The article was checked by gastroenterologist E.G. Melnikova. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
At the Clinical Hospital on Yauza, diagnostics and treatment of diseases are carried out, in which there is stool with blood, mucus, and black feces. Quick diagnosis includes all the necessary tests - blood, urine, feces, and modern research methods - ultrasound, endoscopic with advanced capabilities (in monochrome light, endosonography), real and virtual colonoscopy (CT version). Conservative and high-tech surgical treatment is carried out (including endoscopic and laparoscopic, abdominal and proctological operations).
Blotches or streaks of blood in the stool appear against the background of the following factors:
Haemorrhoids
The disease is characterized by varicose veins of the anus and rectum. This condition is accompanied by the appearance of hemorrhoids. It develops against the background of stagnation due to a sedentary lifestyle, constipation and excessive body weight. Hemorrhoids also occur during pregnancy.
Characterized by the appearance of dark red blood during bowel movements. It does not mix with feces. Accompanied by itching and burning.
Anal fissure
Accompanied by a rupture of the intestinal mucosa mainly on the wall of the anus. In this case, pain is felt during defecation. The discomfort persists for several hours. Over time, the cracks change - replacement of the mucous tissue with connective tissue is observed.
Colorectal cancer
The malignant process develops due to the degeneration of polyps. Most often it is a hereditary disease. Risk factors include Crohn's disease and ulcerative colitis. The progression of the malignant process occurs slowly. It is characterized by the presence of hidden blood in the stool, weakness, weight loss and anemia.
Ulcerative colitis
Chronic inflammation of the colon mucosa is characterized by the appearance of bloody diarrhea. There are also mucus impurities in the stool. Abdominal pain is not a characteristic symptom. The stool is watery and contains mucus. The complicated course of a chronic disease is accompanied by fever, intoxication of the body, spastic pain and an increase in anemia.
Intestinal inflammation
The inflammatory process occurs against the background of various infectious diseases of a bacterial, viral or parasitic (protozoal) nature: enterovirus, salmonellosis, dysentery, amoebiasis, etc.
Ulcer perforation
If the ulcer perforates, intense bleeding occurs. Accompanied by severe pain in the upper abdomen, dry mouth, excessive sweating and vomiting (black-brown masses).
Intestinal diverticulosis
It is characterized by inflammation of hernial protrusions, which are located on the intestinal walls. The disease does not manifest itself until the inflammatory process develops. Accompanied by hyperthermia and abdominal pain on the left side. Diarrhea or constipation, nausea and vomiting are also common. In case of rupture of diverticula, the development of peritonitis is observed.
Crohn's disease
An inflammatory process affecting the intestinal walls. Accompanied by the appearance of nodules (granulomas). This condition cannot be completely cured - you can only achieve remission. Numerous ulcers appear on the mucous membrane. Bleeding is observed only when the disease is complicated.
How to detect blood in stool
Blood in stool leads to anemia
It often happens that blood in the stool is the only symptom that something incomprehensible is happening in the body. It is very important to pay attention and not miss the following:
- The appearance of blood streaks in the stool that look like “worms”
- Scarlet blood, which can be either on the surface of the stool or remain on toilet paper
- Loose stools with foam and blood
- The stool is liquid, and besides, it contains not only blood, but also mucus. This chair will be somewhat reminiscent of jelly.
- The stool looks like plasticine
- The stool has turned black, and this has nothing to do with eating any food
- In addition, it is worth paying special attention to when blood flows from the anus. Sometimes it's even difficult to stop her. In this case, you should definitely call an ambulance.
Prevention
Preventive measures include timely diagnosis and the appointment of adequate treatment for the pathological process in the body. Also organize proper nutrition to prevent bowel movements.
FAQ
What to do if there is blood in the stool?
If you have bloody stools, consult your doctor to determine the cause. The doctor refers the patient for a comprehensive examination and, based on the results obtained, prescribes treatment.
What examinations need to be completed?
Laboratory diagnosis is required. Recto- and anoscopy are also prescribed to determine pathological changes in the intestinal mucosa.
