Preserving the fine structure and physiological function of the cornea is one of the most important tasks of modern clinical ophthalmology. The cornea provides ¾ of the refractive power of the refractive apparatus of the eye [1], and the perfect cytoarchitecture of the cell layers lining the cornea and the keratocytes inhabiting its stroma allows its structure to be more than 99% transparent [2, 3]. Differentiated cells of the outer layer of the corneal epithelium are exfoliated daily (during the natural process of desquamation), giving way to new ones formed from proliferating cells of the basal layer, which, in turn, are derivatives of precursor cells (progenitors) and their more differentiated derivative - transient amplifying cells (SO). The main source of repopulation of the pool of progenitor cells of the corneal epithelium are limbal epithelial stem cells (LESCs), closely associated with Vogt's palisades and the stromal cells inhabiting them [4, 5]. It is the microenvironment of the limbal palisade that maintains stem cells in an undifferentiated, “dormant” state until they are activated by external molecular signals [6]. After activation, the rate of centripetal migration (in the direction from the limbus to the center of the cornea) of LESC-derived cells in humans is about 28 μm per day [7], which allows the restoration of corneal epithelium damaged by external influences in a period of 1 to 4 days. During the migration process, LESCs undergo a number of changes, proliferating first into progenitor cells and then into TAKs. In the case of massive injury to the limbus (damage to more than 70-75% of its circumference), the source of LESC sharply becomes scarce and the main contribution to the regeneration of the epithelial layer of the cornea appears to be made by the pool of TACs that persist in the basal layer of the corneal epithelium [4, 8, 9]. The potential of this residual reserve is low, which leads to disruption of the process of epithelization of the cornea, changes in its transparency and resulting disability.
Thus, the preservation and maintenance of the regenerative potential of the cells of the cornea of the eye both during its iatrogenic injury (photorefractive keratectomy, laser vision correction, shunt operations), and during surgical interventions performed as a result of complicated keratitis or damage to the cornea of a different etiology (penetrating, lamellar or endothelial keratoplasty ), is the primary task of the ophthalmologist and ophthalmic surgeon [10].
Any surgical intervention is accompanied by reactive inflammation [11]. If the inflammation becomes infectious, it can lead to serious consequences, including death of the eye. In modern ophthalmic surgery, one of the main reasons that have a serious adverse effect on the outcome of the operation and the course of the postoperative period is intraocular infection. Therefore, the use of topical antibacterial drugs (TBA) in modern clinical ophthalmology is an integral component of drug therapy, both pathogenetic and preventive. Prescribing ABP for prophylactic purposes in an uncomplicated postoperative period in refractive ophthalmic surgery has become routine practice. At the same time, existing data regarding the effectiveness of this practice are contradictory, which makes the approach to choosing a preventative agent clearly differentiated: taking into account risk factors for the development of infectious complications in the patient and the properties of the agent used [12-13].
Antibiotics of the aminoglycoside and fluoroquinolone groups are most widely used in clinical ophthalmology, as they are highly safe and effective against a wide range of gram-positive and gram-negative bacterial pathogens of ophthalmic infections.
The range of indications for the preventive and therapeutic use of topical antibiotics in ophthalmology is not limited to those listed above, which significantly expands the range of patients receiving these drugs and raises the issue of choice, which should be based not only on the spectrum of activity of the antibiotic, but also on the safety profile of its use.
In ophthalmology, the issue of drug safety requires special attention, since local use of drugs in the conjunctival cavity will certainly affect the epithelium of the conjunctiva and cornea, affecting the rate of tissue repair [15].
The cytotoxicity of ABP is a widely known fact based on both preclinical and clinical data [16–18]. Clinically, this property can manifest itself in a slowdown in the rate of epithelization of the corneal defect [19], corneal edema [20], as well as in the formation of precipitates in its stroma, which has been repeatedly observed in the treatment of keratitis and infected corneal ulcers [21-26]. It should be noted that cytotoxicity, of course, is dose-dependent in nature [27] and is often product-specific, and most publications describing negative experience with the use of antibacterial drugs refer to representatives of the fluoroquinolone group of antibiotics of the first and second generations - ofloxacin and ciprofloxacin [28, 29] . As clinical experience with antibiotics accumulates and new technologies emerge to both search for new candidate molecules and test them, next generations of antibiotics are emerging with improved safety and increased effectiveness. Since the advent of fourth-generation fluoroquinolones, no systematic data on the clinical manifestations of their cytotoxicity have been published, which indirectly indicates an improved safety profile [30, 31], however, there are still isolated clinical cases describing such serious side effects as corneal edema [ 32]. However, the focus of concern has shifted to the safety of delivery vehicles for new molecules, which can also cause serious side effects, as was demonstrated in the case of the bioadhesive sustained delivery platform DuraSite impregnated with besifloxacin or azithromycin in a study of sutureless closure of postoperative corneal defects [33]. B Regarding aminoglycoside antibiotics, in particular third generation drugs, there are currently no clinical data on cytotoxicity.
