Free and general T3
T3 is found in the human body in several forms, often in the direction of analysis you can see total and free T3.
Total T3 is a hormone that contains bound and free shares of the hormone in the blood. But some react with protein molecules, and also interact with the tissues and cells of the body in various ways. Such a hormone is called bound, and its remaining molecules form free triiodothyronine. It does not react with any other substances, but simply “travels” throughout the body as part of the blood.
A general blood test for T3 shows the total concentration of bound and free hormone. It must be said that it is not carried out as often as a free analysis, since the results are influenced by many external factors.
However, in some cases such analysis is necessary, for example, when:
- disruption of the pituitary gland and thyroid gland;
- sudden weight gain;
- presence of edema;
- disruption of the menstrual cycle;
- severe PMS;
- painful menstruation.
Reference! The main difference between total and free T3 hormone analyzes is accuracy and information content. Therefore, a free T3 test is most often prescribed.
Thyroid hormones
- T3 general
- T4 general
- T3 free
- T4 free
- TSH (thyroid stimulating)
- Antibodies to thyroglobulin (AT-TG)
- Antibodies to thyroid peroxidase (AT-TPO)
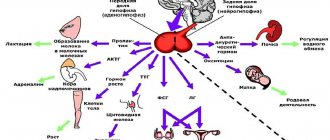
The thyroid gland and its hormones, together with the nervous and immune systems, take part in regulating the functioning of all human organs (heart, brain, kidneys, etc.). Unlike most hormones, which act only on certain cells of individual organs (for example, for estradiol these are the genitals), thyroid hormones are necessary for the normal functioning of all tissues and all organs without exception. Penetrating inside the cell, the hormone is sent to the nucleus, where it binds to certain areas on the chromosomes and activates a complex of reactions responsible for the processes of oxidation and reduction. Thyroid hormones are the main regulators of energy expenditure in the body, and maintaining their concentration at the required level is extremely important for the normal functioning of all organs and systems. For the synthesis of thyroid hormones, two essential components are required - iodine and the amino acid tyrosine. Without iodine, hormone synthesis stops completely, so it is extremely important to ensure that you get enough iodine from your diet. Tyrosine also enters the body with food; it is the basis not only for thyroid hormones, but also for adrenaline, melanin, and dopamine.
T3 and T4 .
The main two hormones produced by the thyroid gland are triiodothyronine and tetraiodothyronine (thyroxine). Triiodothyronine contains 3 molecules of iodine, and thyroxine contains 4 molecules. These hormones are abbreviated as T3 and T4, respectively. In the cells and tissues of our body, T4 gradually turns into T3, which is the main biologically active hormone that directly affects metabolism. However, thyroxine (T4) makes up about 90% of the total hormones secreted by the thyroid gland. Free T3 and T4 . Before entering the blood, thyroid hormones must be bound to transport globulin proteins (in order not to be “washed out” by the kidneys), but in order to enter the cell and tissue they must be freed from this “transport”. That. in the blood, T3 and T4 are found either in free or bound form. The level of free hormones is less than 0.1% of the total, but it is the free fraction of hormones that is the most biologically active, and it is they that provide all the effects of thyroid hormones.
Analysis of the level of the main hormones T3, T4 and their free variants is the first and most important step in determining the quality of the thyroid gland in case of any suspicion of its disease.
Thyroid-stimulating hormone (TSH) is the main regulator of thyroid function. Produced by the pituitary gland, a small gland located on the lower surface of the brain. TSH controls the production of thyroid hormones (thyroxine and triiodothyronine), which, in turn, regulate the processes of energy production in the body. The feedback mechanism allows you to maintain a stable level of these hormones - when their content in the blood decreases, the hypothalamus determines this fact and gives a signal to the pituitary gland to synthesize TSH. An increase in TSH concentration, in turn, stimulates the production of thyroid hormones by the thyroid gland. The reverse process occurs in a similar way. Dysfunction of the pituitary gland can cause an uncontrolled increase or decrease in the level of thyroid-stimulating hormone, thereby provoking the thyroid gland to produce thyroxine and triiodothyronine in abnormal quantities. An increase in their concentration causes hyperthyroidism, and a decrease, accordingly, causes hypothyroidism. Diseases of the hypothalamus, which regulates the secretion of TSH by the pituitary gland, can also cause disruptions in this system. In addition, diseases of the thyroid gland, accompanied by impaired production of thyroid hormones, can indirectly (via a feedback mechanism) affect the synthesis of thyroid-stimulating hormone, causing a decrease or increase in its concentration.
