Compound
Active ingredients: ternidazole - 200 mg, neomycin sulfate - 100 mg (65,000 IU), nystatin - 100,000 IU, prednisolone sodium metasulfobenzoate - 3 mg.
In addition to the active ingredients, the Terzhinan vaginal tablet includes: wheat starch (amylum tritici), colloidal silicon dioxide (silicii dioxydum colloidale), sodium starch (natrii amylum), magnesium stearate (magnesium stearate), lactose (lactose).
Features of use
Terzhinan in the treatment of vaginitis is prescribed on average for up to 10 days. In complicated cases of vaginal mycoses, therapy can be extended to 20 days.
If the drug is used as a prophylaxis, its use is limited to 6 days. When using Terzhinan suppositories, the following recommendations should be followed:
- Tablets are inserted into the vagina once a day. It is better to carry out the procedure in the evening before going to bed; if candles are placed during the day, then after administration you should be in a horizontal position for at least 10 minutes.
- Before inserting the candle, you must wash your hands thoroughly with soap.
- It is recommended to lightly moisten the tablet in boiled water before placing it, this will speed up the absorption of the active ingredients.
- Menstruation is not a contraindication to vaginal administration of Terzhinan. However, it is better to plan the course of treatment on those days when there are no critical days.
Terzhinan vaginal tablets lead to the appearance of yellowish or white foamy discharge, which is considered normal.
pharmachologic effect
Terzhinan is a drug from the group of combined antimicrobial, antifungal and antiseptic drugs used in gynecological practice.
The physiological effect and pharmacological properties of the drug are determined by the activity of the active components included in its composition. During treatment with Terzhinan, pronounced:
- trichomonacid effect;
- antibacterial effect;
- antifungal effect;
- anti-inflammatory effect.
Pharmacodynamics and pharmacokinetics
ternidazole, which is part of Terzhinan, is aimed at the death of Trichomonas. In addition, it provokes the death of anaerobic microorganisms and, in particular, is active against facultative anaerobes of the genus Gardnerella.
Neomycin is an antibiotic from the aminoglycoside group. The mechanism of its action is associated with the ability to irreversibly disrupt protein synthesis in the cells of pathogenic microorganisms at the ribosomal level.
By suppressing protein synthesis, neomycin causes disturbances in the transcription of the genetic code and provokes the death of microbial cells. It has been experimentally proven that aerobic bacteria, as a rule, are sensitive to it: corynebacteria (C. amycolatum), Listeria (Listeria), as well as methicillin -sensitive Staphylococcus aureus (MSSA).
In addition, it was found that gram-negative bacteria are also sensitive to neomycin, including aeruginosa , which is usually resistant to the action of this antibiotic.
Nystatin is an antimycotic agent from the group of polyene antibiotics. to ergosterol contained in the membranes of fungal cells , it causes their damage and thereby provokes the death of fungi. Nystatin only affects eukaryotes. Fungi belonging to the genus Candida are sensitive to it, including strains of Candida albicans and Candida glabrata.
Prednisolone is a glucocorticoid drug. When applied topically, its therapeutic activity is determined by its anti-inflammatory, antiallergic and antiexudative effects. The latter is due to the vasoconstrictor effect of prednisolone.
The excipients included in the vaginal tablets ensure the integrity of the vaginal epithelial tissue in various infectious and inflammatory diseases, and also maintain the pH balance within the physiological norm.
The pharmacokinetic characteristics of Terzhinan have not been studied, which is due to the low systemic absorption of this drug.
Introduction
Disturbances of the vaginal microecosystem are the most important medical problem faced by obstetricians-gynecologists and most patients. This is due to the high frequency of such diseases, diagnostic difficulties and the absence of pathognomonic clinical manifestations. At the same time, the species composition and range of pathogens of genital infections are extremely wide. The vast majority of cases of inflammatory diseases of the female genital organs (60–70%) are caused by polymicrobial flora [1, 2]. The frequency of mixed vaginitis is increasing. Mixed infections are often characterized by a complicated course. Their complications include severe inflammatory diseases of the uterine appendages, leading to the development of severe adhesions and tubo-peritoneal infertility, postpartum and postoperative complications in obstetrics and gynecology [2, 3]. A separate problem is infectious inflammatory diseases of the lower genital tract. They are detected in 60–85% of patients in gynecological hospitals. Currently, numerous clinical, microbiological and pathogenetic studies are being conducted on the problem of vaginitis and vulvovaginitis, new drugs and treatment methods are being proposed, but the prevalence in women of reproductive age still remains high. More than 10% of visits to a gynecologist are related to vaginitis [4]. About 90% of cases of vaginitis are caused by nonspecific bacterial flora, Candida spp. and Trichomonas spp. [1, 3, 5]. The causative agents of nonspecific vaginitis (NV) are represented by a wide range of opportunistic microorganisms, including, in particular, Escherichia spp., Enterococcus spp., Corynebacterium spp., Streptococcus spp., Staphylococcus spp. etc., as well as various combinations thereof. Candida spp. (opportunistic, sporeless dimorphic fungi, which are facultative anaerobes) also often cause vulvovaginitis, often in combination with other representatives of opportunistic flora [5, 6]. The difficulty