitors, more cases of malignancies, including lymphomas, were reported in the group of patients receiving TNF-α inhibitors compared with the control group.
121 malignancies (including 5 cases of lymphoma) were registered in clinical trials of Cimzia® in 4049 patients with rheumatoid arthritis In clinical studies of Cimzia® in patients with rheumatoid arthritis, the incidence of lymphoma in patients receiving Cimzia® was 0.05 per 100 patient-years, and the incidence of melanoma was 0.08 per 100 patient-years.
According to placebo-controlled and open phase clinical trials of the drug Cimzia® in patients with Crohn's disease and other indications, malignant neoplasms (except non-melanoma skin cancer) were observed with a frequency (95% confidence interval) of 0.5 (0.4 and 0.7 ) per 100 patient-years among 4650 patients treated with Cimzia®. However, the same rate in the placebo group was 0.6 (0.1 and 1.7) per 100 patient-years among 1319 patients. According to controlled clinical studies of 2657 patients treated with Cimzia® for Crohn's disease , 1 patient was diagnosed with lymphoma; Also, 1 case of lymphoma was observed in the control group of patients, which included 1319 people.
The incidence of malignancies, including lymphomas, in clinical trials of Cimzia® cannot be compared with the results of studies of other TNF-α inhibitors and cannot serve as a basis for predicting the incidence of these diseases when using Cimzia® in a wider patient population.
Patients with Crohn's disease who require long-term immunosuppressant therapy are at increased risk of developing lymphoma compared with the general population, even if they are not treated with TNF-α inhibitors.
In a clinical trial, lymphoma was diagnosed in one patient with psoriatic arthritis .
Excluding non-melanoma skin cancer, in clinical trials of Cimzia® involving 1112 patients with psoriasis (1481 patient-years), 9 malignancies were reported, including 1 case of lymphoma.
Chronic heart failure
During treatment with Cimzia®, both new cases of CHF and progression of previously existing symptoms of CHF were noted. Most of these cases were mild or moderate in severity and were diagnosed within the first year of treatment with the drug.
Immunogenicity
Rheumatoid arthritis
The total number of patients with rheumatoid arthritis with antibodies to Cimzia®, which were determined at least once, was 9.6% in placebo-controlled studies of the drug. In approximately 1/3 of these patients, the antibodies exhibited neutralizing activity in vitro.
Patients who were simultaneously taking immunosuppressants (methotrexate) had a lower rate of antibody formation than patients who were not initially receiving them. Antibody formation was associated with lower plasma concentrations of Cimzia® and, in some patients, with lower efficacy.
Crohn's disease
In Crohn's disease, antibodies to the drug were detected in 8% of patients receiving long-term treatment with Cimzia®. In approximately 6% of them, the antibodies showed neutralizing activity in vitro. There is no obvious relationship between the formation of antibodies and the effectiveness of Cimzia®. In patients who were simultaneously taking immunosuppressants, the rate of antibody formation was lower than in patients who were not taking them (3% and 11%, respectively).
Axial spondyloarthritis
The overall percentage of patients who had at least one antibody response to Cimzia by week 24 was 4.4% in the placebo-controlled phase III AS001 study in patients with axial spondyloarthritis (ankylosing spondylitis and non-radiological axial spondylitis). spondyloarthritis). Antibody formation was associated with decreased plasma concentrations of the drug.
Throughout the study (up to week 192), the overall percentage of patients with antibodies to Cimzia® measured at least once was 9.6% (4.8% had transient antibodies, and another 4.8% had antibodies to Cimzia® were always present). The overall percentage of patients with antibodies who experienced a decrease in plasma drug concentrations was 6.8%.
Psoriatic arthritis
The total number of patients with psoriatic arthritis in the placebo-controlled study in whom antibodies to Cimzia® were detected at least once during 24 weeks was 11.7%. Antibody formation was associated with lower plasma drug concentrations. The number of patients with antibodies to Cimzia® was insufficient to provide a definitive assessment of the relationship between antibody titer and drug efficacy.
Plaque psoriasis
In phase III placebo-controlled studies, the proportion of patients with antibodies to Cimzia® measured at least once during treatment up to 48 weeks was 8.3% (22/265) and 19.2% (54/281) when using the drug Cimzia® at a dose of 400 mg every 2 weeks or 200 mg every 2 weeks, respectively. In the CIMPASI-1 and CIMPASI-2 studies, antibodies were detected in 60 patients, in 27 of whom they had neutralizing activity. Antibody formation has been associated with decreased plasma drug concentrations and, in some patients, decreased efficacy.
For all indications
The above data, reflecting the percentage of patients whose ELISA test results for antibodies to Cimzia® were considered positive, largely depend on the sensitivity and specificity of the method. In addition, several factors may influence the observed incidence of antibody formation, including sampling method (specimen handling), timing of blood sample collection, concomitant medications used, and the nature of the underlying disease. For these reasons, comparison of the frequency of formation of antibodies to the drug Cimzia® with the frequency of formation of antibodies to other TNF-α inhibitors is not correct.
Non-radiological ax-SpA
In a placebo-controlled study in patients with non-radiographic axial spondyloarthritis, using a test method that was more sensitive and less dependent on the presence of drug in the blood compared to the previously used method, the total number of patients in whom antibodies to certolizumab pegol was 97% (248 of 255 patients). Only the highest antibody titers were associated with decreased plasma levels of certolizumab pegol, but no effect on efficacy was observed. Of patients who tested positive for antibodies to certolizumab pegol at least once, approximately 22% (54 of 248) had antibodies classified as neutralizing.
Autoantibody formation
In clinical studies, the formation of antinuclear antibodies (ANA) was observed in 4% of patients with Crohn's disease treated with Cimzia® and 2% of patients treated with placebo. In studies of TNF-α inhibitors, including Cimzia®, the formation of antinuclear antibodies (ANA) has also been observed in selected patients with rheumatoid arthritis. In clinical studies of Cimzia® for rheumatoid arthritis and Crohn's disease, some patients experienced the development of symptoms similar to lupus-like syndrome. The effect of long-term treatment with Cimzia® on the development of autoimmune diseases is unknown.
Hypersensitivity reactions
In rare cases, the following symptoms are observed that are similar to hypersensitivity reactions after administration of the drug Cimzia®: angioedema, allergic dermatitis, itchy rash, shortness of breath, hot flashes, decreased blood pressure, reactions at the injection site, feeling of malaise, hyperthermia, rash, serum sickness and fainting.
Reactions at the injection site
In some patients, during treatment with Cimzia®, the following reactions were observed at the injection site: erythema, itching, subcutaneous hematoma, pain, swelling or bruising.
There were no cases of drug withdrawal due to the development of local reactions.