You can see prices for services
Causes of Visible Blood
In most cases, blood, after it appears in the stool, can be seen with the naked eye. True, not everyone examines their bowel movements, and therefore do not always notice this manifestation. The most common reasons why blood may appear in the stool, and at the same time it will be visible, include:
- Anal fissure. Sometimes patients notice that after bowel movements they feel pain, and during it too. And if you pay attention to the feces, you can see traces of blood on its surface. This indicates that a crack has appeared. The most common cause of anal fissure is recurrent constipation, for which many people go untreated. In this case, blood may be present in the stool for several days until the wound heals. But the next time you touch it, it will start bleeding again
- Haemorrhoids. One of the most common causes of the presence of blood in the stool is hemorrhoids, which also manifests itself with other symptoms, such as itching, pain, burning, and sometimes prolapse of hemorrhoids. Hemorrhoids appear against the background of swelling of the veins, as a result of which, in severe stages, when the veins are damaged by feces, bleeding may begin. Typically the blood will be dark in color.
- Nonspecific ulcerative colitis, during which ulcerations appear on the mucosa and submucosa. In addition to the fact that there will be blood in the patient's stool, traces of pus oozing from the ulcers will also be found. Usually, a person’s well-being sharply deteriorates, he has all the signs of intoxication of the body, diarrhea, abdominal pain
- Crohn's disease, which is considered a hereditary disease, can develop as a result of measles and food allergies. In addition to blood, the stool will be loose, a skin rash, and fever will appear.
- Intestinal infections, which can be of either bacterial or viral origin. If you do not pay attention to this problem in time, blood will appear in the stool due to irritation and inflammation of the mucous membrane.
- Tumors in the intestines, both malignant and benign, which over time begin to put pressure on the blood vessels, causing them to rupture and, as a result, the appearance of blood in the stool
- Dysbacteriosis, especially when it is caused by clostridium
- Sexually transmitted infections
Depending on what caused the appearance of blood in the stool (when a person sees it independently), the treatment prescribed by a specialist will depend. Because it is very important not only to eliminate the symptoms, but also to remove the source of the problem itself.
Blood in the stool (medical: hematochezia, melena) is seen by most patients as something terrible. If you notice blood in your stool, you don’t have to worry about the worst, but you should immediately consult a doctor. Possible causes of blood in the stool include gastrointestinal infections, colon polyps or hemorrhoids, stomach ulcers or chronic inflammatory disease of the large intestine. To exclude the diagnosis of malignant diseases - such as intestinal cancer - it is necessary to immediately conduct appropriate research in the clinic. Below you will learn all the important information about the “blood in the stool” symptom.
Blood in the stool: Description
Blood in the stool indicates that the body is losing blood somewhere inside the gastrointestinal tract, which is then found mixed in the stool. The color and consistency of mixed blood can serve as an almost reliable indication of where the source of bleeding is located.
Blood in stool does not necessarily appear as a bright red or dark red coating or impurity; in fact, it can turn the stool black. The corresponding manifestations depend on the level of bleeding in the digestive tract, since the state of the blood changes upon contact with gastric juice and as a result of processing by microorganisms.
Red blood in the stool (hematochezia)
If the blood in the stool is bright red or dark red, in the form of impurities or streaks, then the blood is relatively fresh. This type of blood in the stool is called hematochezia. The source of bleeding is most likely in the middle or lower parts of the gastrointestinal tract (GIT), because the blood could not be destroyed in large quantities either by the hydrochloric acid of the stomach or by bacteria.
If the stool is uniformly dark red, this may indicate, for example, major bleeding in the large intestine. With minor bleeding, jelly-like traces of blood are observed in the stool.
In turn, light red stripes may indicate fresh bleeding in the rectal area, for example, with hemorrhoids.
Black blood in stool (melena, tarry stool)
If the stool is black and shiny, then we are talking about the so-called tarry stool (melena). When bleeding in the upper gastrointestinal tract, that is, from the esophagus to the duodenum, hemoglobin in the blood breaks down into hematin upon contact with gastric juice. This hematin is the cause of black stools, and in cases of vomiting, the vomit may resemble coffee grounds.
