Dosage form and composition of the drug Terzhinan
Terzhinan is a combined broad-spectrum antimicrobial drug. It is produced in the form of tablets for local and intravaginal use. These are suppositories similar to suppositories, but have a flatter shape and differ in structure. They do not contain wax.
The packaging of the drug contains 6 or 10 yellowish tablets, packaged in plastic or metallized blisters with individual cells. One dose of the medicine contains 4 active ingredients:
- 200 mg. tenidazole: an antibiotic effective against anaerobic bacteria;
- 100 mg. neomycin: an aminoglycoside that destroys proteins of aerobic microbes;
- 100,000 IU nystatin: antifungal agent;
- 4.7 mg. prednisolone derivative: glucocorticoid hormone with anti-inflammatory effect.
Auxiliary compounds of the drug: starch, lactose, silicon dioxide, magnesium stearate and others.
Reviews about Terzhinan
- Share your review
- Reply to the author
- I agree with the author
- I do not agree with the author
- Complain
- Review page
Hello. Dear women and girls, come to your senses for God's sake. Don’t listen to these gynecologists who don’t shine with special knowledge! There are few good doctors! Never use TERZHINAN. This is a terrible drug. It harms your health and you will later solve numerous problems. I am 29 years old and I had a routine examination with a gynecologist. Everything is fine, the smears are all excellent, but the last smear showed slight inflammation. My gynecologist prescribed TERZHINAN suppositories in the vagina for 6 days at night. I bought. I read that they seem to be good, they have anti-inflammatory, antimicrobial, and antibiotic effects. Made by France. On the 5th tablet I began to have spotting, like during menstruation. My lower abdomen hurt terribly and I was bleeding. imagine my condition. Moreover, my period ended like five days ago. I take Yarina, a hormonal contraceptive, and there are never any failures. I went for a consultation with the head of the gynecological department. She said that TERZHINAN is a strong hormonal drug and can cause terrible side effects, especially when taking another contraceptive. And in general, before prescribing it, the doctor is required to take a smear for bacterial culture of sensitivity to the antibiotic. And they don't do any of this. By the way, the instructions don’t say such terrible side effects. Deceivers. The manufacturer must be judged. Those who do not take hormonal drugs, but have undergone a course of treatment with TERZHINAN, all girls subsequently experience a cycle disorder and they cannot restore it. By the way, if you read on the Internet, Teozhinan caused bleeding and problems for almost everyone. And in Europe, by the way, it is strictly prohibited for pregnant women, and only in Russia is it prescribed to pregnant women from 12 weeks. Come to your senses, Doctor. You are not treating us. Why in Moscow, as prescribed by a doctor, Teozhinan caused uterine bleeding in a 17-week pregnant girl. I don't understand. My pelvic ultrasound is excellent and everything is fine, TERZHINAN is a bad drug! As a woman and as a mother, I ask you to approach the use of this drug very competently and carefully, do not create problems for yourself, dear women. Maybe this is, of course, a reaction of my body, but there are a lot of bad reviews about it. This means I’m not the only one, and these numerous negative reviews already create a system that characterizes this drug as far from being the most ideal and having many side effects that the manufacturer does not even mention in the instructions. Be especially careful if you are pregnant. I would never have written a review if it weren’t for this current situation. Sadly. I will never use it again. Good health to you and take care of yourself. agree disagree
I would never have written a review if it weren’t for this current situation.
Yellow discharge
Yellow discharge after Terzhinan, which is not accompanied by pain, itching or burning, is normal. The drug turns the natural mucus of the cervical canal yellowish and also makes it more abundant. In addition, the mucous membranes absorb only the components necessary for treatment, and the remaining tablets are gradually eliminated over the course of the day.
If the patient takes Terzhinan and the discharge is white or yellow and is also accompanied by itching, this is the result of the destruction of pathogenic microbes. Itching, burning and pain should not continue for more than three days after administration of the drug. The occurrence of side effects over a long period of time indicates the presence of an allergic reaction to the components of vaginal suppositories and the need to replace the drug.
Yellow discharge.
Reviews of good remedies for thrush
Candidiasis (popularly known as thrush) should not be left to chance, as it can become chronic and sometimes even cause infertility. At the moment, there are many tools that can help cope with the problem. So, what is the best remedy for thrush, reviews from doctors and real girls - below.
