home
We treat
Urology
Cystitis
Acute cystitis
Prices Reviews Our specialists Make an appointment
Acute cystitis is a suddenly developing inflammation of the bladder, most often of an infectious nature. Belongs to common diseases. Mainly affects women. This situation is explained by anatomical features. In the female body, the urethra is short and wide, due to which the infection quickly passes through it and penetrates the bladder. In addition, the urethra is located next to the vagina and rectum - organs inhabited by a large number of opportunistic bacteria that can cause inflammation.
20-40 year old women suffer especially often from cystitis. The disease is diagnosed in every third representative of the fair sex.
Types of cystitis
There are primary and secondary cystitis. The primary form is an independent disease that usually occurs in women. Secondary cystitis develops as a complication of other diseases and is more common in men, especially in those who suffer from chronic prostatitis. Due to swelling and enlargement of the prostate, the outflow of urine may be impaired. In women, acute cystitis often develops with colpitis, candidiasis and bacterial vaginitis due to changes in the composition of the vaginal microflora. Often inflammation becomes a consequence of urolithiasis.
How is acute cystitis diagnosed?
Acute cystitis has a very clear clinical picture, so an experienced doctor can make a preliminary diagnosis based on complaints. To confirm it, the following are appointed:
- general analysis and bacteriological examination;
- general blood analysis;
- Ultrasound of the bladder;
- gynecological examination;
- bacteriological analysis of discharge from the urethra and vagina.
When the inflammatory process subsides, cystoscopy and cystography are prescribed. They are necessary to identify the cause of the disease. Since cystitis has manifestations characteristic of a number of other pathologies of the urinary system, it must be differentiated from pyelonephritis, urolithiasis and bladder tumors.
Causes of the disease
The inflammatory process is caused by pathogenic microflora that penetrates the bladder from the outside: from organs located in the pelvic area. Most often, the cause of the disease is Escherichia coli, less often other microorganisms (enterobacteria, enterococci, Proteus, Klebsiella, Pseudomonas aeruginosa, mycoplasma, ureaplasma, trichomonas, chlamydia, yeast-like fungi, gram-positive and gram-negative bacteria).
Various factors increase the likelihood of inflammation:
- hypothermia of the body, especially the pelvic area (when sitting on a cold surface) and legs;
- weakening of the immune system;
- overactive bladder;
- abnormal structure of the urinary system;
- a sedentary lifestyle, leading to stagnation of blood in the pelvic area;
- poor quality nutrition;
- abuse of salty and spicy foods, alcoholic drinks;
- frequent and prolonged constipation;
- the presence of chronic infectious foci in the body;
- self-treatment of sexually transmitted infections;
- frequent change of sexual partners;
- beginning of sexual activity;
- hormonal changes during pregnancy or menopause;
- multiple births leading to bladder prolapse;
- rough sexual intercourse;
- lack of personal hygiene;
- wearing compression garments;
- injury to the pelvic area;
- frequent lack of sleep;
- overwork;
- constant stressful situations;
- avitaminosis;
- elderly age.
Treatment of male cystitis usually includes the following methods:
- Prescribing bed rest to a patient during the acute stage of the disease, which is accompanied by fever and severe pain. In this case, antipyretic and painkillers are prescribed. During this period, the patient needs to drink plenty of fluids, more than 2.5 liters of water per day, and avoid spicy, salty and sour foods. Next is taking various medications.
- Taking antibiotics to which the pathogen is sensitive. Usually these are fluoroquinolones, nitrofurans and cephalosporins, these include drugs such as Nocilin, Normax, Tsiprolet A, Furadonin and others.
- Phytotherapy. To treat cystitis, it is necessary to prescribe diuretic and anti-inflammatory herbal teas from lingonberry leaves, horsetail and bearberry. Before prescribing herbal medicine, it is necessary to exclude the possibility of individual allergic reactions to medicinal plants in the patient. In addition, medications based on natural ingredients are prescribed: “Cyston”, “Fitolysin”. For cystitis, taking cranberries and cranberry juice or taking cranberry extract, for example, Monurel, will be useful. All herbal remedies must be used for a long period of time. It should be remembered that the main treatment is broad-spectrum antibiotics.
