LOSARTAN (tablets)
Bisoprolol is also used for increased heart rate.
When I came to prescribe free medications in May of this year, Lorista was not available in pharmacies. I bought it in cash for two months. In July there was no Lorista or Amlodipine again. That's why they prescribed me this drug. Pranafarm Losartan tablets are an antihypertensive drug. Now I take it twice a day, one tablet in the morning and in the evening. And as an ambulance, just in case, I always have drugs such as Capoten or Captopril. Losartan tablets are sold in red and white cardboard packaging, which contains the minimum necessary information, such as a description of the tablets. Of course, it should be used only as prescribed by a doctor. There is a warning about the lactose content in the drug, because some people are intolerant. And of course there are storage conditions.
The active component of this medication is potassium salt. The manufacturer's details are also indicated on the packaging.
The release date, expiration date and series are embossed on the side.
The package contains three foil blisters of 10 tablets each. I have already started taking the second package.
On the reverse side is the name and description of the drug.
The tablets themselves are white, round in shape with a scoring line.
The instructions for use included in the package are quite extensive, so I’ll highlight only the most important things.
I also draw your attention to contraindications.
And a whole bunch of side effects are described (the photo may be deleted by the moderators). If you make a list of contraindications, you get 78 points.
The medicine can be taken both before and AFTER meals, that is, regardless of the time of meal. If necessary, you can gradually increase the dose. BUT!!! it should not exceed 100 milligrams per day. It turns out that I was immediately prescribed the maximum. For people with chronic heart failure, the standard maintenance dose of this drug is 50 milligrams, taken once a day. I accept the second package. The pressure remains even slightly lower. You probably need to reduce the dose. I don't really feel any side effects. Yes, there is drowsiness, but I have the opportunity to lie down with my grandson during the day)) Of course, I notice tachycardia and increased heart rate. I had pain in my lower extremities and back before. In general, of course, we all know that no medicine is 100% useful. As they say, “We treat one thing, we cripple another.” Nevertheless, you need to take it. I recommend, but with caution and only as prescribed by your doctor. The cost of the drug in our pharmacies is around 300 rubles. I will give the drug four stars, as there are a lot of side effects indicated. Health to everyone and once again health!!! Thanks for reading. With respect to you, the author of this review, Tatyana. See you again on the site!!!
Side effects and consequences
To reduce the risk of side effects, you should stop drinking alcohol during the period of treatment and carefully follow the warnings of doctors and the manufacturer (instructions for the drug).
Losartan should not be taken if there are contraindications:
- Allergy to the components of the drug.
- Individual intolerance to the active substance or auxiliary components.
- Low blood pressure (blood pressure may drop too much).
- Chronic gastritis.
- Acute form of heart failure.
- Children's age up to 18 children.
- Dehydrated state of the body (including from exposure to alcohol).
- During pregnancy and breastfeeding.
The drug has a relatively low likelihood of side effects. Symptoms are relatively mild, so symptomatic therapy or discontinuation/adjustment of the dosage of the drug is usually not required. The most dangerous symptoms occur in case of drug overdose: a sharp and severe decrease in blood pressure, bachycardia and brachycardia (decrease in heart rate to 30-40 beats per minute).
In rare cases (less than 1% of patients), the following side effects are possible:
- Feeling of dry mouth, nausea and vomiting.
- Functional gastrointestinal disorders (diarrhea or diarrhea).
- Deterioration of potency, disruption of the normal functioning of the liver and kidneys.
- Upper respiratory tract infections, bronchitis and rhenitis with symptoms corresponding to the disease.
- Pain in the back, shoulders and lower extremities; exacerbation of arthritis.
- Increased sweating.
- Increased fatigue, chronic fatigue syndrome, sleep disorders.
- Headaches and dizziness.
All these side effects, with some probability, can also occur in a person who fully complies with the recommendations of doctors and does not drink alcohol. Drinking alcohol causes a serious blow to health and increases the likelihood of negative consequences.
Consequences of combining Losartan tablets with alcohol:
- A sharp decrease in pressure. Alcohol dilates blood vessels, thereby causing a decrease in blood pressure for some time. If you have blood pressure-lowering drugs in your body, your blood pressure may drop too much and your heart rate may slow down dangerously.
- A double blow to the gastrointestinal tract and organs. The liver, kidneys and gastrointestinal tract react negatively to both alcohol and most medications. Alcohol abuse puts a strain on the kidneys and liver, increasing the likelihood of side effects and pathological processes.