Assessing the cytotoxicity of antibiotics is an important aspect. In recent years, publications have appeared in the scientific literature that present data on cytotoxicity assessment obtained in experimental in vitro
using cell cultures. An analysis of scientific publications that provide comparative data on assessing the toxic effects of ophthalmic antibiotics on various cellular structures of the eye has shown that there is currently no consensus on this issue [34].
Studies on cell cultures make it possible to quantitatively assess the cytotoxicity of ABP and are of practical importance in the selection and justification of the use of drugs.
The purpose of this study is to compare the general cytotoxic effect on cell cultures of the third generation aminoglycoside antibiotic, netilmicin, the second generation, tobramycin, and the second generation fluoroquinolone antibiotic, ciprofloxacin.
Material and methods
Cell cultures used
Three types of cells were used as test systems in the study: cells of the permanent transformed cell line CHO-K1 (Chinese hamster ovary tumor cells), normal human skin fibroblasts (FC) and cells of the permanent transformed cell line Clone 1−5C-4 (cells normal human conjunctiva). The choice of these cell cultures is due to the fact that all cells are sensitive to general toxicity, regardless of their origin and specialization in the body. CHO-K1 cells, which have a high cloning efficiency and a stable level of spontaneous mutations, are actively used as a model test system for screening potential mutagenicity and carcinogenicity in mammals (OECD, Test No. 476: 1997, IDT). Normal F.K., which maintain a constant diploid set of chromosomes and characteristic morphology throughout the entire cultivation period, are one of the most promising test systems for biochemical and toxicological studies in vitro
. Normal human conjunctival cells are widely used as a test system in ophthalmological research.
Cells of the permanent transformed cell line CHO-K1, isolated from the ovary of a Chinese hamster, were obtained from the Russian collection of vertebrate cell cultures of the Institute of Cytology of the Russian Academy of Sciences (St. Petersburg). Cells were cultured in F12 nutrient medium (Biolot, Russia) supplemented with 10% fetal bovine serum (FBS) (HyClone, USA) and 1% penicillin-streptomycin (Gibco by Life Technologies, USA).
Normal human FCs were isolated at the Institute of Cytology of the Russian Academy of Sciences (St. Petersburg) from facial skin fragments of adult donors obtained as a result of cosmetic surgeries. Cells from passages 3–5 were used in this work. Cells were cultured in DMEM/F12 nutrient medium (Biolot, Russia) supplemented with 10% FBS (HyClone, USA) and 1% penicillin-streptomycin (Gibco by Life Technologies, USA).
Cells of the permanent transformed cell line Clone 1−5C-4 (normal human conjunctival cells) were obtained from the collection of the Research Institute of Virology named after. DI. Ivanovsky RAMS (Moscow). Cells were cultured in Eagle MEM nutrient medium (Biolot, Russia) supplemented with 10% FBS (HyClone, USA) and 1% penicillin-streptomycin (Gibco by Life Technologies, USA).
All cell types were cultured at 37°C in a CO2 incubator under a 5% CO2 atmosphere.
Methods for assessing the effect of antibiotics on cells
The effect of antibiotics on cell cultures was determined by their effect on the viability of cells cultured in nutrient media with the addition of the studied drugs. Quantitative and qualitative assessment methods were used to determine cell viability. Quantitative assessment - a method of cloning cells and a colorimetric method for assessing their proliferation; qualitative assessment - intravital visual observation under an inverted microscope of the morphological state of cells during cultivation with their photographic recording at the time of observation.
Cell cloning method (cell cloning by dilution method)
The method is based on the ability of cells to form colonies, which are clones, like the offspring of one original cell. Distinct clones are formed by sparse seeding of individual cells. The efficiency of colony formation (colony formation efficiency, or cloning efficiency) is determined by the percentage ratio of the number of colonies (clones) formed after N days of cultivation to the number of seeded cells. The efficiency of colony (clone) formation characterizes the viability of cells under given culture conditions.