Important! Do not self-medicate; your doctor will help you choose the optimal course of treatment that is right for you. A separate article discussed ways to quickly get rid of thrush at home.
In later stages of pregnancy, you should consult your doctor.
The mechanism of action of Terzhinan tablets
The instructions for the drug inform that Terzhinan has a pronounced antimicrobial and antiseptic effect, eliminates fungal infections, inflammatory processes, and helps restore the balance of internal microflora. The combination of active substances in it allows you to successfully treat advanced infectious diseases, including those of a combined nature, caused by several pathogens:
- gram-positive and gram-negative bacteria;
- pathogenic fungi;
- Trichomonas.
Terzhinan helps maintain the integrity of the epithelial covers of the mucous membranes, prevents exudative infiltration, the development of erosive and other lesions during inflammatory reactions, normalizes the pH level, alleviates the symptoms of the acute phase of diseases, helps to quickly get rid of itching, burning, tissue swelling and pathological discharge.
The high concentration of components ensures the rapid destruction of all pathogens sensitive to them before they have time to develop resistance to Terzhinan. It is likely that the active substances in the drug enhance the effectiveness and duration of action of each other.
Antibiotics and prednisolone in the medication are active only in the area of placement. They are not absorbed through the mucous membranes into the systemic circulation. The concentrations of active substances penetrating into the body are negligible.
itching after terzhinan
Referral to a gynecological oncologist.
Active substance
The therapeutic effect of the drug is associated with the content of the components included in its composition, such as:
- Ternidazole is a substance with antibacterial activity. It is most effective against Trichomonas.
- Nystatin is an antifungal component that fights candidiasis.
- Neomycin - this substance belongs to the group of aminoglycoside antibiotics that treat purulent complications of infectious infection.
- Prednisolone is a corticosteroid that stops the development of inflammation.
Prednisolone is a glucocorticoid that quickly reduces local inflammation of the vaginal mucosa, itching, and burning.
Precautionary measures
Although no clinically significant interactions with other drugs have been identified, the following should be considered:
- When used simultaneously, nystatin may weaken the effect of clotrimazole.
- It is not recommended to use spermicides during treatment with Terzhinan, as they can weaken the effect of vaginal tablets.
When reception is possible, watch the video:
When reception is possible, watch the video.
Main purposes for the drug Terzhinan
According to the instructions, vaginal tablets are indicated for use:
- for trichomonas and vaginitis caused by pyogenic pathogens
- acute and chronic colpitis of nonspecific or mixed origin, including recurrent ones;
- vaginal candidiasis;
- vaginal dysbiosis;
- ureaplasmosis.
To prevent the development of infectious inflammation in the uterine cavity and adjacent tissues, Terzhinan is prescribed:
- before childbirth;
- insertion of intrauterine devices;
- surgical interventions;
- carrying out abortions, diagnostic curettages;
- before checking the patency of the fallopian tubes.
Medical experience shows that the drug is much more effective than its analogues in treating complicated cases of diseases and rarely causes disturbances in the internal microflora. Terzhinan is better than other intravaginal medications in relieving the symptoms of recurrent thrush and exacerbations of ureaplasmosis.
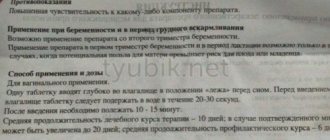
How to use Terzhinan
The medication is indicated for use in patients over 16 years of age. Terzhinan is not recommended for adolescents due to the imperfection of the internal vaginal microflora.
- Before use, it is recommended to moisten the tablet in warm water.
- Lying on your back, carefully insert the drug deep into the vagina.
- After administering Terzhinan, do not stand up for 10–15 minutes so that the candle does not accidentally fall out. The best time for the procedure is in the evening, before bed.
General treatment regimen: 1 tablet once every day for 6–20 days. For a preventive course, a week of use is enough. For acute conditions and recurrent pathologies, it is advisable to use the product for at least two weeks in a row. In case of menstrual flow, it is not recommended to interrupt treatment. The exception is an increase in tissue sensitivity and the appearance of irritation of the mucous membrane when exposed to the drug on these days.