Increased activity of creatine phosphokinase (CPK)
The incidence of increased CPK activity in patients with axial spondyloarthritis (axSpA) was generally higher than in the population of patients with rheumatoid arthritis (RA). This incidence was higher in both indications (axSpA and RA), both in those receiving placebo (2.8% and 0.4%, respectively) and in those receiving Cimzia® (4.7% and 0.8%, respectively). ).
The increase in CPK in patients with axSpA was in most cases transient, clinically insignificant, and was not the reason for discontinuation of the drug in any patient.
Experience with the use of secukinumab in the treatment of severe resistant psoriasis
Improving the treatment of psoriasis vulgaris (VP) remains an important medical and social problem, which is associated with the persistently high incidence of this dermatosis in the Russian Federation and the chronic relapsing course of the disease. In recent years, there has been an increase in the formation of severe, disabling forms of the disease, the torpidity of the process and the ineffectiveness of standard therapeutic approaches are observed, and the formation of iatrogenic complications is recorded [1, 2].
General approaches to the treatment of psoriasis (Ps), taking into account the characteristics of the clinical forms and manifestations of the disease, the severity of the process and comorbid pathology, are presented in domestic clinical recommendations, in the guidelines for the treatment of psoriasis of European countries and the European Academy of Dermatology and Venereology (European Academy of Dermatology and Venereology, EADV) [3, 4].
The most difficult task is the treatment of patients with moderate and severe psoriasis, in whom almost half of the cases have psoriatic joint damage, manifested in the formation of distal arthritis, enthesitis, and dactylitis; mono- or polyarthritis, spondylitis [3, 5].
Patients with moderate and severe manifestations of psoriasis are considered to be those who have widespread skin rashes, characterized by severe inflammatory infiltration, peeling in patches, itching of the skin, when the standardized PASI psoriasis severity index is more than 10–12 points, “problem” areas are affected - the face, neck , scalp, anogenital area; The quality of life of patients is critically reduced. It is for such patients, in addition to the existing pathogenetically oriented methods of therapy using pharmacological agents with anti-inflammatory, immunosuppressive, absorbable effects, and the use of photo- and photochemotherapy methods, that genetically engineered biological preparations (GEBPs) have been developed and are widely used - monoclonal antibodies with high affinity to the determinants of activated lymphocytes and circulating cytokines, neutralizing their influence and interrupting the process of psoriatic plaque formation [2, 3, 6].
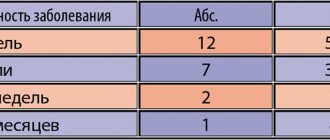
The introduction of biologically active drugs into clinical practice over the past decade has led to a significant paradigm shift in the treatment of psoriasis and psoriatic arthritis (PsA) as chronic inflammatory diseases that require long-term therapy to maintain an effective clinical response. Long-term use of biologically active drugs with immunosuppressive effects for the treatment of patients with PS and PsA involves the assessment of a complex of factors, including the degree of effectiveness of treatment, its stability, the possibility of the formation of adverse events associated with the formation of anti-drug antibodies, potential dangers associated with a decrease in the activity of the immune response to infectious agents and during the development of neoplasia [4, 7]. For these purposes, the indicator “drug survival” is used, that is, through long-term observation, the period during which the patient remains on this type of therapy is established.
For a number of years, a comprehensive assessment of the effectiveness, safety and outcomes of therapy for patients with PS and PsA has been carried out within the framework of the global international prospective, observational study PSOLAR (Psoriasis Longitudinal Assessment and Registry), which brings together more than 12 thousand patients with PsA receiving systemic, including genetically engineering biological therapy (GEBT). Studies have shown that GEBD are effective in the initial stage of treatment of the disease, but the clinical response decreases over time and even with modification of therapy, ultimately leading to suspension of therapy or switching to GEBT of a different mechanism of action [8, 9]. At the same time, a shorter period of “drug survival” was established for the class of TNF blockers than for a drug that inhibits the cytokines IL-12/23 [8].
The possibility of switching from one GIBT to another if the effect “eludes” or if contraindications or adverse events appear is described in a number of publications summarizing the use of GIBT in real clinical practice, and allows for a wide variety of switching options both within one class of drugs and between them [8 , 10, 11]. In domestic clinical practice, most often, initial therapy for PS and PsA is carried out using anti-TNF-α drugs (infliximab, adalimumab, etanercept); if effectiveness is lost, treatment with ustekinumab is prescribed [2].
In the State Budgetary Institution SO UrNIIDVII, treatment of patients with severe, resistant forms of psoriasis and psoriatic arthritis with the use of biologically active drugs has been carried out since 2006, over a 10-year period more than 2200 administrations of biological drugs were carried out.
In the period until 2013, GIBT was provided to citizens of the Russian Federation within the framework of high-tech medical care (HTMC) in the “dermatovenereology” profile from the federal budget. Type of assistance 05.00.002 - treatment of severe, resistant forms of psoriasis, including psoriatic arthritis, with the use of biologically active drugs. During the specified period, 135 patients received treatment with the GEBD infliximab at the State Budgetary Institution SO UrNIIDVII.
From 2014 to the present, residents of the Sverdlovsk region receive GIBT as part of the VMP, included in the basic compulsory health insurance (CHI) program. One type of such assistance is the treatment of patients with severe resistant forms of psoriasis using genetically engineered biological drugs and treatment using genetically engineered biological drugs in combination with immunosuppressive drugs. Total for the period 2014–2016. 25 patients were treated under VMP in compulsory medical insurance.
In addition, since 2014, the order of the Ministry of Health of the Soviet Union has defined additional measures and schemes for providing medical care to patients with severe, widespread, torpid forms of psoriasis using genetically engineered pharmaceuticals. For this purpose, clinical and statistical groups (CSGs) have been identified to provide specialized medical care to patients in a day hospital, taking into account the specific GIBD, the frequency of its administration and cost. Currently, 16 patients annually receive this type of medical care at the State Budgetary Institution SO UrNIIDVII, of which 2 (12.5%) receive etanercept, 4 (25.0%) ustekinumab and 12 (75.0%) adalimumab. A 100% examination carried out by the Territorial Compulsory Medical Insurance Fund, which included control of the volume, timing, quality and conditions of medical care in the State Budgetary Institution SO UrNIIDVII, revealed shortcomings in less than 0.2% of cases; There are no penalties.
Since 2022, together with the territorial compulsory medical insurance fund, work has been carried out to change and supplement the DRG (subgroups) taking into account the registration in the Russian Federation of new and expansion of indications for already registered biological medications, which will increase the volume of specialized medical care for patients with severe forms of psoriasis, torpid to traditional ones and reserve methods of therapy.