The effect of the tested drugs on the efficiency of cloning was tested on cells of the CHO-K1 line, which were seeded on Petri dishes with a diameter of 3 cm in 2 ml of F12 nutrient medium (Biolot, Russia) supplemented with 10% FBS (HyClone, USA). Cultivation was carried out at 37 °C in a CO2 incubator in a gas environment with 5% CO2. The tested drugs were added to the nutrient medium at the time of cell seeding. Cells of the same CHO-K1 line, cultured under standard conditions without the addition of drugs, served as a control. The cultivation period was 5 days. Colonies formed during this time were fixed in a 70% ethanol solution and stained with a 0.1% solution of gentian violet (gentian violet). Cloning efficiency was determined as the percentage of the number of formed colonies consisting of 10 or more cells relative to the number of seeded cells. Differences were considered statistically significant at the significance level p
<0,05.
Colorimetric methods for assessing cell proliferation
Colorimetric methods for assessing cell proliferation are based on their staining with organic dyes followed by their extraction from the cells into a solution. The degree of proliferation is determined by the optical density of the dye. Colorimetric methods allow one to estimate the number of viable cells under given culture conditions. The most commonly used tests are the following dyes: neutral red, 3-(4,5-dimethylthiazolin-2-yl)-2,5-diphenyltetrazolium bromide (MTT test), sulforhodamine B (SRB test), gentian violet. The simplest and most accessible methods are the determination of total protein content as an indicator of cell mass growth (SRB test and gentian violet test) [35].
Colorimetric method using gentian violet
The degree of proliferation is determined by the optical density of the gentian violet dye bound to cellular proteins and extracted from the cells after N days of cultivation. The effect of the tested drugs on proliferation was determined on cells of the CHO-K1 line, normal human FC and cells of the permanent transformed cell line Clone 1−5C-4. Cells were seeded into 96-well plates at a rate of 500 cells per well in 200 μl of the appropriate nutrient medium supplemented with 10% FBS (HyClone, USA). For cells of the CHO-K1 line we used F12 medium (Biolot, Russia), for FC - DMEM/F12 (Biolot, Russia), for cells of the Clone 1−5C-4 line - Igla MEM (Biolot, Russia) . The tested ABPs were added to the nutrient media at the time of cell seeding. Cell lines CHO-K1, Clone 1−5C-4 and FK, cultured under standard conditions: at 37 °C in a CO2 incubator in an atmosphere of 5% CO2, served as a control. Cultivation period: 5 days. On the 5th day of cultivation, the cells were fixed in a 70% ethanol solution and stained with a 0.1% gentian violet solution. After this, the dye was extracted from the cells by adding 100 μl of 7% acetic acid to the wells. The number of cells grown during cultivation was determined by photocolorimetric analysis using a Fluorofot analyzer (Charity, Russia) based on the optical density of the dye (Gentian violet) associated with cellular proteins. Measurements were carried out at a wavelength of 570 nm. The obtained data were processed using the MS Excel computer program. Differences were considered statistically significant at the significance level p
<0,05.
Intravital observation of the morphological state of cell cultures
The method of intravital observation under an inverted microscope with photographic recording makes it possible to visually assess the morphological state of cells during their cultivation under these conditions and compare them with the control variant. Intravital observation with photographic recording during the cultivation of all types of cells (both in media containing the tested ALPs and in control) was carried out under an inverted Nikon Eclipse TS100 microscope equipped with a camera.
Calculation of drug concentrations for the experiment
The choice of ABP concentration for the experiment was based on data from the clinical use of the studied drugs. The therapeutic dose of a single use of each drug is 1 drop into the conjunctival sac of the affected eye. The volume of the drop formed by the eye dropper varies from 25 to 50 µl: the conjunctival sac can hold about 10 µl (10 cm3) of liquid. At the same time, the human conjunctival cavity normally constantly contains about 6-7 μl of tear fluid. With the eyelids closed, the tear fluid completely fills the conjunctival sac, and with the eyelids open, it is distributed over the anterior segment of the eyeball in the form of a thin precorneal tear film with an average thickness of 5-10 microns. Thus, taking into account the volume of tear fluid, the initial concentration of the drug in the conjunctival sac with a single use can vary from 70 to 90%. In experiments to determine cell proliferation by colorimetric methods, 200 μl of nutrient medium was used in 1 well of a 96-well plate. The dose of the drug was 20 and 2 μl per 200 μl of medium, which corresponds to 10 and 1% of the volume of the nutrient medium. In experiments on cell cloning, 2 ml of nutrient medium was used in 1 Petri dish with a diameter of 3 cm. The dose of the drug was 200 and 20 μl per 2 ml of medium (10 and 1% of the volume of the nutrient medium, respectively). Calculation of the concentrations of the studied drugs in the clinic and experiment is presented in the table.