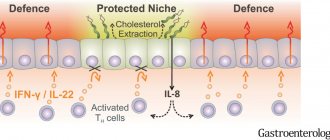
Antibodies to thyroglobulin (AT-TG) and to thyroid peroxidase (AT-TPO) In general, antibodies are proteins synthesized by cells of the immune system. Their main function is to identify and destroy foreign objects (bacteria, viruses, etc.). However, it happens that as a result of a malfunction, the body begins to produce antibodies against its own healthy tissues. In the thyroid gland, most often, the enzyme thyroid peroxidase (TPO) and the basis for hormone synthesis, thyroglobulin (TG), become objects for the production of antibodies.
Thyroglobulin is a preparation for thyroid hormones; thyroid cells “make” the hormones T3 and T4 from it. First, the cells produce thyroglobulin (thus creating iodine reserves), which is “stored for the future” in special containers - follicles. Then, as needed, T3 and T4 are synthesized from thyroglobulin.
Thyroid peroxidase is a thyroid enzyme involved in the formation of the active form of iodine and, thus, plays a key role in the production of thyroid hormones.
The damaging effect of antibodies can lead to disruption of the normal production of thyroid hormones and negatively affect the regulation of its function, which ultimately causes chronic pathologies associated with hypo- or hyperthyroidism. However, it is important to emphasize that antibodies to TPO and TG are not a key element in the pathogenesis of autoimmune diseases of the thyroid gland and begin to be produced in response to its damage. Therefore, attempts to reduce antibody levels are devoid of any practical meaning.
The AT-TG and AT-TPO tests are used to confirm or exclude the autoimmune nature of a particular thyroid disease (enlargement of the thyroid gland without impairing its function, primary hypo- or hyperthyroidism, ophthalmopathy, etc.), as this allows prescribing the most effective therapy . Tests are also prescribed to children born to mothers with pathology of the endocrine organs to determine risk groups for the development of thyroid diseases. Quantitative serum analysis for TPO-AT is the most sensitive method for diagnosing autoimmune thyroid diseases. AT-TG analysis is valuable in differential diagnosis.
Prices for tests can be found in the “Price List” section of the clinical laboratory. Blood for testing is accepted daily (except Sundays) from 7 to 11 am. Strictly on an empty stomach.
Read also about Adrenal Hormones and Sex Hormones
T3 hormone test
Testing for triiodothyronine is carried out for the following indications:
- routine annual physical examination;
- the patient’s initial visit to the endocrinologist due to increasing symptoms of a malfunction of the thyroid gland;
- pathologies of the thyroid gland;
- monitoring the treatment of thyroid disorders;
- pregnancy;
- collecting analysis of the newborn, especially in cases where the mother has problems with the thyroid gland.
A test for the T3 hormone is also prescribed for people:
- with diabetes mellitus;
- with adrenal insufficiency;
- with pernicious anemia;
- elderly;
- women after childbirth;
- having an inherited predisposition to thyroid pathologies.
What is free triiodothyronine (FT3)?
The thyroid gland is located in the neck, in which metabolic processes in the body are regulated through the production of free triiodothyronine (FT3) and thyroxine (FT4).
Free triiodothyronine is produced by the follicular cells of the thyroid gland under the control of thyroid-stimulating hormone. In peripheral tissues it is formed during the deiodination of free thyroxine (T4). Free triiodothyronine is the active part of total triiodothyronine. Triiodothyronine is more active than thyroxine, but is found in the blood in lower concentrations. Free form means that it is not bound to plasma proteins. The functions of free trioidthyronine also include:
- an increase in heat production and oxygen consumption by all tissues of the body, with the exception of the tissues of the brain, spleen and testicles;
- stimulation of vitamin A synthesis in the liver;
- reducing the concentration of cholesterol and triglycerides in the blood;
- acceleration of protein metabolism;
- increased urinary calcium excretion;
- activation of bone tissue turnover;
- having a positive chrono- and inotropic effect on the heart;
- stimulation of cortical processes in the central nervous system.
How to prepare for the analysis?
Some experts recommend taking a thyroid hormone test on an empty stomach, but there is another opinion - this is not required, as it does not change the level of hormones. However, it is not recommended to consume meat and other fatty foods before the study, as this affects the state of the blood serum, and it will be quite difficult for a specialist to isolate the formed elements in it.