Since July 2016, a new biologically active drug, secukinumab (Cosentyx), has been registered in the Russian Federation. Secukinumab is a fully human antibody immunoglobulin G1 (IgG1), which specifically inhibits the pro-inflammatory cytokine interleukin-17A (IL-17A), reduces the degree of its interaction with IL-17 receptors, which are expressed by activated lymphocytes, keratinocytes and synoviocytes, which determine the development of the psoriatic process, that is, it provides a selective effect on the key cause of the development of symptoms of psoriasis and psoriatic arthritis [12, 13]. Clinical studies of the drug secukinumab have shown that it provides a rapid onset of clinical effect with a decrease in the severity of inflammation and infiltration of psoriatic plaques already in the third week of treatment; Therapy of patients with psoriasis with Cosentyx for 4 years determines the state of “clear” or “almost clear” skin in the vast majority of patients, achieving PASI 90 in 8 out of 10 patients and PASI 100 in 4 out of 10 patients with psoriasis [14, 15]. In patients with PsA, secukinumab provides a rapid onset of clinical effect after the first week of treatment; in 84% of patients, it determines the absence of radiological progression of structural joint damage within 2 years; promotes active regression of enthesitis and dactylitis by 70% and 80%, respectively [16, 17].
Cosentyx demonstrates a favorable safety profile both in clinical studies and in real clinical practice in patients with psoriasis and psoriatic arthritis. The most common adverse events are upper respiratory tract infections (nasopharyngitis and rhinitis); the drug has low immunogenicity (< 1% of cases, the formation of non-neutralizing antibodies to secukinumab was observed), which does not affect its effectiveness [18]. Cosentyx demonstrated high efficacy both in “bionaive” patients with PS and PsA, and when used in patients who had previously received GEBD. Important are the results of comparative clinical studies that showed the superior effectiveness of secukinumab over etanercept both in the short and long term (at 4 and 52 weeks of observation), as well as higher efficiency than ustekinumab (~20%) in level of achieving PASI 90 within 52 weeks of treatment [15, 19].
In this article, we present the first clinical observation of effective therapy with an IL-17A blocker (secukinumab) in a patient with severe, treatment-resistant PS and PsA.
Clinical case
Patient V., born in 1960, resident of Yekaterinburg, music teacher. Diagnosis: widespread papular and plaque non-seasonal psoriasis, partial erythroderma, torpid often relapsing course, resistant to traditional, including cytostatic methods of therapy. Psoriatic peripheral polyarthritis, high-grade spondylitis.
Concomitant diagnoses: arterial hypertension stage II, stage 2, risk group 3. Iron deficiency anemia.
I have been suffering from psoriasis for more than 30 years. The onset of the disease is not associated with anything. The diagnosis was established at the first visit, by a dermatologist at the place of residence. The process immediately acquired a widespread, often recurrent course, with exacerbations occurring out of season. She was constantly monitored and received outpatient treatment from a dermatologist at her place of residence (standard methods of therapy). After 3 years from the onset of the disease, the skin process acquired a continuously relapsing character. She repeatedly received treatment in the UrNIIDVII hospital (cytostatic therapy with methotrexate, PUVA therapy), but it was not possible to achieve stable remission. Since 2003, lesions of peripheral joints have appeared. She was constantly observed by a rheumatologist, received outpatient and inpatient treatment: methotrexate, plasmapheresis, pulse therapy with prednisone, without a pronounced effect, but with the formation of persistent intolerance to methotrexate. From 2005 to 2006, she received immunosuppressive therapy with cyclosporine with good effect on both skin and joint processes. However, due to the development of side effects (hypertension), the drug was discontinued, after which a deterioration in skin and joint processes was noted.
Considering the severity of the clinical manifestations of dermatosis, reluctance to previous treatment methods, the continuously relapsing course of the disease, and significant joint damage, the patient received therapy with infliximab at a dose of 300 mg every 8 weeks in the period 2007–2011. Against the background of GIBT, drug remission of the disease was achieved, however, during the fourth year of therapy, a gradual increase in resistance to the drug was observed, and due to a decrease in its effectiveness, the drug was discontinued.
After stopping the administration of biologically active drugs, a sharp deterioration in skin and joint processes was noted, which again acquired a continuously relapsing off-season course. Outpatient therapy (methotrexate, topical glucocorticosteroids, non-steroidal anti-inflammatory drugs) was without effect, there was poor tolerability of cytostatic therapy with the development of dyspeptic disorders, abnormalities in the biochemical hepatogram, and the psoriatic process progressed. In this regard, since 2014, the patient was treated with ustekinumab according to the standard regimen as a basic staged HIBT. The therapy was tolerated well, without complications or side effects, however, from June 2016, after the 7th administration of the drug, there was a significant decrease in the effectiveness of this method of therapy: the appearance of fresh psoriatic rashes, increased pain and swelling of peripheral joints.
It was stated that in this patient the psoriatic process was characterized by a particularly severe course with pronounced clinical manifestations and a continuously relapsing nature, was resistant to standard methods of systemic therapy, and treatment with GIBD, carried out with anti-TNF and anti-IL-12/23 drugs, demonstrated action effective only for a limited time.
By the decision of the medical commission of the State Budgetary Institution Siberian UrNIIDVII, the patient was started on therapy with a gastrointestinal biological agent - secukinumab.
Before starting this therapy:
Status localis. The skin process is common, localized on the skin of the face, scalp, torso, flexor and extensor surfaces of the extremities. It is represented by many numular papules and plaques up to 20.0 cm in diameter with unclear boundaries, moderately and heavily infiltrated. On the surface of the rash there is a mass of scales, tightly fitting, white. Peeling is medium-plate, abundant. The psoriatic triad is positive, pronounced isomorphic Koebner reaction. Dermographism pink. PASI index - 51.5 points. The nail plates are completely affected - with areas of subungual hyperkeratosis, a symptom of an “oil stain”. The volume of active and passive joints of the hands, feet, cervical spine, right elbow, and knee joints is limited. The joints are swollen and hot to the touch. O deformity, axial arthritis, dactylitis and “sausage-shaped” deformity of the fingers and toes (Fig. 1).
Before the start of therapy, a general clinical blood test: red blood cells 3.97 × 1012/l, hemoglobin 95 g/l, leukocytes 6.0 × 109/l, neutrophils 71.7%, lymphocytes 17.4%, eosinophils 3.1%, monocytes 7.2%, ESR 40 mm/hour. General urine test, biochemical hepatogram - no abnormalities.
X-ray examination of the lungs in two projections - without pathology, the patient was consulted by a phthisiatrician, tuberculosis was excluded.
The drug secukinumab is prescribed at a dose of 300 mg, according to the instructions for use of the drug in the form of subcutaneous injections. The initial course was 5 weeks with weekly administration of secukinumab. Subsequently, therapy was continued in the form of monthly subcutaneous injections.
During therapy, already on the 3rd day after the first administration of the drug secukinumab, positive dynamics were noted in both skin and joint processes. In Fig. Figure 2 shows the patient on the 7th day of therapy.