Black stool most often indicates that the source of the bleeding is higher than the small intestine and is caused by either a stomach ulcer or bleeding in the esophagus.
Since intestinal bacteria, with prolonged contact with blood, also cause the breakdown of hemoglobin into the pigment hematin, black stool may not necessarily be a consequence of bleeding in the upper gastrointestinal tract. When the passage of chyme (intestinal contents) is slow, melena can be caused by bleeding located deeper.
Under certain circumstances, high-lying bleeding in the gastrointestinal tract, on the contrary, can lead to hematochezia, both when the secretion of gastric juice decreases due to medication, and in case of severe bleeding, when chyme quickly passes through the intestines.
Hidden blood in stool
It may also be that although there is blood in the stool, it is not visible. Then we are talking about hidden blood. In most cases, it is discovered incidentally during a routine examination or during a targeted examination of known damage to the digestive tract.
Since blood cannot be detected with the naked eye, a guaiacol test for detecting blood in stool (hemoccult test) is used, which can detect even small quantities.
Cases that are confused with the presence of blood in the stool
After eating certain foods, your stool may look like there is blood in it. This is caused by the consumption of red beets, which stain the stool dark red, which occurs with hematochezia. Blueberries turn the stool black, similar to licorice, so that when examined, it is perceived as melena.
Also, some medications can cause black stool (for example, activated charcoal or iron supplements).
Blood in the stool: Causes and possible diseases:
Various possible reasons for the appearance of blood in the stool, causing bleeding in the gastrointestinal tract, are being considered. These include bleeding from the oropharynx, esophagus, stomach, small and large intestines and anus. In principle, bleeding can occur in every department, with the frequency and significance of different causes varying.
Blood in the stool due to bleeding in the upper digestive tract
- The most common cause of bleeding in the upper digestive tract is ulcers in the stomach and duodenum, often caused by Helicobacter pylori bacteria or long-term use of certain medications, such as aspirin.
- Chronic heartburn can, when gastric juice gets in, lead to inflammation of the esophagus (reflux esophagitis) and, as a result, bleeding.
- With certain liver diseases, a redistribution of venous blood flow occurs, which causes varicose veins of the esophagus. Such dilated veins easily rupture and lead to severe, often life-threatening bleeding.
- After profuse vomiting, extended tears of the mucous membrane may occur at the junction of the esophagus and the stomach. Then we are talking about Mallory-Weiss syndrome, often found in alcoholics who have previously had damaged mucous membranes.
- Finally, blood in the stool can also be a likely symptom of stomach cancer.
- In the middle sections of the digestive tract, the most common cause of bleeding is tumors of the small intestine. Also in the large intestine, atypical growths can lead to the appearance of blood in the stool. They do not have to be malignant.
- Particularly in young patients, chronic inflammatory bowel diseases such as Crohn's disease or ulcerative colitis can cause bleeding. If in the latter case only the colon and rectum are affected, then in Crohn's disease the entire gastrointestinal tract [can] be affected. The exact causes of both diseases are unknown.
- Polyps are most often benign growths of the large intestine that usually do not cause any problems, but as their size increases, the risk of bleeding also increases. They can also develop into pre-cancerous conditions, so after a certain size they are mostly removed. The consequence of such interventions, in turn, may be secondary bleeding.
- With diverticula, we are talking about protrusions of the walls of the intestinal wall, which, when viewed from the inside, are small “pits”. Diverticula most often form and are found in the large intestine. Depending on the circumstances, they can become inflamed (then we are talking about diverticulitis) and cause bleeding.
- Various intestinal infectious diseases, ranging from common gastroenteritis to severe diseases such as typhus or dysentery, can cause blood in the stool, most often in combination with diarrhea. Also, excessive proliferation of bacteria that make up the natural intestinal microflora, for example, after [a course of] antibiotic therapy, can cause hematochezia. An example is pseudomembranous colitis.
- Bright red blood in the stool often occurs with hemorrhoids. This usually refers to a pathological increase in arteriovenous anastomoses under the rectal mucosa. During defecation, they are often damaged, resulting in a coating of fresh, often bright red blood.