of diagnosing vaginitis is due to the nonspecificity of complaints and the low level of sanitary and hygienic education of the population, associated with low attendance (often a visit to the doctor occurs only in the case of severe symptoms or the duration of the process). At the same time, there is evidence of a correlation between a history of NV and the number of complications after surgery on the pelvic organs. Separately, it should be noted that the presence of genital infections, including vaginitis, during pregnancy increases the risk of premature birth up to 7.3 times and often becomes the cause of endometritis and other inflammatory infectious complications after cesarean section [7], and also almost doubles the risk spontaneous miscarriages [8]. The choice of drug for the treatment of vaginitis is individual and determined by the clinical course of the disease, the results of microbiological examination (bacterioscopy and culture), polymerase chain reaction (PCR), immunological research methods (enzyme-linked immunosorbent assay (ELISA), etc.), as well as the characteristics of the drug’s action, indications and contraindications to its use. The basis of NV therapy is a two-step treatment approach. The first stage is the eradication of HB-associated microorganisms from the vagina. The second is the restoration of a sufficient number of lactobacilli through the use of probiotics, optionally: local prebiotics, physiotherapy, etc. Previously, at the first stage, as a rule, monotherapy was used: systemic (metronidazole, etc. per os) and topical (clindamycin, chlorhexidine, metronidazole, etc. locally). Currently, preference is given to combination drugs for intravaginal use. This is due to both the complex effect of the active substances included in the drugs, affecting different parts of the etiology and pathogenesis of NV, and a smaller number of adverse drug reactions compared to systemic therapy. Taking into account the high prevalence of NV, especially in the population of women of fertile age, as well as the risks of the impact of these syndromes on the course of pregnancy, the problem is of great medical and social significance [1]. It seems necessary to study the possibilities of using new combined domestically produced topical drugs for the treatment of NV, which would be equal to or superior to their analogues in terms of effectiveness, safety, ease of use and pharmacoeconomic indicators. This article presents the results of a study of the use of the drug "TARGIFORT®, vaginal suppositories" (JSC Avexima, Russia) and the drug "TERZHINAN®, vaginal tablets" (Bouchard-Recordati Laboratories, France) in the treatment of vaginitis of various etiologies. The purpose of this study was to study the effectiveness and safety of the drug TARZHIFORT® in two parallel groups.
Indications for use of Terzhinan
What does Terzhinan treat and when is it advisable to prescribe it?
Indications for the use of vaginal tablets are infectious diseases of the female external genitalia accompanied by inflammatory processes, caused by the entry and active activity of pathogenic microorganisms sensitive to Terzhinan into the vagina.
So, vaginal pills, what are they for? The medicine is prescribed to women who have been diagnosed with:
- vaginitis , provoked by banal pyogenic microflora;
- chronic recurrent colpitis (nonspecific vaginitis);
- vaginal dysbiosis;
- trichomonas vaginitis;
- vaginitis caused by the activity of fungi Candida albicans;
- vaginitis of mixed origin.
Terzhinan is also often prescribed as a prophylactic agent to prevent the development of vaginitis in women who are undergoing minor and major surgical interventions in the pelvic area.
In particular, the medicine is used before childbirth, the procedure of surgical abortion , diathermocoagulation (it is advisable to administer tablets both before and after the procedure), contrast X-ray examination of the uterine cavity and the patency of the fallopian tubes ( metrosalpingography ), before the installation of intrauterine contraceptives and after this procedure and etc..
Terzhinan is also used as a means of preventing complications of antibacterial therapy.
The use of Terzhinan suppositories for ureaplasmosis
Despite the fact that the active growth of ureaplasmosis is most often associated with malfunctions of the immune system, treatment with immunomodulatory drugs does not always achieve the desired result.
In this situation, they resort to prescribing special antibacterial agents or antibiotics. Very often, for ureaplasma, doctors recommend Terzhinan, which acts on a wide range of pathogenic microorganisms and provides a pronounced anti-inflammatory effect.
A valuable property of the drug is that, while provoking the death of microbes and fungi, it does not disturb the natural microflora of the vagina.
Terzhinan for thrush
Terzhinan is recommended for the treatment of women whose thrush is accompanied by suspected secondary inflammation and/or infection with secondary microflora.
In addition, the use of Terzhinan is resorted to in cases where the symptoms are so pronounced that they should be stopped as quickly as possible.
In some cases, the drug is indicated as a substitute for complex therapy if previous treatment with other antifungal agents was ineffective.
Reviews of suppositories for thrush left by patients and practicing gynecologists suggest that Terzhinan successfully cures a fungal infection without causing the development of unwanted side reactions.
For many years, inflammatory processes in the uterus and its appendages occupy one of the first places in the structure of gynecological diseases. The presence of persistent pain syndrome, menstrual dysfunction, and infertility is a consequence of chronic inflammatory diseases of the uterus and its appendages and determines the relevance of this problem [2].