After carrying out the initiating course for 5 weeks, almost complete regression of the rash was noted, the PASI index was 0 (Fig. 3).
When the course of treatment with secukinumab is continued for up to 24 weeks, the state of clinical remission of the skin process is maintained, joint symptoms are minimal, quality of life is completely restored, and the patient has returned to professional activities (Fig. 4).
Treatment with secukinumab was well tolerated; there were no adverse events; laboratory monitoring of the hemogram and biochemical hepatogram in the dynamics of treatment did not reveal any deviations.
Discussion
In everyday clinical practice, there are frequent cases of the development of severe forms of PS and PsA in young and middle-aged people, when the process has a continuously recurrent course, critically reduces the quality of life and determines long-term disability. Therapy for such patients is carried out with systemic pathogenetically oriented drugs that have anti-inflammatory and immunosuppressive effects with alternating agents and treatment methods: phototherapy and its combined variants, photochemotherapy, methotrexate, retinoids, cyclosporine, biologically active drugs [3, 4]. However, even after using the entire available arsenal of treatments, there remain patients who cannot control PS and PsA at an acceptable level.
Promising for such a cohort of patients is the use of new, targeted, highly effective and safe drugs, which include the IL-17A blocker drug secukinumab, and for dermatovenereologists it is extremely important to accumulate and generalize their own positive clinical experience.
Conclusion
The presented observation demonstrates the high clinical effectiveness of the drug Cosentyx (secukinumab) in the treatment of a patient with extremely severe PS and PsA, who has developed resistance to standard methods of systemic therapy, secondary ineffectiveness of monoclonal antibodies to TNF-α and IL-12/23. The achieved rapid and stable treatment effect over 6 months (PASI 100) indicates the rationality of the use of secukinumab in complex clinical situations, the need for wider introduction of the drug into domestic clinical practice, which will help quickly improve the course of the disease and the quality of life of patients suffering from moderate and severe psoriasis and psoriatic arthritis.
Literature
- Kubanova A. A., Kubanov A. A., Melekhina L. E., Bogdanova E. V. Organization of medical care in the “dermatovenereology” profile in the Russian Federation. Dynamics of incidence of sexually transmitted infections, diseases of the skin and subcutaneous tissue, 2013–2015. // Bulletin of dermatology and venereology. 2016; (3): 12–28.
- Kungurov N.V., Kokhan M.M., Keniksfest Yu.V. Biological therapy of patients with severe forms of psoriasis // Bulletin of Dermatology and Venereology. 2012; 4:91–95.
- Federal clinical guidelines. Dermatovenereology 2015: Skin diseases. Sexually transmitted infections. 5th ed., revised. and additional M.: Business Express, 2016. 768 p.
- Nast A., Gisondi P., Ormerod AD, Saiag P., Smith C. et al. European S3-Guidelines on the systemic treatment of psoriasis vulgaris. Update 2015. Short version. EDF in cooperation with EADV and IPC // JEADV. 2015; 29:2277–2294.
- Korotaeva T.V., Nasonov E.L., Molochkov V.A. The use of methotrexate in the treatment of psoriasis and psoriatic arthritis // Modern Rheumatology. 2013; 2:1–8.
- Kungurov N.V., Kokhan M.M., Keniksfest Yu.V., Filimonkova N.N. Immunosuppressive and biological therapy of patients with severe forms of psoriasis // Bulletin of Ural Medical Science. 2011; 2 (2): 35–39.
- Knud Kragballe K., van de Kerkhof PCM, Gordon KB Unmet needs in the treatment of psoriasis // Eur J Dermatol. 2014; 24(5):523–532.
- Menter A., Papp KA, Gooderham M., Pariser DM, Augustin M. Drug survival of biological therapy in a large, disease-based registry of patients with psoriasis: results from the Psoriasis Longitudinal Assessment and Registry (PSOLAR) // JEADV. 2016; 30: 1148–1158.
- Davila-Seijo P., Dauden E., Carretero G., Ferrandiz C., Vanaclocha F. Survival of classic and biological systemic drugs in psoriasis: results of the BIOBADADERM registry and critical analysis // JEADV. 2016; 30: 1942–1950.
- Inzinger M., Wippel-Slupetzky K., Weger W., Richter L., Mlynek A. et al. Survival and Effectiveness of Tumor Necrosis Factor-alpha Inhibitors in the Treatment of Plaque Psoriasis under Daily Life Conditions: Report from the Psoriasis Registry Austria // Acta Derm Venereol. 2016; 96:207–212.
- Mrowietz U., de Jong EMGJ, Kragballe K., Langley R., Nast A., Puig L., Reich K. A consensus report on appropriate treatment optimization and transitioning in the management of moderate-to-severe plaque psoriasis // JEADV . 2014; 28:438–453.
- Langley R., Elewski B.E., Lebwohl M. et al. Secukinumab in plaque psoriasis — results of two phase 3 trials // N Engl J Med. 2014; 371:326–338.
- Mansouri Y., Goldenberg G. New Systemic Therapies for Psoriasis // Cutis. 2015; 95 (3): 155–160.
- Blauvelt A., Prinz JC, Gottlieb AB et al. Secukinumab administration by pre-filled syringe: efficacy, safety, and usability results from a randomized controlled trial in psoriasis. (FEATURE) // Br J Dermatol. 2015; 172:484–493.
- Thaçi D., Blauvelt A., Reich K., Tsai TF, Vanaclocha F., Kingo K. et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial // J Am Acad Dermatol. 2015; 73:400–409.
- Mease PJ, McInnes IB, Kirkham B. et al. FUTURe 1 Study Group. Secukinumab inhibition of interleukin-17A in patients with psoriatic Arthritis // N Engl J Med. 2015; 373(14):1329–1339.
- McInnes IB, Mease PJ, Kirkham B. et al. FUTURe 2 Study Group. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURe 2): a randomized, double blind, placebo-controlled, phase 3 trial // Lancet. 2015; 386:1137–1146.
- Van de Kerkhof PC, Griffiths CE, Reich K., Leonardi CL, Blauvelt A. et al. Secukinumab long-term safety experience: A pooled analysis of 10 phase II and III clinical studies in patients with moderate to severe plaque psoriasis // J Am Acad Dermatol. 2016; 75(1):83–98.
- Strober B., Gottlieb AB, Sherif B., Mollon P., Gilloteau I. et al. Secukinumab sustains early patient-reported outcome benefits through 1 year: Results from 2 phase III randomized placebo-controlled clinical trials comparing secukinumab with etanercept // J Am Acad Dermatol. 2017; 76(4):655–661.