- Painkillers are prescribed to relieve pain and spasms. It is recommended to use antispasmodics - Papaverine, Drotaverine, as well as non-steroidal drugs - Diclofenac, Nimesulide.
- STI. Separately, treatment of sexually transmitted diseases is prescribed, for the diagnosis of which PCR is prescribed. Such diseases can cause the development of cystitis, so the possibility of their presence in the patient should not be missed.
- Symptoms of cystitis may differ depending on the type of pathogen and the diseases that caused it, which became the source of infection. Such diseases include: adenoma, prostatitis, kidney disease. Treatment of cystitis involves eliminating more dangerous symptoms.
- In some cases, the urologist may prescribe washing the inflammation, which is carried out using antiseptics and novocaine.
- Physiotherapeutic procedures, such as UHF, magnetic laser therapy, mud therapy and others, are also indicated in the treatment of cystitis in men; they contribute to the patient’s recovery and alleviate the course of the disease.
- a stay in sanatoriums in the Krasnodar and Stavropol Territories can have a beneficial effect on the patient’s condition.
Symptoms
A characteristic sign of acute cystitis is difficulty urinating:
- pollakiuria - frequent (every 10-15 minutes) and painful urination, urine output in small portions and in a small volume, a feeling of incomplete emptying of the bladder;
- stranguria - frequent and difficult urination caused by sharp pain at the beginning and end of the process;
- nocturia - the urge to urinate more frequently at night than during the day;
- imperative urges - a feeling that you need to urinate immediately, urinary incontinence is possible (if the neck of the bladder is inflamed).
The disease is accompanied by other symptoms:
- pain (usually acute), burning and itching in the genital area;
- cloudiness of urine, the appearance of a putrid odor;
- interspersed with blood and pus in the urine.
Weakness, decreased vitality, and increased fatigue are possible. Sometimes signs of intoxication appear: nausea, deterioration or loss of appetite. In some cases, the temperature may rise, which signals the spread of the inflammatory process to the kidneys and the development of pyelonephritis.
Why is cystitis more common in women than in men?
The main reason is the peculiarities of the physiological structure of the genitourinary system. The penetration of pathogenic microorganisms into the urethra and bladder is ensured by:
- short, wide urethra located close to the anus;
- the influence of hormonal changes on the weakening of the body’s protective functions;
- menopause, which causes a decrease in estrogen levels, weakening of the mucous membrane of the bladder (its atrophy);
- the complex structure of the female reproductive system, which contributes to the rapid spread of infections and bacteria into the urinary system and the development of cystitis.
Treatment
Treatment of acute cystitis does not cause difficulties for an experienced urologist. Antibiotics and anti-inflammatory drugs can cope with the problem. But in order to prevent relapse and avoid the transition of acute cystitis to chronic, it is necessary to find and eliminate the cause of the disease.
Drug treatment of acute cystitis includes:
- antibiotics;
- uroseptics;
- antispasmodics;
- analgesics;
- sometimes, non-steroidal anti-inflammatory drugs;
- rarely corticosteroids;
- immunostimulants;
- vitamin complexes.
In the absence of adequate treatment, the disease becomes chronic, which significantly complicates therapy or causes complications (pyelonephritis, urine reflux).
During treatment you will have to abstain from sexual intercourse and adhere to a diet: exclude salty and spicy foods from your diet, give up coffee and carbonated alcoholic drinks. You should drink at least 2 liters of liquid (preferably clean water) per day to relieve intoxication and free the bladder from pathogenic microflora.
When choosing a treatment method, the doctor takes into account the patient’s age and the presence of concomitant diseases. The urologist takes special care when treating pregnant women in order to protect the fetus.
Typically, treatment of the acute form of the disease takes no more than 5 days.
In the specialized clinic of urology and gynecology Uclinica, consultations are conducted by doctors of the highest category. They will individually select medications, which will ensure a quick recovery and return to your normal lifestyle.