From the perspective of modern pathophysiology, the development of an inflammatory disease, the features of its course and the outcome of the infectious process are determined by three components: a microorganism, a macroorganism and environmental conditions [2, 3]. One of the reasons for failures in the treatment of patients with inflammatory diseases of the genital organs is the peculiarities of the relationship between a macroorganism with altered reactivity (the most important component of which is immune homeostasis) and a microorganism that has acquired new biological properties in new environmental conditions [5].
The trigger mechanism in the development of pelvic inflammatory diseases (PID) is the impact of microbial factors. Currently, the structure of causative agents of inflammatory diseases of the pelvic organs is dominated by polymicrobial flora, including both pathogenic and opportunistic microorganisms [4, 5]. Pathogenic microorganisms, the isolation of which is clearly interpreted as identifying the etiological agent, include Treponema pallidum, Neisseria gonorrhoeae, Haemophilus ducreyi, Chlamydia trachomatis, Trichomonas vaginalis
[5].
Currently, most authors note the increasing role of opportunistic pathogens, which are present in small quantities in the human body without causing disease, and only under certain conditions can become truly pathogenic [6]. Such potentially pathogenic pathogens of nonspecific PID include aerobic gram-positive bacteria of the genera: Streptococcus, Staphylococcus, Enterococcus, Corynebacterium
and aerobic gram-negative rods of the
Enterobacteriaceae family: Escherichia coli, Enterobacter
spp.,
Proteus
spp.,
Klebsiella
spp.,
Pseudomonas
spp.
Among anaerobic bacteria, gram-negative non-spore-forming bacteria of the genera Bacteroides, Fusobacterium, Prevotella
and gram-positive bacteria of the genera
Clostridium
spp.,
Peptostreptococcus, Peptococcus
[2].
As for mycoplasmas and ureaplasmas, which are opportunistic pathogens, their role in the development of the inflammatory process has not been fully determined, although most practitioners, despite the dubious etiological role of these microorganisms, recommend the use of antibacterial drugs aimed at eradicating mycoplasmas and ureaplasmas in the case of their detection in the discharge from the cervical canal.
The routes of infection into the internal genital organs are different, but the main mechanism of infection of the internal genital organs is ascending. Less commonly, a lymphogenous route from nearby pelvic organs is possible. The possibility of infection being introduced into the genital organs from distant foci by hematogenous route cannot be ruled out.
However, for the development of a picture of inflammation, in addition to the presence of the causative microorganism, additional conditions are necessary: violation of barrier defense mechanisms (anatomical and physiological features of the structure of the external genitalia, colonization resistance, acidic environment of the vagina, its ability to self-cleanse, the presence of a mucous plug of the cervical canal), violation local and general anti-infective immunity [1, 6].
Thus, the trigger for the development of exacerbation of chronic salpingo-oophoritis is the influence of a microbial factor due to the activation of opportunistic vaginal flora or the entry of an infectious agent from the outside when barrier defense mechanisms and local anti-infective immunity are disrupted.
The main place in the treatment of inflammatory diseases of the pelvic organs belongs to antibacterial agents, selected taking into account microbiological research data. Considering the polyetiological nature of inflammatory diseases of the uterine appendages, as well as the need to start treatment as early as possible, even before laboratory identification of the pathogen, doctors widely use combinations of antibacterial drugs that can eliminate the widest range of possible pathogenic microorganisms, or broad-spectrum drugs that provide a sufficient clinical effect in the form of monotherapy [7, 8].
In addition to the use of antimicrobial chemotherapy, the complex treatment of chronic PID must include drugs that prevent excessive activation of the inflammatory reaction when it is excessive and activate it when it is insufficient, with the correction of hemostasiological, hemodynamic and metabolic disorders [9].
Treatment and subsequent rehabilitation of women should be based on pathogenetic principles, taking into account the mechanisms of infection of the internal genital organs. Long-term persistence of the pathogen in the lower genital tract with an inadequate response of the immune system contributes to the chronicity of the inflammatory process. The development of subsequent exacerbations, as a rule, is associated with a violation of anti-infective defense mechanisms and with the activation of opportunistic flora.
Therefore, along with systemic drugs for the treatment and prevention of PID, the use of local drugs aimed at normalizing the vaginal microbiocenosis is justified.
The predominance of predominantly polymicrobial associations with the dominant role of opportunistic microorganisms and bacteroid anaerobes explains the fact that currently preference is given to combination drugs capable of eliminating the widest range of possible pathogenic microorganisms. One of these drugs is terzhinan, which is a combination drug containing components necessary for the treatment of bacterial (neomycin sulfate), fungal (nystatin), parasitic and mixed (ternidazole) vaginitis and colpitis. Prednisolone, which is part of it, reduces capillary permeability, helps normalize microcirculation in the vaginal mucosa, thereby improving the flow of anti-inflammatory defense components to the site of inflammation, reducing exudation phenomena, and facilitating the penetration of antibacterial drugs into tissues. Thus, the anti-inflammatory effect of prednisolone is realized, clinically manifested by the rapid disappearance of the main manifestations of the inflammatory reaction: pain, hyperemia, itching, burning. The absence of a systemic effect on the body and the need for additional use of antifungal agents to prevent candidiasis, as well as the absence of an inhibitory effect on the vaginal lactoflora, allows the use of terzhinan for the treatment of mixed infections of the lower genital tract.