- Elderly people often experience so-called mesenteric infarctions, that is, blockage of intestinal vessels. If the tissues of the affected areas are damaged, subsequent bleeding may occur.
Blood in the stool due to bleeding in the middle and lower parts of the digestive tract
Blood in the stool: When should you see a doctor?
If you find blood in your stool, you should consult a doctor in any case. Despite the fact that most bleeding stops on its own without medical help and is often not dangerous. It is still necessary to find out where the source of the bleeding is and whether there is a more serious disease behind it. Especially if you have other symptoms, such as:
- Pain in the stomach and abdomen.
- Pain during bowel movements.
- Nausea and vomiting (including in the presence of blood in the vomit).
- Prolonged lethargy and fatigue.
- Pronounced weight loss in a short time.
- Night sweats.
You can't put off visiting a doctor.
If there is severe bleeding in the digestive tract after a certain period of time, anemia (anemia) may occur due to blood loss, which in any case requires treatment.
Blood in the stool: What does the doctor do?
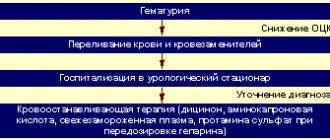
If blood in the stool is caused by acute bleeding in the gastrointestinal tract, resulting in severe blood loss, it is necessary first of all to replace the missing blood volume. If left untreated, in worst cases it can lead to spinolaemic shock, a life-threatening condition.
The patient is placed in a supine position, receives oxygen through a nasal tube and, as soon as possible, a blood substitute to replenish lost blood volumes. In case of large blood losses, blood transfusions are also performed.
Also, with chronic bleeding in the gastrointestinal tract over a long period of time, anemia may develop, the treatment of which is similar [to the treatment of acute blood loss].
History and investigations
If a patient consults a doctor complaining of blood in the stool, in most cases the location of the bleeding is unknown and must be determined.
Medical history data can provide valuable guidance. For example, it may be important whether there has been blood in the stool before. It should also be clarified whether there were previously hemorrhoids, peptic ulcers, chronic inflammatory bowel diseases, alcohol abuse or diverticula, that is, whether there are risk factors for gastrointestinal bleeding. Next, studies are carried out to detect the source of bleeding.
- Of great importance in this case is gastroendoscopy, in which a gastric tube (gastroenteroscope) is inserted through the mouth and allows the doctor to assess the condition of the esophagus, stomach and duodenum using an endoscope. When examining the large intestine (coloscopy), the endoscope is inserted into the rectum and can be inserted down to the final part of the small intestine. Using these examination methods, many possible causes can be detected, such as diverticulum, chronic inflammation, ulcers, esophageal varices, colon polyps and other growths. Rectoscopy is most often used to examine hemorrhoids. Although the nature of the blood in the stool, as well as possible previously established diseases, can indicate the location of the source of bleeding, it is still better to use gastroduodenoscopy, especially in cases where the specific lesion cannot be identified.
Since gastroduodenoscopy cannot always determine the source of bleeding and, in addition, it is not always possible to obtain sufficient data, in such cases additional research methods are used.
- Double-balloon enteroscopy allows you to examine the condition of the small intestine. In this case, two balloons attached to the endoscope are alternately inflated so that they can be advanced along the length of the endoscope. This study is usually carried out in two stages - examination of the upper part of the small intestine with insertion of a probe through the mouth, and the lower part through the anus.
- Meanwhile, it is also possible to perform video capsule endoscopy. In this case, the patient swallows a mini-camera, which takes pictures at certain intervals. This way the small intestine is examined. However, this method takes time and does not allow precise localization of the source of bleeding.
- Ultrasound can help identify blockages in blood vessels as a possible cause of blood in the stool.
- Further, nuclear medicine techniques and selective arteriography can be used, which can detect only active bleeding.
- If it is suspected that the cause of blood in the stool is an infection, an attempt is made to identify the corresponding pathogen using stool and blood cultures.
Therapeutic measures
Treatment depends on the cause of the bleeding. First of all, you should, of course, stop active bleeding, then you need to prevent recurrent bleeding by fighting the cause.