To make an appointment with a urologist, call 8 or fill out the online form.
Uclinica doctors will help you quickly recover from cystitis and prevent the disease from recurring. Reception is conducted by specialists of the highest category.
Contact a specialist:
| Primary appointment with a urologist | 1500 rub. |
| Cystoscopy | 4500 rub. |
| Bladder instillation (1 session) | 1500 rub. |
Go to Contacts Make an appointment
Why is it important to see a doctor on time?
Only a doctor should prescribe medications, since the same antibiotic may not be effective against different types of bacteria. Even if the medications you choose yourself help, this does not mean a cure. Perhaps the acute inflammatory process has subsided and become chronic.
To prevent this from happening, contact our clinic when the very first signs appear. You will be provided with qualified medical care, all the necessary examinations and effective treatment will be prescribed. Make an appointment using the online form or call us at or.
doctor
Specialized multidisciplinary clinic
Our staff consists of high-class doctors - members of the Russian and European Societies (EA).
We have a day hospital
We guarantee constant care for the patient and control over his recovery in the most comfortable conditions.
Low-traumatic treatment methods
We carry out operations with minimal intervention in the body using modern equipment of the new generation of intraoperative X-ray systems.
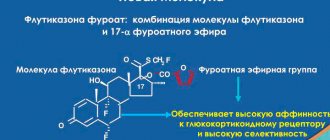
New opportunities in the treatment of cystitis. Krivoborodov G.G.
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– Dear colleagues, today concludes our Internet session, our marathon today from 8 o’clock, the urology section. And in this section you will have to communicate with two very interesting lecturers. Professor Grigory Georgievich Krivoborodov: “New opportunities in the treatment of cystitis.”
Grigory Georgievich Krivoborodov , professor, doctor of medical sciences:
– Dear colleagues, today is indeed the day when I will talk about lower urinary tract infections for the second time, because not everyone probably knows, but today a conference called “Fundamental Urology” began. This conference is held under the auspices of the Moscow Society of Urologists, it takes place at the mayor's office and under the patronage of the mayor's office. One of the issues that was already discussed there today (and we will also discuss this issue now) is the treatment and prevention of urinary tract infections. Our block today will consist of two lectures. First, we will discuss what is new in the treatment of lower urinary tract infections in women, and the next presentation will be regarding the prevention of urinary tract infections.
I spoke for so long at the beginning because this is a very important issue. We haven't been very focused on treating lower urinary tract infections before. This is an acute cystitis that occurs in women, which almost never occurs in men. And there are certain anatomical prerequisites for the fact that women have cystitis, and men have acute prostatitis.
This slide is not a tribute to fashion, it is recently the responsibility of those who speak, and my colleagues also constantly show such slides. This is information about cooperation, that is, those pharmaceutical or other companies with which I cooperate in one way or another. This slide simply shows that I do not have any interest in any one company. Sometimes you have to cooperate with companies that produce medications with approximately the same mechanism of action.
Why are we talking about acute cystitis today? Why are we talking about uncomplicated lower urinary tract infection today? Because it's relevant. There is evidence that in the United States more than two million visits to the doctor are recorded annually and these visits are associated with cystitis. Approximately 10% of women suffer from the so-called recurrent lower urinary tract infection or, as we usually say in our country, chronic cystitis.
Another important message is economic costs. Today, unfortunately, or perhaps fortunately, we are forced to count the economic costs that go into the treatment of certain diseases. I cannot share the same information regarding Russia, but in the United States, 15% of antibacterial agents are used to treat urinary tract infections, and their cost is $1 billion. United Europe is 1.5 billion dollars. These are very significant figures that we, of course, must take into account today.
What could be simpler than diagnosing acute cystitis? An uncomplicated urinary tract infection is a very typical, characteristic clinical picture. We must understand that acute cystitis is always caused by bacterial flora. That is, the cause of acute cystitis is a bacterium, a bacterial invasion. The inflammatory process in uncomplicated cystitis is limited to the mucous membrane of the bladder or, as we also call it, the urothelium. It occurs mainly in healthy women without any concomitant structural or functional disorders of the urinary tract.