During the period of using vaginal tablets, it is important to take good care of hygiene. Due to the specific secretions of the dissolved drug, more frequent changes of underwear are required. It is recommended to use gaskets with a sufficient degree of protection.
Sexual rest during therapy is not necessary, but may be recommended by a gynecologist. It is important to remember that nystatin in Terzhinan may reduce the effectiveness of barrier contraception.
After 5–7 days after the end of the course of treatment, a repeat laboratory test should be done to determine the presence of infection.
For many years, inflammatory processes in the uterus and its appendages occupy one of the first places in the structure of gynecological diseases. The presence of persistent pain syndrome, menstrual dysfunction, and infertility is a consequence of chronic inflammatory diseases of the uterus and its appendages and determines the relevance of this problem [2].
From the perspective of modern pathophysiology, the development of an inflammatory disease, the features of its course and the outcome of the infectious process are determined by three components: a microorganism, a macroorganism and environmental conditions [2, 3]. One of the reasons for failures in the treatment of patients with inflammatory diseases of the genital organs is the peculiarities of the relationship between a macroorganism with altered reactivity (the most important component of which is immune homeostasis) and a microorganism that has acquired new biological properties in new environmental conditions [5].
The trigger mechanism in the development of pelvic inflammatory diseases (PID) is the impact of microbial factors. Currently, the structure of causative agents of inflammatory diseases of the pelvic organs is dominated by polymicrobial flora, including both pathogenic and opportunistic microorganisms [4, 5]. Pathogenic microorganisms, the isolation of which is clearly interpreted as identifying the etiological agent, include Treponema pallidum, Neisseria gonorrhoeae, Haemophilus ducreyi, Chlamydia trachomatis, Trichomonas vaginalis
[5].
Currently, most authors note the increasing role of opportunistic pathogens, which are present in small quantities in the human body without causing disease, and only under certain conditions can become truly pathogenic [6]. Such potentially pathogenic pathogens of nonspecific PID include aerobic gram-positive bacteria of the genera: Streptococcus, Staphylococcus, Enterococcus, Corynebacterium
and aerobic gram-negative rods of the
Enterobacteriaceae family: Escherichia coli, Enterobacter
spp.,
Proteus
spp.,
Klebsiella
spp.,
Pseudomonas
spp.
Among anaerobic bacteria, gram-negative non-spore-forming bacteria of the genera Bacteroides, Fusobacterium, Prevotella
and gram-positive bacteria of the genera
Clostridium
spp.,
Peptostreptococcus, Peptococcus
[2].
As for mycoplasmas and ureaplasmas, which are opportunistic pathogens, their role in the development of the inflammatory process has not been fully determined, although most practitioners, despite the dubious etiological role of these microorganisms, recommend the use of antibacterial drugs aimed at eradicating mycoplasmas and ureaplasmas in the case of their detection in the discharge from the cervical canal.
The routes of infection into the internal genital organs are different, but the main mechanism of infection of the internal genital organs is ascending. Less commonly, a lymphogenous route from nearby pelvic organs is possible. The possibility of infection being introduced into the genital organs from distant foci by hematogenous route cannot be ruled out.
However, for the development of a picture of inflammation, in addition to the presence of the causative microorganism, additional conditions are necessary: violation of barrier defense mechanisms (anatomical and physiological features of the structure of the external genitalia, colonization resistance, acidic environment of the vagina, its ability to self-cleanse, the presence of a mucous plug of the cervical canal), violation local and general anti-infective immunity [1, 6].
Thus, the trigger for the development of exacerbation of chronic salpingo-oophoritis is the influence of a microbial factor due to the activation of opportunistic vaginal flora or the entry of an infectious agent from the outside when barrier defense mechanisms and local anti-infective immunity are disrupted.
The main place in the treatment of inflammatory diseases of the pelvic organs belongs to antibacterial agents, selected taking into account microbiological research data. Considering the polyetiological nature of inflammatory diseases of the uterine appendages, as well as the need to start treatment as early as possible, even before laboratory identification of the pathogen, doctors widely use combinations of antibacterial drugs that can eliminate the widest range of possible pathogenic microorganisms, or broad-spectrum drugs that provide a sufficient clinical effect in the form of monotherapy [7, 8].