Calculation of concentrations of study drugs in the clinic and experiment
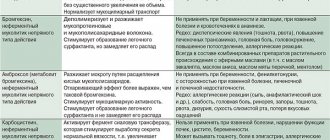
AMINOGLICOSIDES
MODERN ANTIMICROBIAL CHEMOTHERAPY
MODERN ANTIMICROBIAL CHEMOTHERAPY
L.S. Strachunsky, S.N. Kozlov. Guide for doctors
| Content | ANTIBIOTIC.ru |
Antibacterial drugs
The main clinical significance of aminoglycosides is their activity against gram-negative bacteria. Aminoglycosides have a faster bactericidal effect than β-lactams, very rarely cause allergic reactions, but are much more toxic compared to β-lactams. Aminoglycosides are classified by generation (Table 4).
Table 4. Classification of aminoglycosides
| I generation | II generation | III generation |
| Streptomycin Neomycin Kanamycin | Gentamicin Tobramycin Netilmicin | Amikacin |
GENERAL PROPERTIES
Activity spectrum
| Gram(+) cocci: | staphylococci, including PRSA and some MRSA (aminoglycosides of the II-III generations); Streptococci and enterococci are moderately sensitive to streptomycin and gentamicin. |
| Gram(-) cocci: | gonococci, meningococci - moderately sensitive. |
| Gram(-) sticks: | E. coli , Proteus (aminoglycosides of I-III generations), Klebsiella, Enterobacter, Serration (aminoglycosides of II-III generations); P.aeruginosa (aminoglycosides of II-III generations). |
| Mycobacteria: | M. tuberculosis (streptomycin, kanamycin and amikacin). |
| Anaerobes are resistant. | |
Warnings
A. Pneumococci are resistant to aminoglycosides
Therefore, it is a mistake to use them for community-acquired pneumonia.
B.
Streptococci, including the group of viridans streptococci, are generally insensitive to aminoglycosides. But when used together with penicillin, pronounced synergism is observed. Therefore, when treating, for example, bacterial endocarditis, a combination of benzylpenicillin (or ampicillin) with gentamicin (or streptomycin) is used.
IN.
Despite the fact that Salmonella and Shigella
in vitro
, these antibiotics cannot be used to treat shigellosis and salmonellosis due to low efficiency. This is due to poor penetration of aminoglycosides into human cells, where Shigella and Salmonella are localized. To avoid unnecessary testing and to avoid misleading clinicians when interpreting susceptibility results, it is not recommended to test susceptibility to Shigella and Salmonella aminoglycosides.
Pharmacokinetics
They are practically not absorbed into the gastrointestinal tract (prescribed orally for selective decontamination of the gastrointestinal tract before operations on the large intestine or in patients in the ICU). They are well absorbed when administered intramuscularly, intraperitoneally and intrapleurally. Compared to β-lactams and fluoroquinolones, they pass through various tissue barriers (BBB, GOB) worse and create lower concentrations in bronchial secretions and bile. High levels are observed in kidney tissue. They are not metabolized in the liver and are excreted unchanged in the urine. T1/2 of all drugs is 2-3.5 hours. In newborns, due to the immaturity of the kidneys, T1/2 increases to 5-8 hours.
Adverse reactions
- Ototoxicity (vestibulotoxicity, cochleatoxicity).
- Nephrotoxicity.
- Neuromuscular blockade.
Risk factors for the development of adverse reactions
- Elderly age.
- High doses.
- Long-term use (more than 7-10 days).
- Hypokalemia.
- Dehydration.
- Lesions of the vestibular and auditory apparatus.
- Kidney failure.
- Concomitant use of other nephrotoxic and ototoxic drugs (amphotericin B, polymyxin B, furosemide, etc.).
- Simultaneous administration with muscle relaxants.
- Myasthenia.
- Rapid intravenous administration of aminoglycosides or their large doses into the abdominal and pleural cavity.
Measures to prevent adverse reactions
- Do not exceed the maximum daily dose if it is not possible to determine the concentration of aminoglycosides in the blood.
- Monitor renal function before prescribing aminoglycosides and then every 2-3 days by determining serum creatinine and calculating creatinine clearance.
- Observe the maximum duration of therapy - 7-10 days, with the exception of bacterial endocarditis - up to 14 days, tuberculosis - up to 2 months.
- Do not prescribe two aminoglycosides at the same time or replace one drug with another if the first aminoglycoside has been used for 7-10 days. A repeat course can be carried out no earlier than after 4-6 weeks.
- Monitor hearing and vestibular apparatus (patient survey, audiometry if necessary).
Help measures
First of all, drug withdrawal. Hearing impairment is usually irreversible, while kidney function is gradually restored. When neuromuscular blockade develops, calcium chloride is administered intravenously as an antidote.
Drug interactions
Synergy
when combined with penicillins or cephalosporins (but not when administered in the same syringe!).