And this is a very typical picture of acute cystitis. First of all, these are the so-called dysuric symptoms: frequent urination, urgency or so-called urgent urination, imperative urination (that is, a woman has an urge to urinate, which she cannot put off, and often must, of course, visit the toilet, sometimes even to urinary incontinence), pain in the suprapubic region, urine with an unpleasant odor. And another very important and dangerous symptom is hematuria, that is, blood in the urine. And when this symptom occurs, we must understand that the woman has an increased risk of recurrent lower urinary tract infection, that is, in the future, perhaps recurrent cystitis will occur.
Diagnostics. Diagnostics is very simple and mandatory. If we want to clearly confirm bacterial inflammation of the bladder mucosa, then a urine test is performed. In urine tests, bacteriuria and leukocyturia are typical for acute cystitis. If we determine the passive urine, and the bacterial titer is 103 CFU/ml or more, then we can diagnose acute cystitis.
What causes an uncomplicated lower urinary tract infection? This is a study that took place in 2005-2006. We know very well that the most common cause of acute cystitis is Escherichia coli, the most common infection. In recent years, there has been a tendency that the number of patients with E. coli is slightly decreasing and the number of patients in whom the cause of acute cystitis is gram-negative or gram-positive flora is increasing. These include Proteus, Klebsiella, Staphylococcus, and other infections. In 96% of cases, this is a monoinfection - one microorganism that causes bacterial inflammation of the mucous membrane of the bladder.
Today we will talk about acute cystitis, recurrent cystitis. And if we are now starting to discuss the problem of treating acute cystitis (and I have attached data that this is an emergency situation, this is a situation that requires immediate measures aimed at improving the quality of life of such women), then the goal of this treatment, of course, first of all, is quick elimination of clinical symptoms or eradication of the pathogen. And the first goal is achieved by solving the second goal.
Today we should already understand that our treatment must be targeted. When treating acute uncomplicated cystitis, we should already think about repeated cystitis, recurrent infection, and engage in the prevention of recurrent infection, which will be discussed in great detail in the next lecture. Today there are opportunities to prevent recurrent cystitis.
Why are we talking about this today? Because there is a trend towards an increase in the number of women with recurrent lower urinary tract infections. We don't fully know the cause of this condition, but this trend is attracting the attention of many doctors. These are, first of all, therapists who are the first to encounter this problem. Women more often turn to general practitioners and gynecologists, because a urologist is not always available at the outpatient level.
Of course, today we must understand that the main method of treating cystitis is antibacterial therapy. And other types of treatment are currently not being considered for acute conditions, because only antibacterial drugs show in placebo-controlled studies the effectiveness of treatment for this category of patients.
What antibiotic should we use to treat women with this condition today? The slide presents the so-called optimal antibacterial drug. This is a high microbiological activity against topical pathogens with a high concentration of the drug in the urine. And we understand that those antibiotics that predominantly accumulate in the urine are called uroantiseptics.
A very important point is good tolerability, safety and low cost. What is low cost? For each region this is an issue that requires discussion. But we must understand that today the situation is so catastrophic that we should no longer talk about the cost of treatment, not about the cost of an antibacterial drug, but about its good effectiveness and tolerability. These are the two main important points. Because this therapy is most often short-lived and the material costs are not that large, it is not possible to save money here for fear of developing a re-infection. Recurrent cystitis will require much more treatment.
Availability of an oral dosage form. This is a very good and very important indicator for the treatment of acute cystitis with an antibacterial agent. Why? Because, I emphasize again, in most cases there is no need to hospitalize these women. This is an outpatient link and here the presence of an oral form is very important.
The possibility of a single daily dose is also a convenient situation.
Possibility of short course therapy with good results in terms of clinical efficacy, microbiological activity and tolerability.