In addition to the use of antimicrobial chemotherapy, the complex treatment of chronic PID must include drugs that prevent excessive activation of the inflammatory reaction when it is excessive and activate it when it is insufficient, with the correction of hemostasiological, hemodynamic and metabolic disorders [9].
Treatment and subsequent rehabilitation of women should be based on pathogenetic principles, taking into account the mechanisms of infection of the internal genital organs. Long-term persistence of the pathogen in the lower genital tract with an inadequate response of the immune system contributes to the chronicity of the inflammatory process. The development of subsequent exacerbations, as a rule, is associated with a violation of anti-infective defense mechanisms and with the activation of opportunistic flora.
Therefore, along with systemic drugs for the treatment and prevention of PID, the use of local drugs aimed at normalizing the vaginal microbiocenosis is justified.
The predominance of predominantly polymicrobial associations with the dominant role of opportunistic microorganisms and bacteroid anaerobes explains the fact that currently preference is given to combination drugs capable of eliminating the widest range of possible pathogenic microorganisms. One of these drugs is terzhinan, which is a combination drug containing components necessary for the treatment of bacterial (neomycin sulfate), fungal (nystatin), parasitic and mixed (ternidazole) vaginitis and colpitis. Prednisolone, which is part of it, reduces capillary permeability, helps normalize microcirculation in the vaginal mucosa, thereby improving the flow of anti-inflammatory defense components to the site of inflammation, reducing exudation phenomena, and facilitating the penetration of antibacterial drugs into tissues. Thus, the anti-inflammatory effect of prednisolone is realized, clinically manifested by the rapid disappearance of the main manifestations of the inflammatory reaction: pain, hyperemia, itching, burning. The absence of a systemic effect on the body and the need for additional use of antifungal agents to prevent candidiasis, as well as the absence of an inhibitory effect on the vaginal lactoflora, allows the use of terzhinan for the treatment of mixed infections of the lower genital tract.
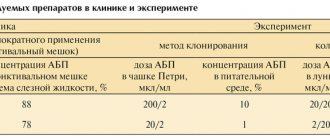
The purpose of the study was to evaluate the clinical effectiveness of the drug terzhinan in the complex treatment of chronic nonspecific PID: chronic metroendometritis, chronic salpingoophoritis in combination with nonspecific colpitis, endocervicitis, bacterial vaginosis.
Material and research methods
During the work, a clinical and laboratory examination was carried out on 60 women aged 15 to 50 years with exacerbation of chronic nonspecific PID: chronic salpingoophoritis and chronic metroendometritis. In all patients, inflammatory diseases of the upper reproductive tract were combined with inflammatory processes in its lower section (with nonspecific colpitis, endocervicitis, bacterial vaginosis). The examination of patients included a medical history, general clinical laboratory research methods (general blood and urine analysis, biochemical tests), as well as bacteriological (examination of cultures from the cervical canal for flora), bacterioscopic (examination of smears of vaginal contents, urethra, anus) and instrumental (colposcopy , Ultrasound of the pelvic organs) methods.
During the study, all patients were divided into 2 groups: group 1 included 40 women who used the combined drug terzhinan (1 tablet in the vagina at night for 10 days) in the complex treatment of PID for the purpose of vaginal sanitation (1 tablet in the vagina at night for 10 days); The third group consisted of 20 women who used a topical drug containing metronidazole and miconazole nitrate.
Research results and discussion
The average age of the patients was 26.78±0.78 years. When analyzing social and everyday factors, it was revealed that 61% of women were unmarried; by professional affiliation, 34% of women were housewives, 29% were students.
The frequency of concomitant extragenital pathology was 69.00±4.65%. Noteworthy is the high percentage of concomitant diseases of an infectious and inflammatory nature: acute respiratory viral infection (65.00±7.54%) and influenza (20.00±6.32%) in the anamnesis, chronic tonsillitis (30.00±7.24% ), chronic pyelonephritis (22.50±6.60%), chronic bronchitis and pneumonia (22.50±6.60%).
