Anal fissure is one of the most common proctological problems associated with a violation of the integrity of the structure of the anal mucosa. The tissue rupture, which mainly forms on the back wall of the anus, can have different lengths and depths, but usually its length reaches 1-2 cm. Over time, the crack changes: granulation, “tubercles” form at the edges, which can later turn into a fibrous polyp . This pathology is encountered by people aged 20-60 years, but in females this disease is diagnosed much more often.
Causes
There are a number of factors that contribute to the appearance of anal fissures. These include:
- Constipation. Constant defecation of hard feces is fraught with the appearance of microcracks and damage to the anal tissues. When a person pushes, pressure increases in the anus, which can result in tissue rupture and cracks.
- Proctitis (inflammation of the mucous membrane). Inflammatory processes make the mucous membrane less durable and, therefore, more vulnerable to injury from feces.
- Childbirth. The mucous membrane can crack as a result of too active pushing, the use of vacuum and other manipulations.
- Poor nutrition. If food (nuts, seeds, etc.) is poorly chewed, then it may not be completely digested in the future. As a result, remaining sharp pieces of food can damage the mucous membrane during bowel movements.
- Increased power loads;
- Sedentary work;
- Examination of the intestines through the anus;
- Anal sex;
- An unbalanced diet - excessive consumption of spicy foods and alcohol.
Symptoms and clinical course of the disease
An acute anal fissure appears suddenly after exposure to one or more unfavorable factors (exacerbation of hemorrhoids, prolonged diarrhea or constipation, dietary errors, alcohol abuse). The disease makes itself felt by acute pain, which intensifies during bowel movements.
The pain is accompanied by the appearance of fresh blood on stool, toilet paper or underwear, but significant bleeding is rare.
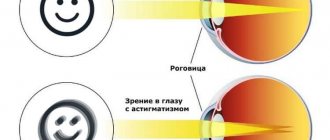
Acute pain causes a reflex spasm of the muscles of the internal anal sphincter, which disrupts the blood supply to the tissues and complicates the independent healing of the mucosal defect.
With a long course of the pathology (4 weeks or more), the edges of the crack thicken, so that healing becomes impossible even when the spasmodic internal sphincter relaxes. The disease takes a chronic course and can last for the rest of your life.
Complications
Every time you defecate, the wound comes into contact with feces, which contain a huge amount of bacteria. Pathogenic microorganisms settled on the crack aggravate inflammatory processes.
If left untreated, the consequences can be very different:
- Bleeding, which may cause anemia;
- The chronic form is a predisposing factor to the formation of tumors;
- Infection of the wound is fraught with the development of paraproctitis or sepsis;
- A prolonged inflammatory process is dangerous due to the formation of fistulas.
Surgical methods
The main goal of surgery for anal fissure is to create conditions for successful self-healing of the wound defect. In chronic pathology, healing is hampered by rough edges and deposits (granulation) at the bottom of the wound. Therefore, the edges of the crack are excised and granulations are removed, transforming the old wound into a fresh one.
In 30% of cases this is enough to get rid of the disease. The use of laser surgery allows operations to be performed on an outpatient basis, without placing the patient in a hospital.
However, most patients develop persistent spasm of the internal sphincter, which impairs blood supply to injured tissues and prevents wound healing. Therefore, the classic method of surgery for anal fissure is a combination of excision of the fissure with sphincterotomy (partial dissection of the internal sphincter).
Diagnostics
The presence of an anal fissure can be determined during a visual examination - the doctor can easily identify swelling and disorders of the mucous membrane. A finger examination allows you to determine the crack located inside by determining its size and feeling the edges.
Diagnostic methods
- Sigmoidoscopy - allows you to assess the condition of the rectum at a distance of 20-25 cm from the anus. During the procedure, tissue can be excised for histology, identified tumors can be removed, and medication can be administered;
- Anoscopy is an informative technique that allows you to examine the anal canal at a distance of 10-12 cm. Using an anoscope you can detect polyps, inflammatory processes, bleeding and other pathological changes;
- Laboratory tests - the patient is sent for a general clinical analysis of blood, feces and urine, culture for flora, etc.;
- Taking an anamnesis allows you to exclude other possible diseases.