N. V. Kungurov, Doctor of Medical Sciences, Professor N. V. Zilberberg, Doctor of Medical Sciences M. M. Kokhan1, Doctor of Medical Sciences, Professor Yu. V. Keniksfest, Doctor of Medical Sciences E. V. Grishaeva, Candidate of Medical Sciences
GBU SO UrNIIDVII, Yekaterinburg
1 Contact information
Experience with the use of the drug secukinumab in the treatment of severe resistant psoriasis / N.V. Kungurov, N.V. Zilberberg, M.M. Kokhan, Yu.V. Keniksfest, E.V. Grishaeva.
For citation: Attending physician No. 11/2017; Page numbers in issue: 17-23 Tags: skin diseases, dermatosis, arthritis, secukinumab
Cimzia, 200 mg/ml, solution for subcutaneous administration, 1 ml, 2 pcs.
Rheumatoid arthritis
The most frequently observed adverse reactions were those belonging to the group of “infections and infestations” - in 14.4% of patients receiving Cimzia® and in 8.0% of patients in the placebo group, “general disorders and reactions at the injection site” in 8.8 % of patients treated with Cimzia® and 7.4% with placebo, as well as “skin and subcutaneous tissue disorders” in 7.0% of patients treated with Cimzia and 2.4% with placebo.
Therapy was discontinued due to the development of adverse events in 4.4% of patients receiving Cimzia® and in 2.7% of patients not receiving the drug (placebo group).
Crohn's disease
In patients with Crohn's disease
in controlled studies, serious adverse events were noted in 10.8% of cases treated with Cimzia®, and in the placebo group - in 8.6%.
The most common adverse reactions were nasopharyngitis (11.1% and 6.7%, respectively), nausea (8% and 6.7%, respectively), urinary tract infections (5.1% and 4.4%, respectively) , abdominal pain (9.3% and 8.8%, respectively), arthralgia (6.7% and 3.9%, respectively), headache (14.8% and 13.8%, respectively).
Due to adverse reactions, 11.3% of patients receiving Cimzia® discontinued therapy and 12.6% of patients receiving placebo. The most common adverse reactions leading to discontinuation of Cimzia® were: diarrhea (0.5% and 0.2%, respectively), abdominal pain (0.9% and 0.4%, respectively) and nausea (0. 4% and 0.2%, respectively).
Axial spondyloarthritis
A placebo-controlled study assessed the safety profile in 325 patients with active axial spondyloarthritis
who received the drug Cimzia® for up to 30 months. The safety profile of the drug Cimzia® when used in patients with axial spondyloarthritis was consistent with that in patients with rheumatoid arthritis and previous experience with the drug.
Psoriatic arthritis
A placebo-controlled study assessed the safety profile in 409 patients with psoriatic arthritis
who received the drug Cimzia® for up to 30 months.
Safety profile of the drug Cimzia® when used in patients with psoriatic arthritis
corresponded to that in patients with rheumatoid arthritis and previous experience with the drug.
Adverse reactions are grouped by frequency of occurrence: very often (≥1/10); often (≥1/100, <1/10); uncommon (≥1/1000, <1/100); rare (≥1/10000, <1/1000); very rare (<1/10000); the frequency has not been established (it is impossible to estimate from the available data).
Infectious and parasitic diseases: often
- bacterial infections (including abscess), viral infections (including those caused by herpes virus, influenza virus, papillomavirus);
uncommon
- sepsis (including multiple organ failure and septic shock), tuberculosis, fungal infections (including opportunistic).
Benign tumors, malignant neoplasms and unspecified neoplasms (including cysts and polyps): uncommon
- malignant diseases of the blood and lymphatic system, including lymphoma and leukemia, solid neoplasms, malignant neoplasms of the skin that do not include melanoma, precancerous lesions (leukoplakia of the oral mucosa, melanocytic nevus), benign tumors and cysts (including skin papilloma);
rarely
- neoplasms of the gastrointestinal tract, melanoma.
Blood and lymphatic system disorders: common
- eosinophilia, eosinopenia, leukopenia (lymphopenia and neutropenia);
uncommon
- anemia, thrombocytopenia, lymphadenopathy, thrombocytosis;
rarely
- pancytopenia, splenomegaly, erythrocytosis, morphological changes in leukocytes.
Immune system disorders: uncommon
- vasculitis, SLE (systemic lupus erythematosus), increased drug sensitivity, psoriasis and related diseases, allergic disorders, positive reaction to autoantibodies;
rarely
- angioedema, sarcoidosis, serum sickness, panniculitis (including erythema nodosum).
Endocrine system disorders: rare
- dysfunction of the thyroid gland.
Metabolic and nutritional disorders: uncommon
- electrolyte disturbances, dyslipidemia, loss of appetite, changes in body weight;
rarely
- changes in plasma glucose concentration, hypoalbuminemia, hypoproteinemia, hemosiderosis.
Mental disorders: uncommon
- anxiety (including mental stress), mood changes (and related symptoms);
rarely
- suicide attempts, delirium, decreased mental activity, aggression.
Nervous system disorders: common
- headache (including migraine), sensory disturbances;
uncommon
- peripheral neuropathy, dizziness, tremor, optic neuritis;
rarely
- demyelinating diseases, including cranial neuritis, seizures, extrapyramidal disorders, trigeminal neuralgia, impaired coordination of movements and sense of balance, dysphonia, mask-like facial expression, sleep disturbance.
Visual disturbances: uncommon
- impaired visual perception (including decreased visual acuity), uveitis and blepharitis, dacryoadenitis and dacryocystitis.
Hearing and labyrinthine disorders: uncommon
- vertigo, tinnitus;
rarely
- hearing loss.
Cardiovascular disorders: common
- increased blood pressure;
uncommon
- cardiomyopathy, heart failure, coronary heart disease, arrhythmias (including atrial fibrillation (atrial fibrillation)), palpitations, hemorrhage, bleeding, venous thromboembolism (PE, thrombophlebitis), fainting, decreased blood pressure, edema (face, extremities), ecchymoses (hematomas, petechiae);
rarely
- pericarditis, atrioventricular block, shock, stroke, atherosclerosis, Raynaud's syndrome, livedo reticularis, telangiectasia.
Respiratory, thoracic and mediastinal disorders: uncommon
- pleural effusion (and associated symptoms), bronchial asthma and its manifestations, shortness of breath, congestive and inflammatory changes in the lungs, cough;
rarely
- interstitial lung diseases, pneumonitis, ulceration of the nasal mucosa.
Gastrointestinal disorders: common
- nausea, vomiting;
uncommon
- ascites, symptoms of Crohn's disease (stenosis), ulcerative lesions and perforation (of various parts of the gastrointestinal tract), inflammation of the gastrointestinal mucosa, dyspepsia, stomatitis, bloating, dry mucous membrane of the oral cavity and pharynx;
rarely
- intestinal obstruction, painful swallowing, anal fissures, increased intestinal motility.
Liver and biliary tract disorders: common
- hepatitis, increased activity of liver enzymes;
uncommon
- liver diseases, including liver cirrhosis, cholestasis, increased concentration of bilirubin in the blood plasma;
rarely
- cholelithiasis.