Antagonism
with β-lactam antibiotics and heparin when mixed in one syringe due to physicochemical incompatibility.
Increased toxic effects
when combined with other nephrotoxic and ototoxic drugs (polymyxin B, amphotericin B, furosemide, etc.).
Indications
- Infections of various localizations caused by gram-negative bacteria from the Enterobacteriaceae
(Escherichia coli, Klebsiella, Enterobacter, etc.) and non-fermenting bacteria (Acinetobacter,
S. maltophilia
, etc.) - aminoglycosides of the II-III generations. - Pseudomonas aeruginosa infection - aminoglycosides of II-III generations.
- Enterococcal infections - gentamicin or streptomycin must be combined with penicillin or ampicillin.
- Tuberculosis - streptomycin, kanamycin, amikacin - must be combined with other anti-tuberculosis drugs.
- Zoonotic infections: plague, brucellosis (streptomycin); tularemia (streptomycin, gentamicin).
Dosing principles for aminoglycosides
Due to the fact that severe adverse reactions may develop when using aminoglycosides, and also taking into account the peculiarities of their pharmacokinetics (excretion through the kidneys unchanged), special attention should be paid to the correct calculation of doses of aminoglycosides. There are two key points to take into account:
- the dose of aminoglycosides (not only in children, but also in adults!) should be calculated based on body weight;
- the dose should be adjusted based on the individual characteristics of the patient: age, kidney function, localization of infection.
Factors determining the dose of aminoglycosides
Frequency of administration
Traditionally, aminoglycosides were administered 2-3 times daily. However, numerous studies have shown that in many cases the entire daily dose of aminoglycosides can be administered once daily.
. With a single administration regimen, clinical efficacy is not reduced, and the frequency of adverse reactions may even decrease.
A single dose is used for most indications. The exceptions are endocarditis, meningitis, and the neonatal period.
For a single administration, aminoglycosides are best administered intravenously by drip over 15-20 minutes, since it is difficult to administer a large volume of the drug intramuscularly.
Therapeutic drug monitoring
For aminoglycosides, a relationship has been established between their concentration in the blood, the antimicrobial effect and the incidence of ototoxicity and nephrotoxicity. At the same time, the pharmacokinetics of aminoglycosides has large individual variations. As a result, when medium doses of drugs are administered, approximately half of patients experience subtherapeutic concentrations.
Table 5. Therapeutic serum concentrations of aminoglycosides
| 1. | Patient body weight Doses for adults and children over 1 month: streptomycin, kanamycin, amikacin - 15-20 mg/kg/day in 1-2 administrations; gentamicin, tobramycin - 3-5 mg/kg/day in 1-2 administrations; netilmicin - 4-6.5 mg/kg/day in 1-2 administrations. |
| 2. | Obesity/emaciation Since aminoglycosides are distributed in the extracellular fluid and do not accumulate in adipose tissue, their doses should be reduced in obesity. If the ideal body weight is exceeded by 25% or more, the dose calculated for the actual body weight should be reduced by 25%. In depleted patients, on the contrary, the dose should be increased by 25%. |
| 3. | Age It is necessary to reduce the dose of aminoglycosides in the elderly, as they experience an age-related decrease in glomerular filtration rate. Newborns should receive a relatively larger dose per kg of body weight because their volume of distribution is increased. Thus, their dose of gentamicin is up to 7.5 mg/kg/day. In general, in newborns, the dose of aminoglycosides and the frequency of administration depend on two factors: the degree of prematurity and postnatal age. This is due to the immaturity of kidney function, which develops after birth. |
| 4. | Kidney function Since aminoglycosides are excreted unchanged from the body in the urine, if renal function is impaired, the daily dose must be reduced. The most informative indicator of kidney function is the clearance of endogenous creatinine (glomerular filtration), which is calculated in adults using the Cockroft and Gault formula (Cockroft, Gault, 1976), and in children using the Schwarz formula (Schwarz, 1987). To correctly select the dose of aminoglycosides, determination of serum creatinine and calculation of its clearance must be carried out before prescribing the drug and repeated every 2-3 days. A decrease in creatinine clearance by more than 25% from the initial level indicates a possible nephrotoxic effect of aminoglycosides; a decrease by more than 50% is an indication for discontinuation of aminoglycosides. For renal failure, first single dose gentamicin, tobramycin and netilmicin is 1.5-2 mg/kg, amikacin - 7.5 mg/kg. |
| 5. | Severity and localization of infection For meningitis, pneumonia, sepsis, maximum doses are prescribed; for pyelonephritis, bacterial endocarditis - average doses. Particularly high doses are administered to patients with cystic fibrosis and burns, since the distribution of aminoglycosides is significantly impaired in them, but it is desirable to determine the concentration of aminoglycosides in the blood. |
| A drug | Concentration, µg/ml | |
| peak, no less | residual, no more | |
| Gentamicin | 6-10 | 2 |
| Tobramycin | 6-10 | 2 |
| Netilmicin | 6-10 | 2 |
| Amikacin | 20-30 | 10 |
When conducting therapeutic drug monitoring, the following is determined:
| 1) | peak concentration of aminoglycosides in blood serum - 60 minutes after intramuscular administration of the drug or 15 minutes after the end of intravenous administration; |
| 2) | residual concentration - before administering the next dose. |
Establishing a peak concentration not lower than the threshold value (Table 5) indicates that the dose of aminoglycoside used is sufficient, while its high levels do not pose a danger to the patient. The value of the residual concentration exceeding the therapeutic level indicates the accumulation of the drug and the danger of developing toxic effects. In this case, reduce the daily dose
or
lengthen the interval between single doses
. With a single administration of the entire daily dose, it is sufficient to determine only the residual concentration.