What do we have today among antibacterial agents that we can use to treat patients with acute cystitis? This table, please note, presents the microorganisms that most often cause acute cystitis, and all currently existing antibacterial agents that are used to treat this group of patients.
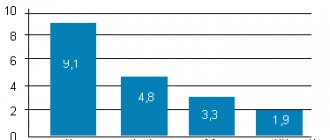
Let's start with the first, most commonly used drug, this drug "Fosfomycin". This is a fairly well-studied well-known drug, which in the last, probably, 10 years has been most often used to treat acute cystitis. What is its microbiological activity? In 2002, 97.9 and in 2004, 97.2 – these are the data for E. coli. And then in relation to pseudomonosis, Protea, Klebsiella, staphylococci, the effectiveness is much less.
The next drug that is most commonly used to treat this condition is Fluoroquinolone. It is clear that in our country, in different regions, the sensitivity of microorganisms to fluoroquinolones is different. As the slide shows, the data is depressing. Look, E. coli – 77%. We know very well that there is such an indicator - sensitivity to antibacterial agents. If the resistance of the insensitive form is 20%, then the question arises about the need to use the drug to treat any infection. Fluoroquinolones, of course, are good drugs that we use to treat mainly complicated infections, and not only lower urinary tract infections, but to treat complicated upper urinary tract infections. These drugs are used in abdominal surgery.
And there is even a point of view that today we must preserve this good group of antibacterial agents for the treatment of complicated forms of upper and lower urinary tract infections, since in the near future there is no prospect of obtaining new antibacterial agents. By 2022, those promises that three completely new molecules of antibacterial agents will be invented, unfortunately, do not justify themselves, and, most likely, they will not appear by 2020. Therefore, we should be concerned about fluoroquinolone resistance and reserve these drugs for the treatment of complicated infections.
"Nitrofurantoin". These are nitrofurans. These are drugs that have good effectiveness against E. coli. With regard to other microorganisms, as presented on the slide, the situation is somewhat different. What should we be afraid of when using Nitrofurantoin? Firstly, the data that we have on Nitrofurantoin is data that concerns a macrocrystalline drug. These are completely different doses that are used abroad, and are currently and have never been presented on the drug market in Russia. Therefore, when prescribing domestically produced nitrofurans, we actually do not have clear data on their treatment effectiveness, although we know clinically that most often these drugs work quite well in the treatment of acute cystitis. Another very important point. In recent years, several cases of side effects from nitrofurans have been described, which consist of impaired liver function, primarily, and the development of fibrosis of the lung tissue, sometimes with a fatal outcome. Therefore, long-term administration of nitrofurans can be dangerous.
And finally, another group of drugs that we know well and have been on the drug market for a long time are third-generation cephalosporins - Cefixime. The data presented on this slide shows that these drugs currently lead in their effect on E. coli and other microorganisms that most often cause acute cystitis.
I do not want to lobby for this or that drug, but today we are on the threshold that, given the problems with antibacterial drugs, we must be especially careful in choosing a drug to treat women with acute cystitis. And as all of the above shows, there are probably very clear reasons for prescribing third-generation cephalosporins in the treatment of uncomplicated lower urinary tract infections in women.
According to the FDA, the Food and Drug Administration in the United States, single-dose therapy is inferior in effectiveness to therapy with short courses of antibacterial drugs. Indeed, the number of women with recurrent cystitis is increasing who take Fosfomycin once, take it a second time, take it a third time, and then a situation occurs when Fosfomycin does not work. Why do these women, after the first onset of cystitis, relapse when using one dose of the drug? Maybe we need to return to short courses of antibiotic therapy for 5-7 days with better effectiveness? For now this is just a guess and requires further study, but this trend exists.
Again we return to fluoroquinolones. Ciprofloxacin is probably the most frequently used drug in our country. Please note that 2001 – resistance was 2.1%, 2005 – 4.7%, 2008 – 10%. Now we are talking about 14-17%, this is a pretty bad situation that should, of course, alarm us.