The purpose of the study was to evaluate the clinical effectiveness of the drug terzhinan in the complex treatment of chronic nonspecific PID: chronic metroendometritis, chronic salpingoophoritis in combination with nonspecific colpitis, endocervicitis, bacterial vaginosis.
Material and research methods
During the work, a clinical and laboratory examination was carried out on 60 women aged 15 to 50 years with exacerbation of chronic nonspecific PID: chronic salpingoophoritis and chronic metroendometritis. In all patients, inflammatory diseases of the upper reproductive tract were combined with inflammatory processes in its lower section (with nonspecific colpitis, endocervicitis, bacterial vaginosis). The examination of patients included a medical history, general clinical laboratory research methods (general blood and urine analysis, biochemical tests), as well as bacteriological (examination of cultures from the cervical canal for flora), bacterioscopic (examination of smears of vaginal contents, urethra, anus) and instrumental (colposcopy , Ultrasound of the pelvic organs) methods.
During the study, all patients were divided into 2 groups: group 1 included 40 women who used the combined drug terzhinan (1 tablet in the vagina at night for 10 days) in the complex treatment of PID for the purpose of vaginal sanitation (1 tablet in the vagina at night for 10 days); The third group consisted of 20 women who used a topical drug containing metronidazole and miconazole nitrate.
Research results and discussion
The average age of the patients was 26.78±0.78 years. When analyzing social and everyday factors, it was revealed that 61% of women were unmarried; by professional affiliation, 34% of women were housewives, 29% were students.
The frequency of concomitant extragenital pathology was 69.00±4.65%. Noteworthy is the high percentage of concomitant diseases of an infectious and inflammatory nature: acute respiratory viral infection (65.00±7.54%) and influenza (20.00±6.32%) in the anamnesis, chronic tonsillitis (30.00±7.24% ), chronic pyelonephritis (22.50±6.60%), chronic bronchitis and pneumonia (22.50±6.60%).
Analysis of gynecological pathology showed that 65.00±4.77% of patients had a history of episodes of chronic salpingoophoritis. Disturbances of the ovarian-menstrual cycle took second place in the structure of gynecological pathology and amounted to 31.00±4.62%, manifested mainly as algodismenorrhea and oligoopsomenorea. These patients often had a history of other diseases of the genital organs of inflammatory origin: metroendometritis (13.00±1.71%), bartholinitis (2.00±1.40%) and endocervicosis (11.00±3.14%).
When studying the characteristics of reproductive function, each woman had 1.42±0.21 pregnancies (38 ended in childbirth, 23 in medical abortion, 25 in spontaneous abortion).
A history of chronic urogenital infection and vaginal dysbiosis was identified in 42 (63.41±5.35%) patients. Urogenital candidiasis was most often diagnosed (17.07±4.15%), which may be due to both a decrease in general immunological resistance and the use of antibacterial drugs during previous exacerbations. Every sixth woman was treated for bacterial vaginosis (15.00±5.64%), which is a recognized risk factor for PID. Chlamydial infection took third place and amounted to 9.76±3.28%, a history of trichomoniasis was detected in 4.88±2.38% of cases.
When analyzing complaints, patients most often noted pelvic pain of varying severity: from periodic pulling to sharp, “cutting” pain. The average temperature was 37±0.04 °C. Pathological discharge from the genital tract occurred in every second patient with inflammatory diseases of the uterus and its appendages and amounted to 74%. In addition, patients noted itching, burning in the vagina (6%), painful urination (5%).
In 20 patients, during a gynecological examination, the inflammatory process in the internal genital organs was combined with pathology of the cervix. Colposcopy revealed signs of severe focal and diffuse cervicitis in all cases.
Ultrasound signs of inflammatory diseases of the uterus and its appendages were enlarged, cystic-changed ovaries (46%), increased in diameter and length of the fallopian tubes with a thickened hyperechoic wall, which were in most cases soldered to the uterus (63%), increased size uterus, the presence of hyperechoic contents with suspension in its cavity (50%), the presence of reactive effusion in the pelvis (17%).
According to the results of a bacterioscopic examination of a vaginal smear, in most cases (87%) the inflammatory type of smear predominated: a large number of leukocytes and coccal microflora.
In 13.00±4.16% of cases, bacterial vaginosis was detected, which is one of the most common infectious diseases of the lower reproductive tract and, according to various authors, accounts for 20 to 60% of cases in women of reproductive age. Bacterial vaginosis is not accompanied by symptoms of severe inflammation and is characterized by a sharp decrease or absence of lactoflora and its replacement by polymicrobial associations of obligate and facultative anaerobic opportunistic microorganisms.
It is noteworthy that in every third woman, nonspecific colpitis and bacterial vaginosis were associated with urogenital candidiasis. According to statistics, over the past 10 years the number of vaginal candidiasis has almost doubled. At a certain stage of life, 75% of women have at least one episode of vaginal candidiasis; in 5% of women, candidiasis constantly recurs. This determines the choice of therapy, including the simultaneous administration of antibacterial and antifungal drugs.