Analysis of gynecological pathology showed that 65.00±4.77% of patients had a history of episodes of chronic salpingoophoritis. Disturbances of the ovarian-menstrual cycle took second place in the structure of gynecological pathology and amounted to 31.00±4.62%, manifested mainly as algodismenorrhea and oligoopsomenorea. These patients often had a history of other diseases of the genital organs of inflammatory origin: metroendometritis (13.00±1.71%), bartholinitis (2.00±1.40%) and endocervicosis (11.00±3.14%).
When studying the characteristics of reproductive function, each woman had 1.42±0.21 pregnancies (38 ended in childbirth, 23 in medical abortion, 25 in spontaneous abortion).
A history of chronic urogenital infection and vaginal dysbiosis was identified in 42 (63.41±5.35%) patients. Urogenital candidiasis was most often diagnosed (17.07±4.15%), which may be due to both a decrease in general immunological resistance and the use of antibacterial drugs during previous exacerbations. Every sixth woman was treated for bacterial vaginosis (15.00±5.64%), which is a recognized risk factor for PID. Chlamydial infection took third place and amounted to 9.76±3.28%, a history of trichomoniasis was detected in 4.88±2.38% of cases.
When analyzing complaints, patients most often noted pelvic pain of varying severity: from periodic pulling to sharp, “cutting” pain. The average temperature was 37±0.04 °C. Pathological discharge from the genital tract occurred in every second patient with inflammatory diseases of the uterus and its appendages and amounted to 74%. In addition, patients noted itching, burning in the vagina (6%), painful urination (5%).
In 20 patients, during a gynecological examination, the inflammatory process in the internal genital organs was combined with pathology of the cervix. Colposcopy revealed signs of severe focal and diffuse cervicitis in all cases.
Ultrasound signs of inflammatory diseases of the uterus and its appendages were enlarged, cystic-changed ovaries (46%), increased in diameter and length of the fallopian tubes with a thickened hyperechoic wall, which were in most cases soldered to the uterus (63%), increased size uterus, the presence of hyperechoic contents with suspension in its cavity (50%), the presence of reactive effusion in the pelvis (17%).
According to the results of a bacterioscopic examination of a vaginal smear, in most cases (87%) the inflammatory type of smear predominated: a large number of leukocytes and coccal microflora.
In 13.00±4.16% of cases, bacterial vaginosis was detected, which is one of the most common infectious diseases of the lower reproductive tract and, according to various authors, accounts for 20 to 60% of cases in women of reproductive age. Bacterial vaginosis is not accompanied by symptoms of severe inflammation and is characterized by a sharp decrease or absence of lactoflora and its replacement by polymicrobial associations of obligate and facultative anaerobic opportunistic microorganisms.
It is noteworthy that in every third woman, nonspecific colpitis and bacterial vaginosis were associated with urogenital candidiasis. According to statistics, over the past 10 years the number of vaginal candidiasis has almost doubled. At a certain stage of life, 75% of women have at least one episode of vaginal candidiasis; in 5% of women, candidiasis constantly recurs. This determines the choice of therapy, including the simultaneous administration of antibacterial and antifungal drugs.
We identified microflora in cultures from the cervical canal in 5.00±7.97% of patients; in the remaining patients there was no growth of microflora under aerobic conditions. The predominant microorganisms were Staphylococcus
spp.
(15.00 ± 5.65%), fungi of the genus Candida
(20.00 ± 6.32%), as well as
Streptococcus
spp.
(5.00±3.45%), Gardnerella vaginalis
(7.50±4.16%),
E. coli
(2.50±2.455), associations (5.00±3.45%).
Complex treatment included antibacterial monotherapy with broad-spectrum drugs (inhibitor-protected aminopenicillins, second-third generation cephalosporins) or a combination of antibacterial agents (amoxicillin/clavulanate + doxycycline; clindamycin + gentamicin, second-third generation cephalosporins - cefuroxime, cefotaxime, ceftriaxone with doxycycline or macroles ladies and metronidazole).
In addition, the components of the complex treatment included non-steroidal anti-inflammatory drugs, immunomodulators, drugs that improve the rheological properties of blood, and desensitizing agents.
In order to reduce the toxic effect of antibacterial drugs and improve treatment results, patients were prescribed multienzyme drugs and probiotics.
During the acute period of the disease, the patients received physiotherapeutic procedures such as magnetic therapy and low-frequency electrotherapy. At the second stage of treatment, the use of ultrasound and low-pulse laser effects, which have a fibrolytic effect, was practiced.