CHARACTERISTICS OF INDIVIDUAL DRUGS
STREPTOMYCIN
The first aminoglycoside antibiotic. It has high cochleatoxicity and especially vestibulotoxicity, but is the least nephrotoxic of the aminoglycosides. Microflora resistance to it quickly develops.
Indications
Currently limited to the following diseases:
- tuberculosis;
- bacterial endocarditis caused by viridans streptococci or enterococci (in combination with penicillin or ampicillin);
- brucellosis, tularemia, plague (in combination with tetracycline).
Dosage
Adults and children
Parenteral - 15 mg/kg/day (no more than 2.0 g/day) in 1-2 administrations.
For tuberculosis
Adults
Intramuscularly - 1.0 g 2 times a week.
Children
Intramuscularly - 20 mg/kg/day 2 times a week.
Release forms
Bottles of 0.25 g, 0.5 g, 1.0 g and 2.0 g of powder for the preparation of solution for injection.
NEOMYCIN
One of the most ototoxic drugs. Parenteral administration is prohibited. Sometimes used internally for selective decontamination of the gastrointestinal tract before operations on the large intestine and locally (included in some ointments in combination with glucocorticoids). Not used in children.
Dosage
Adults
Orally - 0.5 g every 6 hours for 1-2 days.
Release forms
Tablets of 0.1 g and 0.25 g; 0.5% and 2% ointment.
KANAMYCIN
Outdated drug. Unlike aminoglycosides of the second generation, it acts on M. tuberculosis
, but is inferior to them and amikacin in activity against nosocomial strains of gram-negative flora. Does not affect Pseudomonas aeruginosa.
It has high ototoxicity and nephrotoxicity.
Retains its value in tuberculosis as a second-line drug. It can be used orally for the same indications as neomycin.
Dosage
Adults
Orally - 2-3 g every 6 hours; parenterally - 15 mg/kg/day in 1-2 administrations.
Children
Parenteral - 15 mg/kg/day in 1-2 administrations.
Release forms
Tablets of 0.125 g and 0.25 g; bottles of 0.5 g and 1.0 g of powder for the preparation of solution for injection.
GENTAMICIN
Garamycin
The main aminoglycoside of the second generation. Acts on Pseudomonas aeruginosa.
Compared to streptomycin, it is more nephrotoxic, but less ototoxic.
Indications
- Nosocomial pneumonia (with low level of resistance).
- UTI infections.
- Intra-abdominal and pelvic infections (in combination with antianaerobic drugs).
- Bacterial endocarditis (in combination with penicillin or ampicillin).
- Sepsis (in combination with β-lactams).
- Tularemia.
Warnings
Currently, due to the widespread (often unjustified) use of gentamicin, many nosocomial microorganisms, primarily Pseudomonas aeruginosa and Klebsiella, have acquired resistance to the drug.
A serious mistake is the use of gentamicin for community-acquired pneumonia, since gentamicin, like other aminoglycosides, does not act on pneumococci.
Dosage
Adults and children
Parenteral - 3-5 mg/kg/day in 1-2 administrations.
Newborns
Parenteral - 5-7.5 mg/kg/day in 2-3 administrations.
Release forms
Bottles of 0.08 g of powder for the preparation of solution for injection; ampoules of 1 ml and 2 ml of 4% solution (40 mg/ml); 0.1% ointment.
TOBRAMYCIN
Nebtsin, Brulamytsin
Compared to gentamicin, it is more active against Pseudomonas aeruginosa, but in most cases there is co-resistance to both drugs. Does not affect enterococci. Less nephrotoxic.
Indications
- Nosocomial pneumonia.
- UTI infections.