In order for the T3 analysis result to be as reliable as possible, you need to:
- Do not eat fatty or meaty foods 24 hours before the test.
- Avoid stress, drinking alcohol and smoking.
- Tell your doctor about the medications you are taking. Some may have to be canceled for a while.
- Tell the doctor about your history of serious illnesses; some pathologies affect the results.
Important! It has been proven that a woman's use of contraceptive drugs affects the concentration of free T3, and according to the test results, the woman could be misdiagnosed with hyperthyroidism.
Norm of T3 hormone in women, men, children
The normal level of T3 hormone in women and men over 18 years of age is:
- general - 1.2–3.1 nmol/l,
- free - 3.1–6.8 pmol/l.
Normal levels of triiodothyronine in children are the same as in adults; they should be in the range of 3.1–6.8 pmol/l. But the level of other thyroid hormones depends on the age of the child.
Increased T3 hormone
If T3 is elevated, this means that the thyroid gland has malfunctioned. This may be iodine deficiency, thyroiditis, endemic goiter. Increased concentrations are dangerous due to catabolic disorders, loss of body weight, and deterioration in physical development.
Hormonal imbalance can lead to disruption of many systems at once:
- nervous;
- cardiovascular;
- urinary;
- reproductive;
- digestive;
- hepatobiliary;
- immune.
Elevated T3 is the basis for prescribing hormonal therapy, but only an endocrinologist can prescribe drugs.
Free triiodothyronine (free T3)
What is free triiodothyronine (Free T3, FT3)?
This is a thyroid hormone that stimulates the exchange and absorption of oxygen by tissues. It is produced by the follicular cells of the thyroid gland under the control of thyroid-stimulating hormone. In peripheral tissues it is formed during the deiodination of free thyroxine (T4). Free triiodothyronine is the active part of total triiodothyronine. Triiodothyronine is more active than thyroxine, but is found in the blood in lower concentrations.
Free trioidthyronine:
- increases heat production and oxygen consumption by all body tissues, with the exception of brain tissue, spleen and testicles;
- stimulates the synthesis of vitamin A in the liver;
- reduces the concentration of cholesterol and triglycerides in the blood;
- accelerates protein metabolism;
- increases calcium excretion in urine;
- activates bone tissue turnover (to a greater extent, bone resorption);
- has a positive chrono- and inotropic effect on the heart;
- stimulates reticular formation and cortical processes in the central nervous system.
The level of free triiodothyronine depends on:
- from age (by 11 - 15 years, the concentration of free triiodothyronine reaches the level of adults; over 65 years of age, a decrease in free triiodothyronine in serum and plasma is observed);
- during pregnancy, the value of free trioidthyronine decreases from the 1st to the 3rd trimester; a week after birth, serum free trioidthyronine levels return to normal;
- by gender (women have lower concentrations of free trioidthyronine than men);
- depending on the time of year (the maximum level of free trioidthyronine occurs from September to February, the minimum - in the summer).
Indications for the purpose of analysis:
- differential diagnosis of thyroid diseases;
- control study for isolated T3 toxicosis.
When is the free triiodothyronine level elevated?
- Thyrotropinoma.
- Toxic goiter.
- Isolated T3 toxicosis.
- Thyroiditis.
- Thyrotoxic adenoma.
- T4-resistant hypothyroidism.
- Thyroid hormone resistance syndrome.
- TSH-independent thyrotoxicosis.
- Postpartum thyroid dysfunction.
- Choriocarcinoma.
- Decreased levels of thyroxine-binding globulin.
- Myelomas with high levels of IgG.
- Nephrotic syndrome.
- Hemodialysis.
- Chronic liver diseases.
When is the free triiodothyronine level low?
- Uncompensated primary adrenal insufficiency.
- Severe nonthyroidal pathology, including somatic and mental illnesses; period of recovery after serious illness.
- Primary, secondary, tertiary hypothyroidism.
- Artificial thyrotoxicosis due to self-prescription of T4.
- Low protein and low calorie diet.
- Heavy physical activity in women.
- Loss of body weight.
- Taking amiodarone, large doses of propranolol, x-ray iodine contrast agents.
Detailed description of the study
Normally, the thyroid gland, under the influence of the pituitary thyroid-stimulating hormone (TSH), synthesizes two hormones that affect the metabolism of the entire body: T3 (triiodothyronine) and T4 (thyroxine). The difference between them is that the first hormone contains three iodine molecules, and the second - four.