Skin and subcutaneous tissue disorders: common
- rash;
uncommon
- alopecia, the onset of psoriasis or worsening of its symptoms, dermatitis, eczema, dysfunction of the sweat glands, skin ulcerations, increased photosensitivity, acne, skin pigmentation disorders, dry skin, lesions of the nail plate and nail bed;
rarely
- acute febrile neutrophilic dermatosis, exfoliation and desquamation of the skin, bullous dermatitis, skin ulcerations, pityriasis rosea, stretch marks, rosacea, hair structure disorder.
Musculoskeletal disorders: uncommon
- arthritis, muscle dysfunction;
rarely
- dysfunction of the tendons.
Urinary system disorders: uncommon
- impaired renal function, hematuria, nephrolithiasis, urethritis, cystitis;
rarely
- nephropathy, nephritis.
Reproductive system and breast disorders: uncommon
- menstrual irregularities, uterine bleeding, amenorrhea, breast dysfunction, azoospermia;
rarely
- premature birth, vaginal discharge, sexual dysfunction, balanitis.
General disorders and reactions at the injection site: often
- hyperthermia, pain (unspecified localization), asthenia, itching (unspecified localization), reactions at the injection site;
uncommon
- formation of fistulas (without specifying the location), chills, flu-like syndrome, impaired temperature sensitivity, night sweats, hot flashes; skin damage, slow wound healing.
Laboratory and instrumental data: uncommon
- increased activity of creatinine phosphokinase (CPK), alkaline phosphatase, total bilirubin, increased blood clotting time, changes in general urinalysis;
rarely
- increased concentration of uric acid in the blood.
The following adverse reactions have been associated with the use of drugs from the TNF-α antagonist class: Merkel cell carcinoma, multiple sclerosis, Guillain-Barré syndrome, but the frequency of their occurrence with the use of Cimzia® is unknown.
Infections
In controlled studies in patients with rheumatoid arthritis
new cases of infectious diseases were observed at a rate of 1.03 patients per year in those treated with Cimzia® and at a rate of 0.92 patients per year in those receiving placebo. Infections were represented mainly by diseases of the upper and lower respiratory tract, diseases of the urinary system and viral herpetic diseases.
In controlled studies, there were more cases of serious infectious diseases in the group treated with Cimzia® (0.07 patients per year) than in those treated with placebo (0.02 patients per year). The most common serious infectious diseases were pneumonia and tuberculosis. There is no increase in the risk of infections with increasing duration of use of the drug Cimzia®.
Incidence of infections in controlled studies in patients with Crohn's disease
was 38.6% in those treated with Cimzia® and 30.6% in patients treated with placebo. Infectious diseases of the respiratory tract were mainly observed (18.9% in patients treated with Cimzia® and 12.4% with placebo). The incidence of clinically significant serious infections in controlled studies was 2.6% of patients per year among those treated with Cimzia® and 1.3% with placebo. Serious infections included both bacterial and viral diseases, pneumonia, and pyelonephritis.
Tuberculosis
The use of drugs from the TNF-α inhibitor group may be accompanied by the development of active tuberculosis. There are reports of severe and fatal cases of tuberculosis during treatment with Cimzia®. In completed and ongoing clinical studies for all known indications among 5118 patients treated with Cimzia®, the incidence of tuberculosis was approximately 0.61 per 100 patients per year. The greatest number of cases was observed in countries where tuberculosis is endemic. Reports have included cases of pulmonary and disseminated tuberculosis and, in rare cases, opportunistic infections. Rare cases of death have been reported in patients with tuberculosis and opportunistic infections.
Malignant and lymphoproliferative diseases
In controlled studies of TNF-α inhibitors, more cases of malignancy and lymphoma were reported in the group of patients receiving Cimzia® compared to the control group.
Of 4049 patients with rheumatoid arthritis
who received the drug Cimzia®, lymphoma was diagnosed in 5 patients. Patients with rheumatoid arthritis, especially those with severe disease activity, are at increased risk of developing lymphoma.
Of 2657 patients treated with Cimzia® for Crohn's disease
, 1 patient was diagnosed with lymphoma; Also, 1 case of lymphoma was observed in the control group of patients, which included 1319 people.
The incidence of malignancy and lymphoma in clinical studies of Cimzia® cannot be compared with the results of studies of other TNF-α inhibitors and cannot serve as a basis for predicting the incidence of these diseases when using Cimzia® in a wider patient population. In patients with Crohn's disease who require long-term immunosuppressant therapy
, have an increased risk of developing lymphoma compared with the general population, even if they are not treated with TNF-α inhibitors.
In a clinical study, one patient with psoriatic arthritis was diagnosed with lymphoma.
Chronic heart failure
During treatment with Cimzia®, both new cases of CHF and progression of previously existing symptoms of CHF were noted. Most of these cases were mild or moderate in severity and were diagnosed within the first year of treatment with the drug.
Immunogenicity
Rheumatoid arthritis
Total number of patients with rheumatoid arthritis
with antibodies to the drug Cimzia®, which were determined at least once, was 9.6% in placebo-controlled studies of the drug.
In approximately 1/3 of these patients, the antibodies showed neutralizing activity in vitro
. In patients who were simultaneously taking immunosuppressants (methotrexate), the rate of antibody formation was lower than in patients who were not initially receiving them. Antibody formation was associated with lower plasma concentrations of Cimzia® and, in some patients, with lower efficacy.
Crohn's disease
In Crohn's disease, in 8% of patients receiving long-term treatment with Cimzia®, antibodies to the drug were detected, in approximately 6% of them the antibodies were neutralized in vitro
. There is no obvious relationship between the formation of antibodies and the effectiveness of Cimzia®. In patients who were simultaneously taking immunosuppressants, the level of antibody formation was lower than in patients who were not taking them (3% and 11%, respectively).
Psoriatic arthritis
Total number of patients with psoriatic arthritis
in a placebo-controlled study in which antibodies to the drug Cimzia® were detected at least once within 24 weeks was 11.7%. Antibody formation was associated with lower plasma drug concentrations. The number of patients with antibodies to Cimzia® was not sufficient to provide a definitive assessment of the relationship between antibody titer and drug efficacy.
Axial spondyloarthritis
In a placebo-controlled study in axial spondyloarthritis
the total number of patients in whom antibodies to Cimzia® were detected at least once within 24 weeks was 4.4%. Antibody formation was associated with lower plasma drug concentrations. The number of patients with antibodies to the drug was not sufficient to provide a definitive assessment of the relationship between antibody titer and drug efficacy.