Diagnosis and choice of treatment tactics
The diagnosis of anal fissure is established during the initial examination by a proctologist. For long and deep cracks, doctors prescribe anoscopy.
During the examination, indications for surgery are revealed: • rough edges of the crack; • symptoms of prolonged sustained spasm of the internal sphincter; • presence of hemorrhoids requiring surgical intervention.
If surgery is to be performed, the doctor will prescribe a standard list of diagnostic procedures (general blood test, coagulogram, ECG, laboratory tests for infectious diseases transmitted through blood (hepatitis, HIV, etc.), consultation with a therapist, fluorography of the chest organs, and for women also receive a report from a gynecologist).
Treatment
Treatment of acute anal fissure
In this case, conservative treatment methods are used, involving the use of special ointments, suppositories, and laxatives. Drug therapy is aimed at:
- Anesthesia;
- Relieving anal spasms;
- Normalization of stool;
- Healing of the wound (crack).
If conservative treatment does not achieve the desired effects, then minimally invasive methods can be used.
Treatment of chronic anal fissure
If the disease has become chronic, then most likely, surgical intervention will be required - removal of granulation and cutting off the tubercles. Further treatment continues using conservative methods.
Treatment methods:
- Radiosurgery – targeted removal of damaged tissue using the Surgitron radio wave apparatus;
- Pararectal blockade - injection of an anesthetic with a syringe and further divulsion - expansion of the anal sphincter to relieve spasms.
Preparing for surgery
3 days before surgery, you should avoid foods that stimulate gas formation in the intestines. The ban includes black bread, legumes, cabbage, fresh vegetables and fruits, juices, mineral water, and alcoholic drinks.
A day before excision of the anal fissure, they switch to easily digestible food (“chocolate” diet). 12 hours before surgery. If you smoke, it is advisable to also give up cigarettes on the day of surgery.
During preparation for surgery, a protective regime is followed. It is necessary to exclude physical and nervous stress, do not drink alcohol, as well as tonic drinks, including coffee.
The evening before surgery, the intestines are cleansed using enemas or laxatives.
General recommendations
After defecation, you should treat the anus and the area around the anus with cold water - this will help reduce pain and prepare the anus for the use of topical medications.
To facilitate the act of defecation, it is recommended to use enemas. The procedure is performed when there is a urge to defecate.
- Oil enema. To prepare the solution, you need to measure 150 ml of water and add 50 ml of oil;
- Water enema. In this case, boiled water is used, preferably with the addition of disinfectants.
How is the operation performed?
Surgery for anal fissure takes 15-30 minutes. If intravenous anesthesia is used to control pain, the patient falls asleep before the operation and wakes up in the recovery room. If doctors prescribe epidural anesthesia or local anesthesia, the patient is conscious, but does not feel pain. When choosing an anesthesia method, both medical indications and the wishes of the patient are taken into account.
The surgery is performed using equipment that resembles a gynecological chair. Today in Moscow and other cities of Russia, surgeons prefer to replace the traditional scalpel with the latest methods: • electrocoagulation; • radio wave surgery (Surgitron device); • laser surgery.
These methods allow the operation to be performed bloodlessly, since the miracle knives simultaneously seal the vessels. In addition, when using modern technologies, tissue is less damaged, and the healing process is much faster. The choice of method is made by the doctor, taking into account medical indications (size and location of the crack, accompanying changes in tissue, etc.).
Symptoms
The manifestation of a chronic anal fissure is a triad of symptoms: pain, sphincter spasm and bleeding from the rectum during bowel movements. In some patients they are reduced. In typical cases, acute burning pain in the perineum occurs at the time of defecation and lasts from several minutes to several hours. In some patients, fear of pain transforms into fear of stool. In this case, stool retention and defecation of dense, lumpy feces occurs. For this reason, the next emptying of the rectum becomes very painful. Other patients have a higher threshold for pain sensitivity, and they do not subjectively experience pain as catastrophically.