If we are talking about a drug that accumulates well in urine as a drug for the treatment of uncomplicated lower urinary tract infections, then Cefixime, a third-generation cephalosporin, ideally suits this situation. Their pharmacokinetics is such that within 24 hours the concentration of the drug is 10 times higher than the minimum inhibitory concentration - the antibacterial agent is enough to destroy more than 90% of the microorganisms that most often cause acute cystitis. That is, “Cefixime” fully meets the requirement of a drug with good ability to accumulate in urine for the treatment of acute cystitis.
In addition, we must pay attention that if we compare third-generation cephalosporins with Fosfomycin, we must understand that we cannot use Fosfomycin for the treatment of cystitis and pyelonephritis, which are often combined together (the so-called cystopyelonephritis). If we are talking about cefixime, then it is clear that this drug accumulates well in the renal parenchyma, and thus it can be used in situations where a woman has cystitis and subsequent pyelonephritis, or a condition that is combined together.
Clinical base that proves the effectiveness of Cefixime for uncomplicated urinary tract infections. We can talk about microbiological effectiveness. If we are talking about Fosfomycin, then, unfortunately, the data that the drug accumulates well in the urine and destroys a sufficient number of microorganisms is mainly based on microbiological studies, which are not fully confirmed by data from clinical studies. What about cefixime in the clinic? Almost 90% clinical effectiveness of using short courses of Cefixime in the treatment of acute cystitis. You see, this is 3 days, two doses. And, probably, the results will be just as good, maybe even better, if we use the drug for 5-7 days.
Here is another important table to summarize all the antibacterial agents that we use in the treatment of acute cystitis. "Cefixime": good effectiveness against almost all microorganisms that most often cause acute cystitis, is effective against pyelonephritis, can be used during pregnancy (I forgot to say this). If we are talking about cystitis and pyelonephritis of pregnancy, then Fosfomycin is also good for cystitis and can be used. We understand that third generation cephalosporins (“Cefalosporin”) are the drugs of choice for the treatment of infections of some inflammatory processes in pregnant women. The drug can also be taken regardless of food intake. In general, a small one, but an advantage, at least for the doctor. When the patient asks him: “When should I take the drug - before, after, during or instead of meals?” - then the doctor can say: “Take it whenever you want.”
Adverse reactions. Today we have already talked about pseudomembranous colitis and diarrhea when using antibacterial drugs. Sometimes, when prescribing an antibacterial drug, we do not have such complications during treatment, but these complications can arise within two to three days, even within a month after the end of therapy. Please note, as shown on the slide, Cefixime causes diarrhea in only one percent of cases. This is also a good indicator, indicating that this drug is well tolerated.
This is the packaging, this is the drug - Suprax. I emphasize once again that I am far from advertising any drugs. I'm just introducing to you that it comes in a dose of 400 mg, used once a day, a very convenient soluble form to use. It’s better to combine it with the drug “Uro-Vaxom”, which my colleague will tell you about. This is how this drug is used for treatment. Favorable safety profile: has a gentle effect on intestinal microflora, belongs to category B according to the FDA classification and can be used in pregnant women. In conditions of resistance of uropathogens to fluoroquinolones, third generation cephalosporins, high activity against community-acquired strains of Escherichia coli, low potential for selection of resistant strains, high concentrations not only in urine, but also in the kidney parenchyma, safety during pregnancy, minimal frequency, convenience, variety of methods reception.
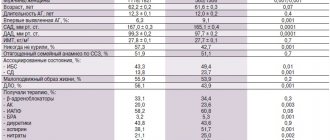
Chronic cystitis. It is probably better to talk about the recurrent effect of the lower urinary tract. When do we talk about this? We talk about this when a woman contacts us more than twice in six months or more than three times in a year. And here are again the depressing statistics: within 3-4 months after the first episode of urinary tract infection, 20-30% of women experience a relapse (that is, every second, third out of ten will most likely have a relapse of the infection), 10- 20% of women experience this recurrent infection (what we talked about at the beginning of our talk today).