- Symptoms of incompatibility. Symptoms can appear suddenly after drinking even a small amount of alcohol: nausea, dizziness, sudden weakness, cold extremities, loss of coordination and orientation in space.
To avoid negative consequences, do not combine alcohol with medications, spacing out taking pills and alcohol as much as possible over time. It is advisable to consult a doctor regarding the possibility of drinking alcohol for health reasons. It should be remembered that other medications taken may be incompatible with alcohol and may also change the effect of other medications.
Compound
| Film-coated tablets | 1 table |
| active substance: | |
| losartan potassium | 50 mg |
| 100 mg | |
| excipients: colloidal silicon dioxide - 0.75/1.5 mg; magnesium stearate - 1.5/3 mg; croscarmellose sodium - 3/6 mg; pregelatinized starch - 20.2/40.4 mg; MCC - 74.55/149.1 mg | |
| film shell: Opadry 33G28523 white (triacetin - 0.3/0.6 mg, macrogol - 0.4/0.8 mg, lactose monohydrate - 1.05/2.1 mg, titanium dioxide (E171 - CI77891) - 1 .25/2.5 mg, hypromellose - 2/4 mg) - 5/10 mg |
The second class of drugs is angiotensin II receptor blockers.
Research that has focused on studying the possibilities of blocking the RAAS has led to the discovery of a group of drugs that do not have the classic disadvantage of ACE inhibitors - the side effect of cough. ARBs, or sartans, block the RAAS more completely, resulting in better tolerability than their predecessors. Despite their relatively recent introduction into clinical practice - sartans began to be used for long-term treatment of hypertension only in 1999 - representatives of this group have today become one of the most popular antihypertensive drugs [12].
Sartans: mechanism of action and effect
The pharmacological effect of sartans is identical to the effect of ACE inhibitors. Due to competitive blockade of angiotensin II receptors, they suppress vasoconstriction, aldosterone secretion, reduce myocardial hypertrophy, and also improve endothelial function.
The mechanism of action of ARBs is not the blockade of angiotensin-converting enzyme, as is the case with ACE inhibitors, but the blockade of angiotensin AT1 receptors, through which the vast majority of the physiological effects of angiotensin II are realized (vasoconstriction, etc.). AT1 receptors are located predominantly in vascular smooth muscle, heart, liver, adrenal cortex, kidneys, lungs and brain.
Over the past 10 years, drugs have appeared that some experts propose to separate into a separate, second generation of ARBs. They not only block AT1 receptors, but also help normalize carbohydrate and lipid metabolism.
Indications and properties
Sartans, like ACE inhibitors, are prescribed for a number of diseases, including arterial hypertension, chronic heart failure, previous myocardial infarction, diabetic nephropathy, atrial fibrillation and metabolic syndrome. In addition, ARBs become the drugs of choice in situations where cough develops while taking ACE inhibitors [13].
The effectiveness of sartans has been proven to significantly reduce blood pressure and have a cardioprotective effect [13, 14], as well as:
- reduce the incidence of myocardial infarction and stroke;
- reduce the frequency of hospitalizations due to chronic heart failure;
- reduce the severity of symptoms of CHF;
In addition, some ARBs, like ACEIs, reduce the likelihood of developing diabetes and exhibit nephroprotective effects.
The first class of drugs is ACE inhibitors.
Drugs of this group became one of the first classes of drugs that effectively reduce the activity of the RAAS; their development began in the 60s of the last century [2]. Today they are included in the category of so-called “life-saving drugs” due to their proven ability to improve the prognosis of a number of cardiovascular and renal diseases [2].
ACE inhibitors: mechanism of action and effect
ACE inhibitors reduce the level of circulating angiotensin II by blocking the angiotensin-converting enzyme, which causes a complex pharmacological effect:
- antihypertensive;
- cardioprotective;
- angioprotective;
- antiatherosclerotic;
- anti-inflammatory.
When taking drugs from the ACE inhibitor group, carbohydrate metabolism also improves: tissue sensitivity to insulin increases and glucose metabolism improves.
Indications and properties
The spectrum of activity of ACE inhibitors allows their use in arterial hypertension, coronary heart disease, chronic heart failure, nephropathies and acute myocardial infarction [3].