The dominance of polymicrobial associations, including both aerobic, obligate and facultative anaerobic opportunistic microorganisms, and yeast fungi of the genus Candida
, dictates the need to prescribe, along with systemic antibacterial therapy, complex local agents, of which terzhinan is a representative.
According to a clinical and laboratory study, the effectiveness of terzhinan therapy was 87.7%, which was manifested by normalization of the degree of purity of vaginal contents, subjective and objective improvement, which was characterized by the disappearance or reduction of discharge from the genital tract, and in 12.3% of cases these indicators significantly improved compared with those before treatment (see table).
The dynamics of clinical symptoms when using Terzhinan included the disappearance of vulvar itching on average on the 5th day of treatment, relief of pain in the area of the vaginal vestibule - on the 2nd, normalization of the nature of discharge - on the 6th day. By the end of the course of treatment (on the 10th day), all patients had no complaints. Of the 40 patients with nonspecific colpitis, according to a microbiological study, cure was found in 34. In addition, all patients had an increase in the number of lactobacilli without additional use of eubiotics.
In group 2, the disappearance of these symptoms occurred 1-2 days later, and in some cases the pathological symptoms resumed on the 9-10th day and later (see figure).
Figure 1. Time frame for relief of the main clinical manifestations of inflammatory diseases of the lower reproductive tract during treatment in the examined groups. In 12 out of 20 patients, treatment was found to be ineffective, which required an additional anti-inflammatory course of treatment.
Side effects of terzhinan were observed in 2 patients in the form of unexpressed short-term burning sensations, and only on the 1st-2nd day after application.
Among the patients of group 1, 12 had concomitant pathology of the cervix, in group 2 - 8. According to the results of colposcopy, signs of focal and diffuse cervicitis were revealed in patients of both groups. A cytological study, allowing to assess the structure and cellular level of tissue damage, was carried out after anti-inflammatory treatment.
In the group where terzhinan was used, there was no questionable cytological evidence of the presence of intraepithelial neoplasia; In no case was additional anti-inflammatory treatment required. In group 2, 5 out of 8 patients, due to incomplete relief of the inflammatory process in the cervical tissues, had difficulties with the differential diagnosis of intraepithelial neoplasia and inflammatory changes, which required an additional course of vaginal sanitation.
Thus, a decrease in local immunological resistance of the lower genital tract, characteristic of the chronic course of the inflammatory process, contributes to the disruption of normal colonization resistance of the vagina, serves as a source of ascending infection of the internal genital organs and is the main factor in the development of exacerbation. Antibacterial therapy, which is an integral part in the treatment of exacerbation of infectious processes in the internal genital organs, in turn, is accompanied by the development of dysbiosis of the vaginal flora. Thus, one of the vicious circles in the pathogenesis of exacerbation of PID is closed. Local use in complex treatment of a broad-spectrum antibiotic, a metronidazole component that affects anaerobic flora, and an antifungal drug not only promotes vaginal sanitation, but also prevents the development of bacterial vaginosis. The role of prednisolone as one of the components of terginan is significant, which allows normalizing microcirculation in the vaginal mucosa, promotes the influx of anti-inflammatory defense components, optimizes the delivery of drugs to the site of inflammation, and ensures the maintenance of normal flora in the vagina.
conclusions
The combined local drug terzhinan, along with systemic antibacterial chemotherapy drugs, immunomodulators, drugs aimed at combating hemodynamic and metabolic disorders, as well as degenerative processes in the tissues of the uterus and its appendages, is the drug of choice in the complex treatment of inflammatory diseases of the pelvic organs.
Side effects and contraindications
Terzhinan does not cause exacerbations of existing chronic pathologies. Due to the lack of systemic action, it does not interact with other medications. In rare cases, its use may cause itching and irritation of the mucous membranes. The only contraindication is individual intolerance to one or more components. Its signs:
- severe burning sensation;
- redness of the integument;
- swelling of the mucous membrane or severe pain at the injection site.
In isolated cases, Prednisolone in tablets can provoke erosive lesions of the vaginal walls. In addition, this hormone requires careful use of the drug for hypothyroidism, diabetes, and cardiovascular pathologies.