This slide, it seems to me, is very important because we sometimes don’t think about how much this condition disrupts the quality of life of women. One out of two female patients has recurrent cystitis. That is, 50% of patients have relapses more than three times a year. Maybe it's 5 times a year? Maybe it's 6 times a year? This situation also happens. And even more. We no longer know how to treat this category of women. This is a big problem. Imagine how much this disables the patient, what the economic costs are, what problems with sex life, problems in the family and problems at work. It seems like a simple disease – cystitis: take a pill and you’re healthy for tomorrow. Not always. Why? We must talk about this today. And we should not deceive our women who come to us for appointments. The goal of treating acute cystitis (this is such an old, well-known slide) is to eliminate the pathogen and eliminate the symptoms. The goal of treating a recurrent infection is only to increase the disease-free period and improve the quality of life. We cannot guarantee a woman with recurrent cystitis that she will return to normal life and be healthy. We can only talk about increasing the duration of the disease-free period.
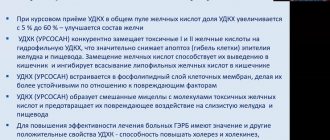
I will not talk about macro and microbial factors, which may play a leading role in the development of cystitis, because we have been talking for quite a long time today. But much attention is currently paid to the state of the urothelium of the bladder, its ability to prevent the binding of microorganisms with the help of fimbriae, umbrella cells of the wall of the mucous membrane of the bladder.
Why am I talking about this? I tell our colleagues that there is no need to simply mechanically instill various medications into the bladder, which most often are not licensed for the treatment of some kind of infection. Usually this does not lead to real improvement in the condition, and has an even worse effect on the possibility of relapse and subsequent treatment.
Microorganism factors. It is clear that microorganisms also have certain virulence factors, the ability to attach to the mucous membrane of the bladder and reside there in the form of cocoons. Periodically, these cocoons break, a pre-multiplication of these bacteria occurs, and they are released into the cavity of the bladder. This may be why lower urinary tract infections recur.
Guidelines for the treatment of women with recurrent lower urinary tract infection. In first place is the so-called long-term antibacterial prophylaxis using low doses of antibacterial drugs. In this situation, half doses of cephalosporins, fluoroquinolones, nitrofurans are used, or Fosfomycin therapy is used for several days. And you ask me: “How long?” Three months to a year (please note). We prescribe this drug treatment for a year. So what, the woman was cured? Unfortunately, after the end of this drug therapy, after 3-4 months, in my opinion, 60% of women have a recurrence of lower urinary tract infection. And today we should use antibacterial prophylaxis only in those women when other types of treatment do not allow increasing this relapse-free period and are ineffective.
Here is another very important slide, this is what I talked about about nitrofuran, because in Russia we use nitrofurans very often. There is a society that says: “Do not use Nitrofurantoin for prophylaxis.” Why? Because very often there are side effects from the liver and lungs, they are associated with long-term use of Nitrofurantoin.
Many patients experience recurrent urinary tract infections. Many strategies have been proposed. Despite this, we are far from perfect; only a few antibiotics are suitable for treating infection. And, of course, it is necessary to develop alternative strategies.
What can we do today, right now? First of all, we must be very careful when prescribing antibacterial agents. We are already a country that has good international connections. Doctors from other countries come to our country. When they realize that they can buy any antibacterial drug (and not only) anywhere - in the subway, at a train station, in any pharmacy - it plunges them into shock, because there must be strict control over the sale of medicines. Only a doctor can understand who should be prescribed which drug and in what doses, because everything is poison and everything is medicine. You need to use doses. And we, doctors, must, of course, advocate for this. Mandatory adherence to the principles of prescribing antibacterial drugs. And epidemiological control of medical institutions is very important: what microorganisms are present there, how sensitive they are to certain antibacterial agents. This plays a leading role in the choice of medicines.
Here are my contact details: Professor Grigory Georgievich Krivoborodov, telephone 8-903-105-00-00, e-mail If there are questions regarding either a patient who requires consultation, or there are questions for discussion, we are always open, our urology clinic of the Russian Scientific -Research Medical University named after N.I. Pirogova is always ready to cooperate not only with urologists, but also with doctors of other specialties.