Muco-bloody discharge from the rectum with a non-healing anal fissure is scanty. Obvious rectal bleeding occurs only in the presence of concomitant hemorrhoids. To identify sphincter spasms, proctologists at the Yusupov Hospital conduct a rectal examination. To do this, carefully, using your thumbs, the doctor gradually spreads the buttocks apart. The anal canal opens and on one of the walls the outer part of a linear or triangular fissure and the sentinel tubercle become visible.
Since digital examination for chronic anal fissure is very painful, doctors at the proctology department perform it after preliminary local anesthesia with gel, spray with local anesthetics, and injections with lidocaine. When palpated, the doctor usually reveals a dense, painful formation that is located along the axis of the intestine. Sometimes the anal canal is rigidly narrowed due to the development of pectenosis (scar narrowing).
Rules of conduct after surgery
After anal fissure surgery, patients are discharged from the hospital on the fifth day. It will take 2-3 weeks for the wound to heal completely. In order for surgery to result in successful restoration of health, it is necessary to strictly adhere to the rules. 1. Stool should be daily, preferably in the morning. 2. If it is not possible to achieve regular bowel movements with the help of a diet, mild laxatives are allowed - as prescribed by a doctor. 3. Toilet paper is replaced by washing. 4. Spicy, salty, smoked foods, fruits with small seeds, and alcohol are prohibited. 5. It is necessary to refrain from heavy physical exertion, as well as from prolonged sitting, visiting the bathhouse, sauna.
If the operation was performed on an outpatient basis, in the first days after surgery it is necessary to care for the wound (daily dressings and warm baths with potassium permanganate), relieve pain using recommended painkillers and strictly follow all the instructions of the attending physician.
What is required for differential diagnosis of this disease?
A fissure can occur with inflammatory diseases of the colon, such as Crohn's disease or ulcerative colitis. Infectious diseases (syphilis, HIV, herpetic infection, etc.) can also contribute to the development of anal fissure. Tumor diseases such as cancer, melanoma, leukemia can manifest themselves in the same way as an anal fissure. The patient will experience pain in the anus and bleeding from the anus.
Rice. 8. Cancer of the anal canal with transition to the perianal skin
How to avoid relapse: patient reviews and doctors’ recommendations
As an analysis of reviews published on the Internet shows, most patients tolerate anal fissure excision surgery relatively easily and are happy to be free of the disease.
However, in order to avoid such surgical interventions in the future, it is necessary to adhere to the rules of prevention: • timely treatment of diseases of the digestive system; • ensuring regular bowel movements; • combating physical inactivity (hiking, swimming, etc.).
The fact is that an anal fissure occurs as a result of the influence of causative factors (diseases of the gastrointestinal tract, irregular bowel movements, a “sedentary” lifestyle leading to congestion of the pelvic organs, etc.). If the causes of the pathology are not eliminated, the disease may return at any time.
Early rehabilitation after surgery
Regardless of the chosen method of operation and anesthesia technique, after surgery, a tampon soaked in medicinal ointments is installed in the anus.
Then, throughout the early postoperative period (the first 2-3 days), dressings are performed daily. Gauze bandages soaked in levomekol ointment are applied to the anus.
Inpatients are advised to begin getting out of bed and walking the day after surgery. A slag-free diet is also prescribed (if there are no contraindications, a “chocolate” diet). The purpose of such a diet is to delay bowel movements for better wound healing.
From the third day, the diet expands, foods containing dietary fiber that stimulate bowel movements are prescribed. If on the third day it is not possible to achieve independent stool, a cleansing enema is used.