Antibody formation
In clinical studies in 4% of patients with Crohn's disease
, receiving the drug Cimzia®, and in 2% of patients receiving placebo, the formation of antinuclear antibodies (ANA) was noted. In studies of TNF-α inhibitor drugs, including Cimzia®, the formation of antinuclear antibodies (ANA) has also been observed in selected patients with rheumatoid arthritis. In clinical studies of Cimzia® for rheumatoid arthritis and Crohn's disease, some patients experienced the development of symptoms similar to lupus-like syndrome. The effect of long-term treatment with Cimzia® on the development of the autoimmune process has not been established.
Hypersensitivity reactions
The following symptoms, which are similar to hypersensitivity reactions, have been observed in rare cases after administration of Cimzia® to patients: angioedema, allergic dermatitis, itchy rash, shortness of breath, hot flashes, decreased blood pressure, injection site reactions, feeling of malaise, hyperthermia , rash, serum sickness and fainting.
Reactions at the injection site
In some patients, during treatment with Cimzia®, the following reactions were observed at the injection site: erythema, itching, subcutaneous hematoma, pain, swelling or bruising.
There were no cases of drug withdrawal due to the development of local reactions.
Increased activity of creatine phosphokinase (CPK)
The incidence of increased CPK activity in patients with axial spondyloarthritis (ASA) was generally higher than in the population of patients with rheumatoid arthritis (RA). This frequency was higher in patients with ASA and RA receiving placebo, 2.8% and 0.4%, respectively, and during treatment with Cimzia®, 4.7% and 0.8%, respectively.
The increase in CPK activity in patients with ASA was in most cases transient, clinically insignificant, and was not the reason for discontinuation of participation in the study in any patient.
Simziya
The most serious adverse reactions were infections, cancer and heart failure. In controlled studies, the most commonly reported infections were upper respiratory tract infections (18%), skin rashes (9%), and urinary tract infections (8%).
In patients with rheumatoid arthritis in controlled studies during treatment with Cimzia®, adverse reactions were noted in 10.7% of cases, and in the placebo group - in 6.6%.
The most frequently observed adverse reactions were those related to the area of “infections and infestations” - in 15.5% of patients receiving the drug Cimzia®, and in 7.6% of patients in the placebo group; and also - “general disorders and complications associated with the method of drug administration” in 10.0% of patients receiving Cimzia® and 9.7% receiving placebo.
Treatment was stopped due to the development of adverse reactions in 5% of patients treated with Cimzia* and in 2.5% of patients who did not receive the drug (placebo group). The most common reasons for stopping treatment with Cimzia® were: tuberculosis (0.5%), hyperthermia, urticaria, pneumonia and skin rashes (0.3%).
In Crohn's disease in controlled studies, the most common adverse reactions were the following: upper respiratory tract infections (rhinopharyngitis, laryngitis, acute respiratory viral infection (ARVI)) in 20% of patients treated with Cimzia® and in 13% of patients who did not receive the drug ; infections of the urinary system (cystitis, bacteriuria) in 7% of patients receiving Cimzia® and 6% receiving placebo; arthralgia - in 6% of patients receiving Cimzia®, and in 4% - placebo; headache - in 14.8% of patients receiving the drug Cimzia® and in 13.5% - placebo, abdominal pain - in 9.3% of patients receiving the drug Cimzia®, and in 8.8% - placebo.
11.3% of patients treated with Cimzia® and 12.6% who did not receive the drug were excluded from the study due to severe adverse reactions. The most common reactions were: diarrhea (0.4% and 0%, respectively), abdominal pain (0.4% and 0.2%) and nausea (0.4% and 0.2%).
Adverse reactions are grouped by frequency of occurrence: very often (≥1/10); often (≥1/100, <1/10); uncommon (≥1/1000, <1/100); rare (≥1/10,000, <1/1000); very rare (<1/10,000), including isolated reports.
Infections and infestations:
often - bacterial infections (abscess), viral infections (caused by herpes virus, papillomavirus, influenza); uncommon - sepsis (including multiple organ failure and septic shock), tuberculosis, fungal infections (including opportunistic).
Benign tumors, malignant neoplasms and other formations (including cysts and polyps):
uncommon - solid tumors, non-melanoma skin cancer, precancerous conditions (leukoplakia of the oral mucosa, melanocytic nevus), benign tumors and cysts (including papillomas); rarely - lymphoma, gastrointestinal tumors, melanoma.
From the hematopoietic and lymphatic systems:
often - eosinophilia, eosinopenia, leukopenia (lymphopenia and neutropenia); uncommon - anemia, thrombocytopenia, lymphadenopathy, thrombocytosis; rarely - pancytopenia, splenomegaly, erythrocytosis, morphologically altered leukocytes.
From the immune system:
uncommon - vasculitis, SLE (systemic lupus erythematosus), hypersensitivity to the drug, psoriasis and related diseases, allergic disorders, positive reaction to autoantibodies; rarely - angioedema, sarcoidosis, serum sickness, panniculitis (including erythema nodosum).
From the endocrine system:
rarely - dysfunction of the thyroid gland.
Metabolic disorders:
uncommon - electrolyte disturbances, dyslipidemia, loss of appetite, changes in body weight; rarely - changes in plasma glucose concentration, hypoalbuminemia, hypoproteinemia, hemosiderosis.
Mental disorders:
uncommon - anxiety (including restlessness), mood changes (and associated symptoms); rarely - suicide attempts, delirium, decreased mental activity, aggression.
From the nervous system:
often - headache (including migraine), sensitivity disorders; uncommon - peripheral neuropathy, dizziness, tremor, optic neuritis; rarely - acoustic neuritis, convulsive attack, extrapyramidal disorders, trigeminal neuralgia, impaired coordination of movements and sense of balance, dysphonia, mask-like facial expression, sleep disturbance; frequency unknown - multiple sclerosis.
From the side of the organ of vision:
uncommon - impaired visual perception (including decreased visual acuity), uveitis and phlebaritis, dacryoadenitis and dacryocystitis, impaired lacrimation.
On the part of the hearing organ:
infrequently - vertigo; rarely - hearing loss, tinnitus.
From the cardiovascular system:
often - increased blood pressure; uncommon - cardiomyopathy, heart failure, coronary heart disease, arrhythmias (including atrial fibrillation), rapid heartbeat, hemorrhages, bleeding, hypercoagulation (PE, thrombophlebitis), fainting, decreased blood pressure, edema (face, extremities), ecchymosis (hematomas, petechiae) ); rarely - pericarditis, atrioventricular block, stroke, atherosclerosis, Raynaud's syndrome, livedo reticularis, telangiectasia.
From the respiratory system:
uncommon - pleural effusion (and associated symptoms), bronchial asthma and its manifestations, shortness of breath, congestive and inflammatory changes in the lungs, cough; rarely - interstitial changes in the lungs, pneumonitis, ulceration of the nasal mucosa.