Our partners
Phlebology Clinic First Phlebological Center
Phlebology Clinic First Phlebological Center.
Treatment of varicose veins by leading specialists from Russia using the most advanced equipment. The head of the clinic is Viktor Nikolaevich Lobanov, a vascular surgeon and phlebologist. The clinic’s doctors have more than 20 years of experience, which makes it possible to treat chronic diseases, as well as perform operations even at the most severe stages of venous disease. The Phlebology Center is located at: Moscow, st. Dmitry Ulyanov, 31. Phone: +7(495) 967-94-42.
Patients of our urology clinic are provided with preferential conditions for consultations, diagnostics and further treatment.
Etiology
The causative agent of acute uncomplicated cystitis in most cases (about 80–90%) is Escherichia coli
and much less often - other pathogens of urinary infection:
Staphylococcus saprophyticus, Klebsiella spp., Proteus spp.
and others [4].
Currently, multicenter clinical studies are regularly conducted around the world to monitor UTI pathogens and their antibiotic resistance. The largest international study, ECO-SENS, involving 4,734 patients from 252 clinics in 16 countries in Europe and Canada, which ended in 2003, revealed the following patterns: in 77.7% of patients, UTIs were caused by E. coli
, in 5.2% -
Proteus mirabilis
, in 2.8% -
Klebsiella spp
., in 3.9% - other representatives of the
Enterobacteriaceae
, in 4.6% -
S. saprophyticus
and in 5.8% - other microorganisms.
29.8% of the isolated strains of microorganisms were insensitive to ampicillin, 29.1% to sulfamethoxazole, and 14.8% to trimethoprim. E. coli
strains to ciprofloxacin, the combination of amoxicillin and clavulanic acid, nitrofurantoin, gentamicin and fosfomycin trometamol was observed in less than 3% of patients [5].
In Russia, under the leadership of Professor L.S. Strachunsky, similar studies were conducted: UTIAP I (1998–1999), UTIAP II (2000–2001) and UTIAP III (2004–2005). During these studies, it was found that in Russia, acute cystitis was caused by E. coli
, in 6% -
Klebsiella spp
., in 1.8% -
Proteus spp.,
in 1.6% -
S. saprophyticus
, in 1.2% -
Pseudomonas aeruginosa
etc.
E. coli
resistant to ampicillin were found in 22.7-44% of cases, to co-trimoxazole - in 16.2-26.9%, to nitroxoline - in 6.8-7.9% of cases.
Resistance of E. coli
to norfloxacin, ciprofloxacin and nitrofurantoin was noted in less than 3% of patients with acute cystitis [6, 7].
The multicenter study "DARMIS-2011" showed that among the causative agents of UTIs, the proportion of representatives of the family Enterobacteriaceae
amounted to 83.5%.
At the same time, E. coli
was detected in 63.5% of patients.
In general, the frequency of pathogen isolation did not differ significantly between patients with complicated and uncomplicated UTIs [8]. In the DARMIS-2018 study, the detection rate of E. coli
in the group of patients with uncomplicated infection was 74.6%, complicated - 67.2%,
Klebsiella pneumoniae
- 9.6% and 12.7%;
P. mirabilis -
3% and 4.6%;
Enterococcus faecalis -
5% and 6.3%;
Staphylococcus spp.
— 2.3% and 1.2%, respectively;
the proportion of P. aeruginosa
that was detected in complicated UTIs was 1.7%.
E. coli
strains to ampicillin (57.7%), amoxicillin/clavulanate (43%) and trimethoprim/sulfamethoxazole (36.9%) was recorded; a decrease in sensitivity to ciprofloxacin (60.6%) was also noted, which was significantly lower than 7 years ago (79.9%). Compared with the previous study, according to DARMIS-18, the number of pathogenic microorganisms producing extended spectrum β-lactamases increased statistically significantly - from 8.5% to 27% [8].