In order to stop active bleeding in the digestive tract, various endoscopic techniques are first used. It is advisable that if the source of bleeding is detected during gastro- or colonoscopy, the cause of the bleeding can also be eliminated using one of the following methods:
- bleeding can be stopped, for example, with a hemoclip - a type of clamp that compresses the affected area.
- There are also injection techniques, in which a solution of adrenaline is injected into the site of bleeding with a needle, which compresses the blood vessels, or so-called fibrin glue can be injected.
- It is possible to use a laser to cauterize the bleeding site.
- The source of bleeding can be cut out microsurgically.
- In the case of esophageal varices and hemorrhoids, latex ligation is often used.
When the bleeding has stopped, treatment begins to eliminate the cause of the disease:
- For peptic ulcers, an attempt is made to reduce the production of stomach acid with the help of certain medications (proton pump inhibitors, PPIs), and dietary therapy can also be carried out. In case of Helicobacter pylori , a combination of various antibiotics is used.
- The cause of varicose nodes in the esophagus is high pressure in the portal vein system, and therefore they try to reduce it with the help of medications (beta blockers, spironolactone).
- Chronic inflammatory bowel diseases require special treatment, using anti-inflammatory drugs - glucocorticoids.
- Diverticulitis is treated with antibiotics. If this is no longer possible, the affected area of the intestine is removed.
- Intestinal polyps are also usually removed.
- For malignant diseases, surgery, chemotherapy and radiation therapy are considered.
How to contact us
Email: Tel.: +49 212 5476913 Viber | WhatsApp: +49 173-2034066 | +49 177-5404270 For your convenience, please save the phone number in your phone book and call or write to us for free on WhatsApp, Viber or Telegram. Applications made on weekends or holidays will be processed on the first business day.
Causes of occult blood
Stool with blood is an alarming symptom
Sometimes it happens that a person cannot see blood in the stool on his own, since there are no visible traces. This usually happens when blood in the intestines and in the stool itself enters from the upper parts of the digestive system, that is, when it reaches the end, it manages to change color.
Hemoglobin, which is present in the blood, breaks down under the influence of acids, and therefore the feces literally become black. The main reasons for this phenomenon include:
- Bleeding from dilated veins in the esophagus. In addition to the fact that the stool will change color, it will also become tarry. In addition, immediately after eating a person will experience severe pain in the chest and vomit blood.
- Mallory-Weiss syndrome, in which a blood fissure forms in the esophagus or in one of the parts of the stomach. This usually happens to people who drink or those who do not treat stomach ulcers.
- Bleeding from a stomach ulcer or duodenal ulcer, when stool can be several times a day, and black in color. In addition, the person will be in pain, and the body temperature may also increase
- Perforation of a duodenal ulcer, in which the person’s condition will be as if he had lost a lot of blood, that is, dizziness, weakness, loss of consciousness. In addition, there will be blood in the stool
- Stomach cancer, especially in the later stages. It may be accompanied by other symptoms, such as weakness, anemia, aversion to any meat products
- Tumors of the esophagus, which at the moment will be in the stage of decay
- Stomatitis, both in adults and children
Due to the fact that not everyone pays attention to their stool, especially not paying attention to its color, many diseases are detected already in the last stages, when it is difficult and simply unrealistic to change something. That is why you need to be sensitive to your health and listen to your body in order to notice any changes in time and consult with a specialist about this.
Diagnosis of altered blood in stool
Blood in stool can be secretive
And if in the case of visible blood in the stool there is no need to carry out special diagnostics, since everything is already visible, then in the case of altered blood it is necessary to undergo a series of studies to make sure that it is blood and not the influence of certain food products. The most important test that allows you to determine whether there is hidden blood in the stool or not is the Gregersen test, or in other words, the Gregersen reaction.
In order to pass this test, you need to prepare. Three days before donating stool, you should not brush your teeth, eat meat or fish, or take any vitamins that contain iron. Then the person’s stool is collected, and a special mixture is applied to its surface, which allows blood to be detected.
Diagnostics
- determines the inflammatory process;
- diagnoses anemia caused by blood loss;
- determines dysbacteriosis, worms, hidden blood;
- (CA 19-9, CA-50, REA) – establishes the presence of malignant processes in the body.