We identified microflora in cultures from the cervical canal in 5.00±7.97% of patients; in the remaining patients there was no growth of microflora under aerobic conditions. The predominant microorganisms were Staphylococcus
spp.
(15.00 ± 5.65%), fungi of the genus Candida
(20.00 ± 6.32%), as well as
Streptococcus
spp.
(5.00±3.45%), Gardnerella vaginalis
(7.50±4.16%),
E. coli
(2.50±2.455), associations (5.00±3.45%).
Complex treatment included antibacterial monotherapy with broad-spectrum drugs (inhibitor-protected aminopenicillins, second-third generation cephalosporins) or a combination of antibacterial agents (amoxicillin/clavulanate + doxycycline; clindamycin + gentamicin, second-third generation cephalosporins - cefuroxime, cefotaxime, ceftriaxone with doxycycline or macroles ladies and metronidazole).
In addition, the components of the complex treatment included non-steroidal anti-inflammatory drugs, immunomodulators, drugs that improve the rheological properties of blood, and desensitizing agents.
In order to reduce the toxic effect of antibacterial drugs and improve treatment results, patients were prescribed multienzyme drugs and probiotics.
During the acute period of the disease, the patients received physiotherapeutic procedures such as magnetic therapy and low-frequency electrotherapy. At the second stage of treatment, the use of ultrasound and low-pulse laser effects, which have a fibrolytic effect, was practiced.
The dominance of polymicrobial associations, including both aerobic, obligate and facultative anaerobic opportunistic microorganisms, and yeast fungi of the genus Candida
, dictates the need to prescribe, along with systemic antibacterial therapy, complex local agents, of which terzhinan is a representative.
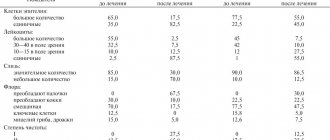
According to a clinical and laboratory study, the effectiveness of terzhinan therapy was 87.7%, which was manifested by normalization of the degree of purity of vaginal contents, subjective and objective improvement, which was characterized by the disappearance or reduction of discharge from the genital tract, and in 12.3% of cases these indicators significantly improved compared with those before treatment (see table).
The dynamics of clinical symptoms when using Terzhinan included the disappearance of vulvar itching on average on the 5th day of treatment, relief of pain in the area of the vaginal vestibule - on the 2nd, normalization of the nature of discharge - on the 6th day. By the end of the course of treatment (on the 10th day), all patients had no complaints. Of the 40 patients with nonspecific colpitis, according to a microbiological study, cure was found in 34. In addition, all patients had an increase in the number of lactobacilli without additional use of eubiotics.
In group 2, the disappearance of these symptoms occurred 1-2 days later, and in some cases the pathological symptoms resumed on the 9-10th day and later (see figure).
Figure 1. Time frame for relief of the main clinical manifestations of inflammatory diseases of the lower reproductive tract during treatment in the examined groups. In 12 out of 20 patients, treatment was found to be ineffective, which required an additional anti-inflammatory course of treatment.
Side effects of terzhinan were observed in 2 patients in the form of unexpressed short-term burning sensations, and only on the 1st-2nd day after application.
Among the patients of group 1, 12 had concomitant pathology of the cervix, in group 2 - 8. According to the results of colposcopy, signs of focal and diffuse cervicitis were revealed in patients of both groups. A cytological study, allowing to assess the structure and cellular level of tissue damage, was carried out after anti-inflammatory treatment.
In the group where terzhinan was used, there was no questionable cytological evidence of the presence of intraepithelial neoplasia; In no case was additional anti-inflammatory treatment required. In group 2, 5 out of 8 patients, due to incomplete relief of the inflammatory process in the cervical tissues, had difficulties with the differential diagnosis of intraepithelial neoplasia and inflammatory changes, which required an additional course of vaginal sanitation.
Thus, a decrease in local immunological resistance of the lower genital tract, characteristic of the chronic course of the inflammatory process, contributes to the disruption of normal colonization resistance of the vagina, serves as a source of ascending infection of the internal genital organs and is the main factor in the development of exacerbation. Antibacterial therapy, which is an integral part in the treatment of exacerbation of infectious processes in the internal genital organs, in turn, is accompanied by the development of dysbiosis of the vaginal flora. Thus, one of the vicious circles in the pathogenesis of exacerbation of PID is closed. Local use in complex treatment of a broad-spectrum antibiotic, a metronidazole component that affects anaerobic flora, and an antifungal drug not only promotes vaginal sanitation, but also prevents the development of bacterial vaginosis. The role of prednisolone as one of the components of terginan is significant, which allows normalizing microcirculation in the vaginal mucosa, promotes the influx of anti-inflammatory defense components, optimizes the delivery of drugs to the site of inflammation, and ensures the maintenance of normal flora in the vagina.
conclusions
The combined local drug terzhinan, along with systemic antibacterial chemotherapy drugs, immunomodulators, drugs aimed at combating hemodynamic and metabolic disorders, as well as degenerative processes in the tissues of the uterus and its appendages, is the drug of choice in the complex treatment of inflammatory diseases of the pelvic organs.