- Intra-abdominal and pelvic infections (in combination with antianaerobic drugs).
- Sepsis (in combination with β-lactams).
Dosage
Adults and children
Parenteral - 3-5 mg/kg/day in 1-2 administrations.
Release forms
Ampoules of 1 ml and 2 ml of 4% solution (40 mg/ml).
NETILMICIN
Netromycin
Active against some nosocomial strains of gram-negative bacteria resistant to gentamicin. Compared to gentamicin, it has slightly less ototoxicity and nephrotoxicity.
Indications
- Nosocomial pneumonia.
- UTI infections.
- Intra-abdominal and pelvic infections (in combination with antianaerobic drugs).
- Bacterial endocarditis (in combination with ceftriaxone).
- Sepsis (in combination with β-lactams).
Dosage
Adults and children
Parenteral - 4-6.5 mg/kg/day in 1-2 administrations.
Release forms
Solution for injection in 2 ml bottles containing 0.05 g or 0.15 g of netilmicin.
AMICACIN
Amikin
Effective against many strains of gram-negative bacteria (including P.aeruginosa
), resistant to gentamicin and other second generation aminoglycosides.
Active against M. tuberculosis
. Does not affect enterococci.
Compared to gentamicin, it is slightly less nephrotoxic.
Indications
Used to treat infections caused by multidrug-resistant gram-negative microflora. The most preferred among aminoglycosides for the empirical treatment of nosocomial infections.
- Nosocomial pneumonia.
- UTI infections.
- Intra-abdominal and pelvic infections (in combination with antianaerobic drugs).
- Sepsis (in combination with β-lactams).
- Tuberculosis (II line drug).
Dosage
Adults and children
Parenteral - 15-20 mg/kg/day in 1-2 administrations.
Release forms
Solution in ampoules containing 0.1 g, 0.25 g and 0.5 g of amikacin; solution in vials containing 1.0 g of amikacin.
| Copyright © 2000-2007 ANTIBIOTIC.ru Posted: 05/15/2004 |
The address of this page: https://www.antibiotic.ru/books/mach/mac0108.shtml
Last modified date: 05/24/2004 18:56
Results and discussion
The effect of antibiotics on the efficiency of cloning was assessed on CHO-K1 cells in 2 series of experiments with different concentrations of the studied drugs (1 and 10%) in the volume of the nutrient medium. The results of a series of experiments on the efficiency of cloning cells of the CHO-K1 line in the presence of the studied drugs at a concentration of 1% of the volume of the nutrient medium showed that the efficiency of cloning in the experimental variants was lower than in the control. Netilmicin was the closest to the control in terms of cloning efficiency - 73%. Tobramycin showed the most pronounced cytotoxic effect on cells. The cloning efficiency in this variant was only 13%. At a concentration of the tested ABPs of 10% of the volume of the nutrient medium, cells of the CHO-K1 line formed clones only in the presence of netilmicin, and the cloning efficiency in this variant was 57%. Ciprofloxacin and tobramycin at the same concentration showed a high degree of cytotoxicity when cells were sparsely seeded. The results are presented in Fig. 1.
Rice. 1. Histograms of the efficiency of cloning cells of the CHO-K1 line on the 5th day of cultivation in a medium with a concentration of the studied drugs of 1 and 10% of the volume of the nutrient medium. K - control, 1 - ciprofloxacin, 2 - tobramycin, 3 - netilmicin.
In Fig. Figure 2 shows the differences in the morphology of clones and individual cells in the control and experimental variants. Colonies in the control are dense, formed from 100 or more cells with an epithelial-like morphology typical of the CHO-K1 line. The variant with netilmicin is closest to the control in terms of these morphological characteristics. In this variant, clones with both dense and diffuse structure, formed from 80–90 cells, were identified. In the variant with ciprofloxacin, the clones have a looser structure (diffuse structure) and consist of 15-20 cells. In the variant with tobramycin, the colonies are very small (consisting of less than 10 cells) and diffuse. Cells in these variants do not always have the characteristic epithelial-like morphology. There are many rounded and elongated cells, their structure is granular, with vacuoles, which indicates their insufficiently good physiological condition. These data allow us to conclude that the tested antibiotics at a concentration of 1% of the volume of the nutrient medium have a cytotoxic effect of varying degrees on CHO-K1 cells. The most toxic effect on cells was detected for tobramycin. Netilmicin showed the least cytotoxic effect.
Rice. Fig. 2. Morphology of cells of the CHO-K1 line in clones formed after 5 days of cultivation in a medium with a concentration of the studied drugs of 1% of the volume of the nutrient medium (×20).