From the digestive system:
often - nausea, vomiting; uncommon - ascites, symptoms of Crohn's disease (stenosis), ulcerative lesions and perforation (of various parts of the gastrointestinal tract), inflammation of the gastrointestinal mucosa, dyspepsia, stomatitis, symptoms of peritoneal irritation, dry mucous membrane of the mouth and throat; rarely - intestinal obstruction, dysphagia, anal fissures, increased intestinal motility.
From the hepatobiliary system:
often - hepatitis, increased activity of liver enzymes; infrequently - liver cirrhosis, cholestasis, increased concentration of bilirubin in the blood plasma; rarely - cholelithiasis.
For the skin and subcutaneous fat:
often - rash; uncommon - alopecia, dermatitis, eczema, dysfunction of the sweat glands, ulcerative dermatitis, increased photosensitivity, acne, areas of depigmentation, dry skin, lesions of the nail plate and nail bed; rarely - acute febrile neutrophilic dermatosis, exfoliation and desquamation of the skin, bullous dermatitis, pityriasis rosea, stretch marks, disorder of the hair structure.
From the musculoskeletal system:
uncommon - arthritis, muscle dysfunction; rarely - dysfunction of the tendons.
From the urinary system:
uncommon - renal dysfunction, hematuria, nephrolithiasis, urethritis, cystitis; rarely - nephropathy, nephritis.
From the reproductive system:
uncommon - menstrual irregularities, uterine bleeding, amenorrhea, breast dysfunction, azoospermia; rarely - premature birth, vaginal discharge, sexual dysfunction, balanitis. Others: often - hyperthermia, pain (unspecified localization), asthenia, itching (unspecified localization), skin reactions at the injection site; uncommon - formation of fistulas (without specifying the location), chills, flu-like syndrome, impaired temperature sensitivity, increased sweating at night, hot flashes; skin damage, slow wound healing.
From the laboratory parameters:
uncommon - increased activity of creatinine phosphokinase (CPK), alkaline phosphatase, total bilirubin, increased blood clotting time, changes in general urinalysis; rarely - increased uric acid in the blood.
Infections
In controlled studies in patients with rheumatoid arthritis, new cases of infectious diseases were observed with a frequency of 0.91 patients per year in those treated with Cimzia® and in those not receiving the drug - with a frequency of 0.72 patients per year. Infections included upper respiratory tract diseases, viral herpetic diseases, urinary tract and lower respiratory tract infections.
In controlled studies, there were more cases of serious infectious diseases in the group treated with Cimzia® (0.06 patients per year) than in those not treated with the drug (0.02 patients per year). Serious infectious diseases included: tuberculosis, pneumonia, inflammation of the subcutaneous tissue, pyelonephritis. There is no increase in the risk of infections with increasing duration of use of the drug Cimzia®.
The incidence of infections in controlled studies in patients with Crohn's disease was 38.0% in those treated with Cimzia® and 30.0% in patients not treated with the drug. Infectious diseases of the respiratory tract were mainly observed (20.0% in patients treated with Cimzia® and 13.0% with placebo). The incidence of clinically significant serious infections in controlled studies was 3.0% among those treated with Cimzia® and 1.0% with placebo. Serious infections included both bacterial and viral diseases, pneumonia, and pyelonephritis.
Tuberculosis
The use of drugs from the group of TNFα inhibitors may be accompanied by the development of activity of the tuberculosis process; when treated with Cimzia®, there are also reports of severe and fatal cases of tuberculosis. In completed and ongoing clinical studies for all known indications among 5118 patients treated with Cimzia®, the incidence of tuberculosis was approximately 0.61 per 100 patients per year. The greatest number of cases was observed in countries where tuberculosis is endemic. Reports include cases of pulmonary and disseminated tuberculosis. In isolated cases - opportunistic infections. There have been cases of death in patients with tuberculosis and opportunistic infections.
Malignant and lymphoproliferative diseases
In controlled studies of TNF-α inhibitors, there was a trend toward an increased incidence of malignancy and lymphoma compared with patients not receiving TNF-α inhibitors.
In patients with rheumatoid arthritis
out of 2367 patients who received the drug Cimzia®, lymphoma was diagnosed in 3 patients, which is approximately 2 times more often than expected on average in the population. Patients with rheumatoid arthritis, especially when the disease is active, have an increased risk of developing lymphoma.
Of 2657 patients with Crohn's disease
, who received the drug Cimzia®, 1 case of lymphoma was registered, and 1 case of lymphoma was observed in patients who did not receive the drug Cimzia® (from the control group, which included 1319 patients).
The incidence of malignancy and lymphoma in clinical trials of Cimzia® should not be compared with the results of studies of TNF-α inhibitors, and the expected prevalence of these diseases also cannot be predicted when used in clinical practice. In patients with Crohn's disease undergoing long-term therapy with immunosuppressants
, have an increased risk of developing lymphoma compared with the general population, even if they are not treated with TNF-α inhibitors.
Heart failure
During treatment with Cimzia®, cases of onset and progression of chronic heart failure have been observed. They were moderate in nature, diagnosis was carried out during the first year of treatment with Cimzia®.
The immune system
Total number of patients with rheumatoid arthritis
with antibodies to the drug Cimzia®, which were determined at least once, was 7.7% in phase III studies of the drug.
About 1/3 of patients (2.6% of the general population) had antibodies with neutralizing activity in vitro
. In patients who were treated with immunosuppressants (methotrexate), the rate of antibody formation was lower than in patients who did not receive them. Antibody formation was associated with lower plasma concentrations of Cimzia® and, in some patients, with lower efficacy.
For Crohn's disease
in those treated with Cimzia®, the total number of patients with a positive reaction to antibodies to the drug during long-term therapy was 8%, and about 6% were neutralized
in vitro
. There is no obvious relationship between the formation of antibodies and the effectiveness of the drug Cimzia® when used in accordance with the dosage regimen. In patients with concomitant use of immunosuppressants, the level of antibody formation was lower (3% and 11%, respectively).
Autoantibody formation
For Crohn's disease
in clinical studies, the formation of autoantibodies was observed in 4% of patients receiving Cimzia® and 2% of patients who did not receive it. In studies of TNF-α inhibitor drugs, including the use of the drug Cimzia®, the appearance of autoantibodies was noted in some patients with rheumatoid arthritis. In studies of both rheumatoid arthritis and Crohn's disease, cases of “lupus-like” syndrome have been reported infrequently. The effect of long-term treatment with Cimzia® on the development of the autoimmune process has not been established.
Hypersensitivity reactions
The following hypersensitivity reactions may develop: angioedema, allergic dermatitis, itchy rash, shortness of breath, hot flashes, decreased blood pressure, skin reactions at the injection site, a feeling of malaise, pyrexia, rash, serum sickness and fainting.
Reactions at the injection site
The following symptoms were observed: erythema, itching, subcutaneous hematoma, pain. There were no cases of drug withdrawal due to the development of local reactions.