The biological activity of T3 is 3-4 times higher than T4. Both hormones enter the blood and circulate in it independently (free fraction) or by combining with blood plasma proteins. This study reveals the concentration of total T3 in the blood.
Total T3 is the total indicator of hormone fractions bound and unbound to plasma proteins in the blood. Most bound T3 is transported by albumins, prealbumins, and to a lesser extent by a special protein, thyroxine-binding globulin. Unbound (free) T3 molecules have greater biological activity than bound fractions.
The main functions of the T3 hormone include:
- Regulation of protein, fat and carbohydrate metabolism;
- Supports the physiological functioning of the heart (heart rate, blood pressure);
- Regulation of energy metabolism (acceleration of basal metabolism, maintaining body temperature);
- Participation in growth and development, especially in children: T3 accelerates growth, promotes the development of cognitive functions.
The physiological level of the hormones T3 and T4 (together with TSH) ensure optimal functioning of the thyroid gland - this condition is called “euthyroidism”. Disruption of the thyroid gland is accompanied by an increase (hyperthyroidism) or a decrease, and sometimes a complete loss of its function (hypothyroidism). Hypothyroidism and hyperthyroidism are nonspecific syndromes and can occur against the background of various diseases of the thyroid gland and the hypothalamic-pituitary system.
Symptoms of hypothyroidism may include:
- General weakness, drowsiness;
- Constipation (constipation);
- Slow heart rate (bradycardia);
- swelling of the face, limbs or trunk;
- Sensation of a “foreign body” in the neck due to an increase in the volume of the thyroid gland;
- Difficulty breathing and/or swallowing due to an increase in the volume of the thyroid gland;
- Delayed mental and physical development in children and sexual development in adolescents.
Signs of hyperthyroidism include:
- Headache;
- Anxiety, nervousness;
- Increased sweating;
- Rapid heart rate (tachycardia);
- High fatigue;
- Diarrhea;
- Sleep and eating disorders.
Determining the concentration of T3 in the blood, especially together with identifying the levels of T4 and TSH, makes it possible to establish a dysfunction of the thyroid gland and begin timely treatment.
What is the purpose of measuring free triiodothyronine (FT3)?
Indications for the analysis are differential diagnosis of thyroid diseases and control testing for isolated T3 toxicosis. This test accurately measures FT3 levels in the body and therefore can help in assessing thyroid function. This test is often prescribed in combination with a TSH and T4 (thyroxine) test. As a rule, tests are carried out as planned if the doctor suspects problems with the thyroid gland. Such potential problems may include:
- Hyperthyroidism (hyperfunction of the thyroid gland);
- Primary or secondary hypothyroidism (decreased thyroid function);
- Hypopituitarism (decreased activity of the pituitary gland);
- Thyrotoxic periodic paralysis (high levels of thyroid hormones).
The thyroid gland produces hormones that affect almost all body functions. Thus, thyroid disease can cause a wide range of symptoms such as weakness and fatigue, anxiety, constipation, weight loss, insomnia, menstrual irregularities and increased heart rate. In addition, the FT3 test is re-ordered after initial tests that show TSH results above or below normal.
It is important to understand that thyroid research is a look at what is happening in the human body. Trioidthyronine levels depend on:
- from age (by 11 - 15 years, the concentration of free triiodothyronine reaches the level of adults; over 65 years of age, a decrease in free triiodothyronine in serum and plasma is observed);
- during pregnancy, the value of free trioidthyronine decreases from the 1st to the 3rd trimester; a week after birth, serum free trioidthyronine levels return to normal;
- by gender (women have lower concentrations of free trioidthyronine than men);
- depending on the time of year (the maximum level of free trioidthyronine occurs from September to February, the minimum - in the summer).
In addition, test results may also be affected by certain medications, such as estrogen, birth control pills, and high-dose aspirin.
References
- Hypothyroidism. Clinical recommendations. Association of Endocrinologists of Russia, 2022. - 38 p.
- Federal clinical guidelines for the diagnosis and treatment of thyrotoxicosis with diffuse goiter (diffuse toxic goiter, Graves-Bazedow disease), nodular/multinodular goiter, 2014. - 45 p.
- Encyclopedia of clinical laboratory tests / ed. WELL. Titsa. - M.: Labinform, 1997. - P. 461-465.
- Kumar, V., Abbas, A., Fausto, N. et al. Robbins and Cotran Pathologic Basis of Disease, 2014. - 1464 p.