Anal fissure (anal fissure)
Anal fissure
(
anal fissure
) is a defect in the mucous membrane of the anal canal, located on the wall of the rectum in the area of transition of the anoderm into the mucous membrane of the anal canal. Anal fissure is characterized by the following symptoms:
- pain during bowel movements
- spasm of the internal anal sphincter
- bloody discharge from the anus
There are:
- acute anal fissure
- chronic anal fissure
Based on the location of the crack, the following are distinguished:
- posterior anal fissure
- anterior anal fissure
- lateral anal fissure
Based on the presence of sphincter spasm, the following are distinguished:
- with sphincter spasm
- without sphincter spasm
Acute anal fissure
The main complaint of patients with anal fissure is the pain that occurs during defecation, which is usually very strong and can last for a long time. Because of these pains, patients often delay bowel movements, which can lead to the development of constipation. The pain causes a spasm of the anal sphincter, which, starting during defecation, can last for a long time, up to several days, until the next act of defecation. Thus, pain can cause sphincter spasm; spasm increases pain and prevents the healing of the anal fissure. Constant injury to the mucous membrane by stool is accompanied by slight bleeding from the anus. Acute anal fissures most often (in 90% of patients) heal spontaneously or with therapy, most often within 6–8 weeks. However, in some patients this does not happen, which leads to the formation of a chronic anal fissure.
Chronic anal fissure
Chronic anal fissure occurs in 2-2.5% of the adult population, occupying third place among proctological diseases after hemorrhoids and paraproctitis.
The existence of a defect (crack) for a long period of time, as a rule, is accompanied by the appearance of distinctive morphological features: the presence of muscle fibers of the internal sphincter of the anus at the bottom of the defect, its dense “callous” edges, the proliferation of granulations in the form of a fibrous compaction “sentinel tubercle” at the distal end of the crack , compaction of the apex of the anal papilla at its proximal end (Krylov N.N.). The microbial landscape of chronic anal fissure is represented by associations of aerobic and anaerobic microorganisms. The anaerobic microflora is dominated by representatives of the genus Bacteroides
.
Among the representatives of aerobic microflora, gram-negative rods (most often E. coli
) and gram-positive cocci (
Enterococcus spp.
), sensitive to fluoroquinolones (ciprofloxacin), aminoglycosides (gentamicin) and cephalosporins (ceftriaxone, cefuroxime) were identified (Maleeva E.A.).
Treatment of anal fissure
Treatment of anal fissure can be therapeutic (conservative) and surgical.
Conservative includes diet *), drug treatment to normalize stool, suppositories, ointments, warm sitz baths. Conservative treatment of acute anal fissure
includes warm sitz baths and laxatives containing psyllium - the shells of plantain seeds: "Mukofalk", "Metamucil" or "Fiberlex", can reduce pain, stop bleeding and heal in half of those suffering from acute anal fissure with minimal risk of side effects. Adding local anesthetics and anti-inflammatory drugs to the treatment regimen does not affect its results. Such treatment of acute anal fissure is contraindicated in the following cases:
- erosive and ulcerative lesions of the upper gastrointestinal tract, which requires limiting the intake of fiber contained in psyllium
- intestinal obstructions
- malignant neoplasms in the pelvic area.
Conservative treatment of chronic anal fissure
should include medications to relax the internal anal sphincter. For this, organic nitrates are used, in particular nitroglycerin ointment 0.4%, which is prepared by mixing a concentrated oily solution of nitroglycerin and petroleum jelly.
0.5 ml of nitroglycerin ointment is applied 2 times a day to the perianal skin and inserted with a finger into the anal canal to a depth of 1 cm. For accurate dosing, use a ruler on which a column of ointment is applied (if it is packaged in tubes), or use a syringe.
The use of 0.4% nitroglycerin ointment allows for recovery in half of those suffering from chronic anal fissure. However, its use only slightly increases the rate of healing of anal fissure, significantly speeding up only the time of disappearance or reduction of pain. The number of relapses of anal fissure after treatment with 0.4% nitroglycerin ointment is significantly higher than the number of relapses after surgical treatment, although the frequency of complications is much lower. The main side effect of nitroglycerin ointment is headache, which occurs in 20-30% of patients.
If side effects occur that prevent treatment with organic nitrates, it is possible to use calcium channel blockers such as diltiazem or nifedipine (Clinical guidelines of the Association of Coloproctologists of Russia).