Side effects
Terzhinan quite rarely provokes side effects. Since suppositories are used topically, their constituent components are absorbed into the systemic circulation in very small concentrations.
Therefore, in most reported cases, they provoked exclusively local reactions, which were expressed in the form of allergy symptoms, burning sensation, tingling, itching, pain and irritation at the site of drug administration.
Systemic effects during treatment with the drug occur in isolated cases. A possible reaction to the use of glucocorticosteroids (and, in particular, to prednisolone ) is a slowdown in the healing processes of wounds and cracks, and atrophic processes in the mucous membrane may also occur in some patients.
Terzhinan suppositories, instructions for use (Method and dosage)
Instructions for use of Terzhinan recommend inserting vaginal tablets deep into the vagina, one once a day, every day for ten days.
Before inserting the tablet into the vagina, it should be immersed in water for about 30 seconds (or held in a wet hand for about two minutes). If the tablet is administered during the day rather than in the evening, you should lie down for at least ten minutes after administration.
The optimal time for the procedure is evening. This is due to the fact that in the morning after the administration of Terzhinan, a yellowish discharge may appear, which is normal when undergoing a course of treatment with the drug.
If the goal of treatment is to normalize the imbalance of microflora in the vagina and relieve symptoms of inflammation, then the duration of treatment, depending on the clinical picture and the doctor’s prescription, is from six to ten days.
If the reason for using the drug is thrush , the course of therapy is increased to 20 days. Three days after its completion, it is recommended to undergo a re-examination and take tests, which will either confirm complete recovery or indicate the need for a repeat course.
During pregnancy, the dose and duration of treatment are determined by the attending physician depending on the clinical situation.
Is it possible to use suppositories during menstruation?
Very often, patients who are indicated for treatment with Terzhinan wonder whether these pills can be used during menstruation. In the instructions for the drug, the manufacturer indicates that menstruation is not an indication for stopping treatment.
How to use Terzhinan
The medication is indicated for use in patients over 16 years of age. Terzhinan is not recommended for adolescents due to the imperfection of the internal vaginal microflora.
- Before use, it is recommended to moisten the tablet in warm water.
- Lying on your back, carefully insert the drug deep into the vagina.
- After administering Terzhinan, do not stand up for 10–15 minutes so that the candle does not accidentally fall out. The best time for the procedure is in the evening, before bed.
General treatment regimen: 1 tablet once every day for 6–20 days. For a preventive course, a week of use is enough. For acute conditions and recurrent pathologies, it is advisable to use the product for at least two weeks in a row. In case of menstrual flow, it is not recommended to interrupt treatment. The exception is an increase in tissue sensitivity and the appearance of irritation of the mucous membrane when exposed to the drug on these days.
During the period of using vaginal tablets, it is important to take good care of hygiene. Due to the specific secretions of the dissolved drug, more frequent changes of underwear are required. It is recommended to use gaskets with a sufficient degree of protection.
Sexual rest during therapy is not necessary, but may be recommended by a gynecologist. It is important to remember that nystatin in Terzhinan may reduce the effectiveness of barrier contraception.
After 5–7 days after the end of the course of treatment, a repeat laboratory test should be done to determine the presence of infection.
special instructions
The results of studies of the effectiveness of the components of the drug Terzhinan demonstrated that the concentrations of the active components in this drug for local therapy (but not for oral administration) are higher than the toxic concentrations that determine the development of immunity to the antibacterial component.
Under such conditions, it is assumed that the activity of strains of the infectious agent that are theoretically resistant to the active substance will be suppressed by its high concentrations.
In addition, it is very likely that high concentrations of all active components of Terzhinan can have a synergistic (increasing effect of each other) effect on pathogenic microflora, which, in terms of its spectrum of action, is much wider than that of each individual active component.
It should be remembered that drugs containing nystatin intended for intravaginal use may damage latex contraceptives.
Considering that the active components of Terzhinan can potentially be slightly absorbed into the systemic circulation, it should be remembered that when using systemic glucocorticosteroids in patients diagnosed with osteoporosis , arterial hypertension and heart failure , supervision by specialists in the appropriate field is required.
Specialist supervision is also required for existing or history of peptic ulcers , tuberculosis , glaucoma , hypothyroidism , serious emotional disorders, myopathy provoked by the use of glucocorticosteroids, liver failure , epilepsy , diabetes mellitus , recent myocardial infarction .
Terzhinan is an effective remedy for women. What about for men?
Gynecologists constantly remind us that all infectious and inflammatory diseases for which Terzhinan is indicated must be eliminated from both the woman and the man. To do this, both partners must undergo a course of treatment with antibacterial drugs.
Neglecting this point risks the fact that all the unpleasant symptoms that appear with a particular disease will return. It is also recommended to abstain from sex for the entire period of treatment, but some doctors sometimes still allow partners to have a normal sex life.