ACE inhibitors belong to the group of antihypertensive drugs that specifically lower blood pressure and slow the progression of heart failure, which determines their widespread use in cardiology. Data from a review of 158,998 patients with hypertension showed that taking ACE inhibitors reduces mortality from all of the above causes. This is a significant advantage of ACE inhibitor drugs, including compared to angiotensin II blockers [4].
However, ACE inhibitors are still not able to completely prevent the conversion of angiotensin I to angiotensin II, since there are a number of other enzymes that successfully “replace” ACE. This is exactly how the enzymes chymase, elastase and cathepsin G work, for example [5]. When using ACE inhibitors, these substances are compensatory activated, and the blockade of the RAAS becomes incomplete. This is a significant drawback of ACE inhibitors.
What should I warn the client about?
Important!
During the consultation, it is appropriate to emphasize that drugs that block the activity of the RAAS - ACEIs and ARBs - with constant use, along with an antihypertensive effect, protect the heart and blood vessels, significantly reducing the incidence of cardiovascular accidents. This small note can serve as a convincing argument in favor of regular and disciplined use of such drugs, according to the instructions and recommendations of the doctor.
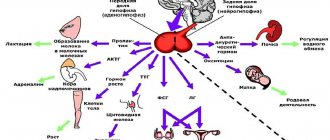
RAAS: the basics
Before we begin describing the drugs, let’s dive briefly into the intricacies of pharmacology and once again remember what the mechanism of action of the renin-angiotensin-aldosterone system, or RAAS, is.
The RAAS is a complex hormonal-enzymatic system in which almost all organs and tissues of the body are involved, but the key roles in it belong to the liver, kidneys, adrenal glands and lungs.
Alpha-2‑globulin angiotensinogen is constantly synthesized in the liver. At the same time, the kidneys produce the enzyme renin in response to decreased intrarenal pressure, decreased delivery of sodium and chloride, and hypoxia. It enters, like angiotensinogen, into the systemic circulation, where it binds to it to form angiotensin I.
Angiotensin I is a practically inert substance. It does not act on blood vessels and is only a precursor of the active component angiotensin II. In the formation of the latter, along with angiotensin I, angiotensin-converting enzyme (ACE), which is produced in the lungs, is involved.
Angiotensin II is the main link in the RAAS circuit.
It exhibits a powerful vasoconstrictor effect and affects the target organs in which its receptors are located. First of all, we are talking about the endothelium, heart and kidneys. This is why high levels of angiotensin II are associated not only with increased blood pressure, but also with damage to the vascular wall, myocardium, kidneys, and the development of chronic heart and kidney failure.
In addition, angiotensin II causes increased synthesis of the adrenal hormone aldosterone. The latter is involved in the control of blood pressure (BP) by regulating the homeostasis of potassium, sodium and intracellular fluid volume. Under its influence, blood pressure increases and the sensitivity of vascular smooth muscles to vasoconstrictor substances, including angiotensin II, increases.
Thus, the RAAS is directly involved in the drama called “arterial hypertension”, playing one of the main roles in it. Fortunately, it is possible to block this system. This can be done with drugs of two pharmacological groups - angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs, also known as sartans).
Tolerability of ACE inhibitors
The subject of special attention of pervostolniks, as specialists dispensing the drug, is the side effects of ACE inhibitors. Despite the generally favorable safety profile, adverse reactions are the weak link of drugs in this group.
What should I warn the client about?
- While taking ACE inhibitors, a dry cough develops in 1–10% of cases [6]. Different members of the group practically do not differ from each other in their ability to cause it, and replacing one ACE inhibitor with another does not improve tolerability in this regard [11].
- When taking single-agent ACEIs, Quincke's edema can extremely rarely occur (but more often than when taking other antihypertensive drugs) [2]. It is believed that drugs in this group do not cause this complication, but alleviate its occurrence in predisposed patients. When releasing ACE inhibitors, it is appropriate to emphasize that if difficulty breathing and shortness of breath occur, you should immediately contact your doctor [11].
The cause of cough while taking ACE inhibitors has not been fully determined. It is assumed that the leading role is played by the accumulation of bradykinin in the bronchial mucosa, which is activated by blockade of angiotensin II [11].






![Table 1. Bioavailability (absorption) of various organic forms of calcium within 2 hours after oral administration in the experiment [22]](https://laram-halal.ru/wp-content/uploads/tablica-1-biousvoyaemost-absorbciya-razlichnyh-organicheskih-form-kalciya-v-techenie-330x140.jpg)