During surgical treatment
Excision of the anal fissure is performed in combination with sphincterotomy or without it. The need for sphincterotomy is determined using anorectal manometry (Groshilin V.S.).
Patient Materials
- Demin A.A. Anal fissure / www.GastroScan.ru, 2022
The website GastroScan.ru contains materials for patients on various aspects of gastroenterology and coloproctology:
- “Advice from doctors” in the “Patients” section of the site
- “Popular gastroenterology” in the “Literature” section
- “Popular gastroenterology” in the “Video” section
Note. *) The diet corresponds to the diet for constipation, see “Constipation”, “Diet for children with constipation”.
Resources for healthcare professionals regarding the diagnosis and treatment of anal fissures
Printed materials
- Krylov N.N. Chronic anal fissure. // Bulletin of surgical gastroenterology. - 2008, - No. 1, - p. 5-11.
- Groshilin BC The importance of anorectal manometry in the choice of tactics for surgical treatment of anal fissures // RZHGGK. - 2010. - T.20. - No. 5. - Adj. No. 36. - P.50.
- Clinical recommendations for the diagnosis and treatment of adult patients with anal fissure // Association of Coloproctologists of Russia. Moscow. 2013 17 p.
- Clinical recommendations. Coloproctology. Anal fissure / ed. Yu.A. Shelygina. M.: GEOTAR-Media, 2015. pp. 12-29.
- Maleva E.A. Microecological status of chronic anal fissure and its impact on the choice of treatment method. Abstract of dissertation. PhD, 01/14/17 – surgery, 02/03/03 – microbiology. South Ural State Medical University, Chelyabinsk, 2014.
- Lyukhurov R.N. Surgical tactics for chronic hemorrhoids stage III-IV in combination with anal fissure. Abstract of dissertation. PhD, 01/14/17 – surgery. KRSU, Bishkek, 2016.
- Rogozhkina E.A. Differentiated pathogenetic approach to the treatment of chronic anal fissures. Abstract of dissertation. PhD, 01/14/17 – surgery. RostSMU, Rostov-on-Don, 2022.
- Adiev R.F. Surgical tactics and complex treatment of patients with chronic anal fissure. Abstract of dissertation. PhD, 01/14/17 – surgery. BSMU, Ufa, 2013.
- Achkasov E.E., Solomka A.Ya., Ulyanov A.A., Gribanov I.I. A new method of combined treatment of chronic anal fissure // Modern theory and practice. Surgery: materials X All-Russian. conf. general surgeons with international uch. and conf. young scientists-surgeons. Ryazan. 2018. pp. 154–155.
- Belik B.M., Kovalev A.N., Khatlamadzhiyan A.L. The use of PRP therapy in the complex treatment of anal fissure on an outpatient basis / Coloproctology. 2022. T.18. No. S3(69) P.17. .
- Rivkin V.L. Transanal (internal) and paraanal (external) dosed sphincterotomy: indications, technique, practice // Gastroenterology. Surgery. Intensive therapy. - 2018. - No. 02. pp. 55–57.
On the website in the “Literature” section there is a subsection “Surgery of the colon and rectum”, containing medical articles related to the treatment of the rectum and diseases of the anal canal.
Video
Kitsenko Yu.E. Anal fissure. Elective “Basics of Coloproctology” (video)
Anal fissure with fistulous passage into the intestine. Still from the film: Tsodikov G.V. and others. Instrumental and laboratory methods for studying the gastrointestinal tract. Medfilm. 1985
On the website in the “Video” section there is a subsection for patients “Popular Gastroenterology” and a subsection “For Doctors”, containing video recordings of reports, lectures, webinars in various areas of gastroenterology for healthcare professionals.
Anal fissure in ICD-10
In the International Classification of Diseases ICD-10, anal fissure is classified as “Class XI. Diseases of the digestive organs”, section “K60 Fissure and fistula of the anus and rectum”, which includes the following subsections:
- K60.0 Acute anal fissure
- K60.1 Chronic anal fissure
- K60.2 Anal fissure, unspecified
Back to section