The main conditions are the mandatory use of a condom and the complete absence of any side effects from the reproductive system (for both women and men).
For example, some women may experience a strong burning sensation during sexual intercourse (or some time after it), while complaints from men are more often associated with unpleasant sensations and some discomfort.
In any of these cases, the optimal solution is to abstain from sexual activity until the course of treatment is completed. It is important to remember that sexual intercourse must occur only before the next evening vaginal tablet is administered (not after!).
Terzhinan's analogs
Many patients, having received a prescription for the drug from a doctor, try to find a cheaper alternative to Terzhinan.
Currently Terzhinan has no analogues. For women diagnosed with bacterial vaginosis or vaginitis , a number of medications may be prescribed, such as:
- Neotrizol
- Polygynax
- Meratin Combi
Despite the fact that they are similar in action to Terzhinan, the latter is unique in its composition and ability to have a complex effect on inflammatory and infectious processes affecting the mucous membrane of the female external genital organs.
The average price of analogues of Terzhinan candles varies from 400 to 700 rubles.
Which is better: Terzhinan or Polygynax?
The effect exerted by the drug Polygynax is identical to the effect exerted by Terzhinan. However, studies aimed at comparatively assessing the activity of the components of these two drugs in in vitro models showed that Terzhinan, unlike Polygynax, has no effect on MRSA (methicillin-resistant Staphylococcus aureus), streptococci and enterococci. At the same time, it showed great activity against Gardnerella vaginalis (G. vaginalis).
Which is better: Hexicon or Terzhinan? Terzhinan or Penotran?
Both of these drugs have a similar effect to Terzhinan, but differ from the latter in composition.
That is, the active ingredients of each of these drugs may exhibit different activity against the same microorganisms. Consequently, only the attending physician can decide which drug is better and which will be less effective in each specific case.
Terzhinan during pregnancy and lactation
Why are Terzhinan suppositories prescribed to pregnant and lactating women?
The instructions for Terzhinan during pregnancy allow the use of the drug during this period of a woman’s life, but only under the supervision of a doctor managing the pregnancy.
The tablets are contraindicated in the 1st trimester; in the 2nd and 3rd trimester during pregnancy, the drug is usually prescribed for inflammation of the vagina (vaginitis) , which is caused not by one pathogen, but by several (that is, bacteria and fungi). This disease is called combined, and combination medications, which include an antibiotic and an antimycotic agent, are suitable for its treatment.
The low degree of absorption of Terzhinan into the systemic circulation eliminates the possibility of overdose and the possibility of transfer of drug components through the bloodstream to the developing fetus.
Thus, Terzhinan suppositories during pregnancy do not have a negative effect on the body of the unborn child. In addition, it is allowed to take the medicine regardless of taking oral medications, since its active components do not interact with the components of other medications.
The use of Terzhinan during lactation is also allowed. The main condition for prescribing the drug is a correctly diagnosed diagnosis confirming the need for treatment. The drug is prescribed if more gentle means and methods do not help eliminate itching and burning.
However, like any other drug, Terzhinan should not be used by pregnant and lactating women unless absolutely necessary and without first consulting a doctor.
Reviews about Terzhinan
In their reviews of Terzhinan suppositories, almost all women note that the main advantages of this drug are that the latter is very easy to use, accessible (Terzhinan tablets are relatively inexpensive medicines), in the vast majority of cases well tolerated and extremely rarely provokes the development of complications and unwanted side reactions.
If we talk about the effectiveness of the drug for thrush, then reviews of Terzhinan on the forums allow us to conclude that this drug has established itself as an effective and safe remedy that allows you to quickly cure chronic thrush, which becomes more active with any decrease in immunity.
Reviews of Terzhinan during pregnancy and breastfeeding indicate that very often this drug turns out to be an effective remedy (even in cases where other drugs did not help solve the problem).
Negative reviews are mainly associated with hypersensitivity reactions to the components of the drug.
Some women also write that they began to experience spotting after taking one or more Terzhinan tablets. Gynecologists assure that this phenomenon has nothing to do with the use of the drug and to establish the cause of its origin it is necessary to undergo additional examination.
results
Our study is consistent with the data of Russian and foreign researchers, since the average age of the patients in the studied group was 31.5 years.