The effect of antibiotics on proliferation was determined on cells of the CHO-K1 line, FK and cells of the Clone 1−5C-4 line. With each type of cell, 2 series of experiments were performed with different concentrations of the studied drugs (1 and 10%) in the volume of the nutrient medium. Testing by photocolorimetric analysis revealed that at a concentration of the studied drugs of 1% of the volume of the nutrient medium, netilmecin was the least toxic for all types of cell cultures, which showed practically no cytostatic effect. At a concentration of 10% of the volume of the nutrient medium, the toxic effect of this drug on all types of cells is moderate, while tobramycin and ciprofloxacin exhibit a high degree of toxicity for all types of cells both at a concentration of 1% of the volume of the nutrient medium and at a concentration of 10 %. This effect was most pronounced on cells of the CHO-K1 and Clone 1−5C-4 lines.
The results of experiments on cells of the CHO-K1 line, FK and cells of the Clone 1−5C-4 line with a concentration of tested antibiotics of 10 and 1% of the volume of the nutrient medium, obtained using the photocolorimetric analysis method, are shown in Fig. 3.
Rice. 3. Histograms assessing the proliferation of cells of the CHO-K1 line, FK and cells of the Clone 1−5C-4 line on the 6th day of cultivation in a medium with a concentration of the studied drugs of 1 and 10% of the volume of the nutrient medium. K - control, 1 - ciprofloxacin, 2 - tobramycin, 3 - netilmicin.
Using a photocolorimetric method for determining proliferation, the cytotoxic effect of the studied drugs on all types of cells was established in the following sequence (in descending order of toxicity): tobramycin→ciprofl-oxacin→netilmicin.
The morphological state of cells of the CHO-K1 line, FK and cells of the Clone 1−5C-4 line, cultured in media containing the studied drugs at a concentration of 1 and 10% of the volume of the nutrient medium, is presented in Fig. 4, 5.
Rice. 4. Cells of the CHO-K1 line, FK and cells of the Clone 1−5C-4 line on the 6th day of cultivation in a nutrient medium containing 1% of the studied drugs (×10).
Rice. 5. Cells of the CHO-K1 line, FK and cells of the Clone 1−5C-4 line on the 6th day of cultivation in a nutrient medium containing 10% of the studied drugs (×10).
As can be seen in those shown in Fig. 4, 5 photographs, all types of cells in the control variants have their typical morphology (cells of the CHO-K1 and Clone 1−5C-4 lines are epithelial-like, FC - fibroblast-like) and on the 6th day of cultivation they formed a confluent monolayer. At a concentration of the tested drugs of 1% of the volume of the nutrient medium, the experimental variants with netilmicin turned out to be closest to the control in terms of the morphological state of all types of cells and the degree of monolayer formation. In the presence of tobramycin and ciprofloxacin in a nutrient medium at the same concentration, none of the cell types formed a subconfluent monolayer. In experimental variants with these preparations, the cells are spread out, but there are few of them; many rounded and elongated cells are revealed, their structure is granular, with vacuoles, which is a sign of the depressed state of the cells. These data allow us to conclude that the tested antibiotics at a concentration of 1% of the volume of the nutrient medium have a cytotoxic effect of varying degrees on all types of cells. Regardless of the cell test system used, the most toxic effect was detected for tobramycin. Netilmicin showed the least cytotoxic effect on the cells of all test systems. At a concentration of the tested drugs of 10% of the volume of the nutrient medium in the experimental variants with tobramycin and ciprofloxacin, a monolayer was not formed. The cells of all test systems in the presence of these drugs in a nutrient medium at a given concentration have a round shape, which indicates their suppressed viability. In the nutrient media of all test systems in the presence of ciprofloxacin, the formation of crystals of the drug was detected. These data allow us to conclude that ciprofloxacin and tobramycin at a concentration of 10% of the volume of the nutrient medium have a highly toxic effect on all types of cells. Experimental variants with netilmicin, present in the culture media at a concentration of 10%, turned out to be close to the control both in terms of the degree of monolayer formation and in the morphological state of the cells of all test systems.
The results of assessing the cytotoxicity of the third generation aminoglycoside antibiotic - netilmicin, the second generation - tobramycin and the second generation fluoroquinolone antibiotic - ciprofloxacin, obtained in this in vitro
, showed that these drugs have varying degrees of cytotoxicity. Regardless of the method used to assess the general toxicity of the antibiotics tested in this work, the toxic effect of each drug on a specific cell type was revealed. The greatest toxic effect for all types of cells used as test systems in this work was exhibited by the second generation aminoglycoside antibiotic tobramycin. The least toxic and closest to the control in terms of toxicity for all types of cells used as test systems in this work was the third generation aminoglycoside antibiotic netilmicin.