Diagnosis of diseases accompanied by bloody stools involves identifying the degree of anemia and inflammation, establishing the location and cause of bleeding.
At the medical center on Yauza you can undergo a full range of diagnostic tests: general analysis of urine, blood, stool, stool examination for dysbacteriosis, worms, occult blood, all types of biochemical and oncological markers.
Ultrasound diagnostics, intestinal radiography, computed tomography on a modern tomograph (including virtual colonoscopy) will help to visually determine the pathological process.
Experienced and qualified radiology and endoscopic diagnostic doctors, together with gastroenterologists, surgeons, and coloproctologists, will give an objective assessment of the health status of the patient with blood in the stool and help eliminate the threat as soon as possible and achieve good results in individually selected treatment.
Approximately 30-50% of people over 25 years of age have intestinal diseases, which subsequently develop into serious chronic pathologies. Don't be fooled by false modesty. Make an appointment with your doctor today for a healthy tomorrow.
Causes of blood in stool in children
Children are no different from adults. And if many people think that they simply cannot have some problems, then they are deeply mistaken. The child's body is absolutely the same as the adult's body. The only difference is the size of the organs. Therefore, all the reasons described above can be applied to children. However, you need to remember that mainly blood in the stool in children can appear for the following reasons:
- Intestinal dysbiosis. Today, this is one of the most common problems in children of any age, since, despite the promotion of a healthy diet and the availability of many food products specifically for children (formulas, purees, etc.), not all parents adhere to this. And there are those who feed their baby cabbage soup at six months. As a rule, dysbiosis in children appears after taking antibiotics, when a course of bifidobacteria has not been taken. To be sure that the cause of blood in the stool is dysbacteriosis, it is necessary to undergo bacterial culture tests. After the results are received, the doctor will prescribe treatment. But the most important thing is to follow the correct diet for some time and eliminate all irritating foods.
- Intestinal obstruction. One of the most dangerous reasons for the presence of blood in a child’s stool is intestinal obstruction, which occurs as a result of frequent constipation, congenital anomalies, poor nutrition, and early introduction of complementary foods. Most often, obstruction is diagnosed in children under two years of age. If we talk about the symptoms of manifestation, then immediately after eating the child will cry loudly and a lot, and then, after a while, he will simply spit up like a fountain. This symptom will also be accompanied by frequent stools with mucus and blood. But after a couple of hours, the stool will turn into a dangerous lump of mucus and blood. From this moment the most dangerous stage begins, during which, if you do not call an ambulance, the child will completely refuse water and food and fall into a state of shock.
- Food allergies. Parents often notice that their child’s skin breaks out on some food product. But sometimes allergies can be manifested by the presence of blood in the stool, as well as foamy stools. As a rule, such a manifestation can occur when a child consumes milk, citrus fruits, and various food additives.
If there is a suspicion of one of the above reasons, or in general the child has stool in the blood, it is necessary to visit a doctor as soon as possible so that he can determine the cause and prescribe treatment.
When to call an ambulance
Bloody feces are a symptom of various diseases
There are a number of cases, both with adults and children, when when blood appears in the stool, it is necessary to urgently call an ambulance. Such cases include:
- Frequent loose stools, especially in children, because dehydration may develop. And if a child loses 10 to 20 percent of fluid, this can be fatal
- Frequent vomiting, which is also dangerous for children. But even in the case of adults, if you cannot stop it, it is better to call an ambulance
- High body temperature, especially when it cannot be brought down for a long period of time
- Severe pain in the abdominal area, such that the person begins to lose consciousness
- Vomiting blood
Sometimes an ambulance can give several injections on the spot, administering the necessary drugs, and leave. But in the case of children, they usually offer to go to the hospital, which in no case should be refused. Because in the hospital, with the help of medications and IVs, the child will quickly be brought back to normal. In addition, he will be under the constant supervision of qualified doctors who can provide assistance at the right time.
Many people immediately become concerned if they see blood in their stool. And this is a normal reaction, because blood cannot appear here just like that. This is one of the important and often the main symptoms of bleeding caused by destructive processes in the intestines that need to be treated, and the sooner the better.