Risk factors for the development of mixed vulvovaginitis are well known. These include a number of diseases (decompensated diabetes mellitus in the first place), the use of various methods of contraception (spermicides, hormonal contraceptives with a high content of estrogen component), the use of various hygiene products (pads, tampons, antibacterial hygiene products), wearing tight underwear and clothing ; taking broad-spectrum antibacterial drugs. Many authors believe that the activation of endogenous flora due to disruption of the protective role of the normal vaginal microbiota is of key importance in the development of vulvovaginitis; about 90% of cases of vaginitis are caused by nonspecific bacterial flora, Candida spp. and Trichomonas vaginalis [1, 3, 6]. Diagnosis of mixed vulvovaginitis is difficult due to the nonspecificity of complaints and the low level of sanitary and hygienic education of the population, associated with low appeal. The importance of timely diagnosis and treatment is due to the high frequency of relapses, complications and the difficulties of conservative treatment of complications that have arisen (infertility, adhesions) and the difficulties of managing pregnancy against the background of an active infectious process - the risk of preterm birth increases up to 7.3 times [8] and almost twofold the risk of spontaneous miscarriage increases times [10]. The choice of therapy for the treatment of mixed vulvaginal infections is determined by the clinical course of the disease, the results of microbiological examination (bacterioscopy and culture), PCR, immunological research methods (ELISA, etc.), as well as the characteristics of the drug, indications and contraindications for its use. Based on the “Clinical recommendations for the diagnosis and treatment of diseases accompanied by pathological discharge from the female genital tract” (Moscow, 2019), the basis of therapy is a two-stage method of treatment with combined topical drugs for intravaginal use due to a complex effect on different parts of the etiology and pathogenesis with a smaller number of unwanted drug reactions compared to systemic therapy. Taking into account the high prevalence of vulvovaginitis, as well as the risks of impact on women’s health and the course of pregnancy, it seems necessary to study the possibilities of using new combined topical drugs of domestic production for treatment, which in terms of effectiveness, safety, ease of use and pharmacoeconomic indicators are not inferior or superior to foreign analogues. This article presents the results of a study of the use of the drug "TARGIFORT®, vaginal suppositories" (JSC Avexima, Russia) and the drug "TERZHINAN®, vaginal tablets" (Bouchard-Recordati Laboratories, France) in the treatment of vaginitis of various etiologies. The purpose of this study was to study the effectiveness and safety of these drugs in two parallel groups. The results of the study allow us to recommend the Russian-made drug TARZHIFORT® for the treatment of vaginitis of various etiologies for women of fertile age as an effective and safe means of therapy, convenient for independent use. A comparison of the drugs TARZHIFORT® and TERZHINAN® shows that the effectiveness of the domestic drug TARZHIFORT® in a number of very important indicators that directly affect the quality of life of patients is no lower (no pain in 98.3%, burning in 97.8% and itching in 98, 9% in patients of the TARZHIFORT® group and 98.3%, 97.8% and 95.5% in patients of the TERZHINAN® group), and the rate of disappearance of symptoms “pain” and “burning” – 4.3 and 4.8 days – statistically significantly higher than in patients receiving TERZHINAN® (5.6 and 5.8 days). Not a single patient left the study early, which indicates high compliance with the drug and indicates its convenience for patients and good tolerability. When applying the results of the study in clinical practice, it should be taken into account that its data are associated with such limitations as criteria for inclusion of patients, duration of therapy, presence/absence of concomitant diseases and/or therapy with other drugs. Apparently, further studies (observational programs) are required, during which the effectiveness and safety of the use of the study drug for long-term (repeated use) will also be assessed, as well as a number of such important parameters as patient adherence to treatment, the effect of therapy on the quality of life etc. From a medical and social point of view, it is also important to analyze the pharmacoeconomic characteristics of the drug under study and its availability to the patient.
Terzhinan price, where to buy
How much do candles cost in Russia?
The price of Terzhinan No. 10 tablets is about 600 rubles. The price of Terzhinan No. 6 candles is about 500 rubles. You can find out the exact cost of 6 or 10 tablets either on the website of a specific pharmacy chain or by calling the desired pharmacy.
Terzhinan price in Ukraine
The average price of Terzhinan No. 10 candles in Ukraine is 200 UAH. You can buy tablets No. 6 for an average of 150 UAH.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Terzhinan tablets vaginal.
6 pcs.Sofartex RUR 538 order - Terzhinan tablets vaginal. 10 pcs.Sofartex
RUR 736 order
Pharmacy Dialogue
- Terzhinan vaginal tablets No. 10Lab.Bouchara-Recordati
RUR 733 order
- Terzhinan (tab. vag. No. 6)Lab.Bouchara-Recordati
RUR 533 order
show more
Pharmacy24
- Terzhinan N10 tablets Sofartex, France
194 UAH. order - Terzhinan N6 tablets Sofartex, France
147 UAH order
PaniPharmacy
- Terzhinan tablets Terzhinan vaginal tablets No. 6 France, Sofartex
159 UAH order
- Terzhinan tablets Terzhinan vaginal tablets No. 10 France, Sofartex
224 UAH order
show more
Dosage form and composition of the drug Terzhinan
Terzhinan is a combined broad-spectrum antimicrobial drug. It is produced in the form of tablets for local and intravaginal use. These are suppositories similar to suppositories, but have a flatter shape and differ in structure. They do not contain wax.
The packaging of the drug contains 6 or 10 yellowish tablets, packaged in plastic or metallized blisters with individual cells. One dose of the medicine contains 4 active ingredients:
- 200 mg. tenidazole: an antibiotic effective against anaerobic bacteria;
- 100 mg. neomycin: an aminoglycoside that destroys proteins of aerobic microbes;
- 100,000 IU nystatin: antifungal agent;
- 4.7 mg. prednisolone derivative: glucocorticoid hormone with anti-inflammatory effect.
Auxiliary compounds of the drug: starch, lactose, silicon dioxide, magnesium stearate and others.