Home | About us | Delivery | Advertisers | Login | Registration
Delivery on Sundays and holidays does not work!
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2022 Pharmacy 84.
Calcitriol: new possibilities of a well-known compound
Calcitriol, an active metabolite of vitamin D3, has been used for many years to treat secondary hyperparathyroidism in patients with stage IV-V chronic kidney disease. Along with traditional target organs (kidneys, intestines, parathyroid glands), calcitriol, interacting with specific enzymes (VDR) in various organs and tissues, actively influences many biological processes in the body, providing improved survival of patients on renal replacement therapy, providing nephroprotection with progressive nephropathies, increases resistance to infections. This review focuses on both traditional and non-traditional effects of calcitriol.
Calcitriol (1,25-dihydroxycholecalciferol) is a metabolite of vitamin D (VD), formed by adding two hydroxyl groups (OH) at the 1 and 25 positions to the native VD. The term “vitamin D” combines a group of several forms of VD (D1-D5) similar in chemical structure (sexosteroids), of which only D2 and D3 have found wide clinical use in various human pathologies.
VD is traditionally classified as a group of fat-soluble vitamins, however, VD is not a vitamin itself, since only through two-stage metabolization it is converted into an active form and, like a hormone, has diverse biological effects by interacting with specific receptors in the nuclei of cells of various organs and tissues. Therefore, calcitriol formed in the kidneys is justifiably called D-hormone.
The discovery and clarification of the mechanisms of action of VD is closely related to the history of rickets, the first reliable description of which dates back to the middle of the 17th century, although disabling skeletal changes associated with insufficient exposure to the sun for religious and other reasons were known in ancient times. In the last quarter of the 19th century, data from autopsies carried out in Boston and Leiden indicated that 80-90% of deceased children had signs of rickets. In 1822, J. Sniadecki recognized the importance of sun exposure for the treatment and prevention of rickets, and T. Palm (1890) treated rickets with sunbathing.
Experimental study of rickets began at the beginning of the twentieth century, when B. Mellanby et al. reproduced rickets in dogs and treated the animals with cod liver oil. Ultraviolet irradiation of products, such as milk, enhanced its antirachitic properties. A similar effect was achieved by feeding ultraviolet-irradiated yeast to cows. The conducted studies revealed that there are 2 main forms of VD: vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol). The source of cholecalciferol is animal products - fish oil, liver, eggs, etc. D3 is partially formed in human skin from 7 dehydrocholesterol under the influence of ultraviolet radiation, and skin melanin competes for ultraviolet rays and people with dark skin need longer ultraviolet exposure than white-skinned people to produce an equal amount of cholecalciferol. In older people, cutaneous production of D3 is reduced by 70% compared to young people. Because of this, older and dark-skinned people under physiological conditions need to increase their intake of dietary cholecalciferol.
Ergocalciferol is formed from ergosterol under the influence of ultraviolet radiation. Ergosterol is a major component of plant cell membranes, performing the same function as cholesterol in animals and humans.
In the human body and other mammals, vitamins D2 and D3 are included in chylomicrons, enter the lymphatic system and subsequently into the circulation, binding to the carrier protein (TRP). In the liver, both compounds undergo hydroxylation (the addition of an OH group to the carbon atom at position 25) with the participation of 25-hydroxylase. 25(OH) D (calcidiol) is the main circulating form of VD, the half-life of which is 14 days, reflecting the reserves of VD in the body, and the concentration of which correlates with the development of rickets in children, osteomalacia in adults and secondary hyperparathyroidism (SHPT) in patients with chronic renal failure. . The 25(OH) D-DVP complex, filtered in the renal glomeruli, binds to megalin in the plasma membranes of the proximal tubules and enters the tubular epithelial cells. In mitochondria, 25(OH) D is released from connection with VD and converted by 1α-hydroxylase into 1,25(OH)2 D3-calcitriol, which is the active form of VD, involved in various biological reactions and in the regulation of mineral homeostasis in healthy people and patients with CKD .
Together with parathyroid hormone (PTH), calcitriol ensures a stable level of calcium in the blood, increasing the absorption of Ca2+ in the gastrointestinal tract, and promotes the release of calcium from the skeleton by enhancing osteoclastic resorption, and also enhances the absorption of phosphate in the intestine by translocation of the Na/Pi phosphate transporter IIb type from the cytoplasm to the apical membrane of enterocytes. In the kidneys, calcitriol enhances the expression of megalin in the proximal tubules, suppresses the activity of 1α-hydroxylase and activates 24-hydroxylase, controlling its own homeostasis, enhances PTH-dependent calcium reabsorption in the tubules, and in bone tissue promotes the differentiation and maturation of osteoclasts. By reacting with VDR on the parathyroid glands (PTG), calcitriol affects the proliferation of gland cells and controls the secretion of PTH.
The listed effects of calcitriol are carried out by its interaction with specific receptors (VDR) and the complexation of this structure with RXR (retinoid acid X receptor). The resulting complex (calcitriol-VDR-RXR) enters the nucleus of cells, for example, enterocytes, where it reacts with the D-responsive element (VDRE). The result of the interaction is the expression of Ca channels on the apical membrane of enterocytes, through which calcium enters the enterocyte and, with the participation of calcium binding protein (calbindin 9K), quickly overcomes the intracellular spaces and enters the circulation; at the same time, gene transcription and synthesis of osteocalcin, ostepontin, alkaline phosphatase are enhanced and the production of pro-inflammatory cytokines (interleukin-2 and interleukin-12) and peptides related to PTH is reduced.
During dietary calcium deficiency, VD interacts with VDR on osteoblasts, inducing the expression of RANKL (a ligand of the receptor nuclear factor activator (NF-κB) on the plasma membrane of cells. The receptor activator of NF-κB (RANK) of the plasma membrane of preosteoclasts interacts with RANKL, accelerating the differentiation of preosteoclasts into mature osteoclasts. The latter, producing HCl and collagenases, dissolve the bone tissue matrix, releasing calcium and phosphorus into the circulation, maintaining a constant level of calcium in the blood. Thus, the main physiological function of VD is to maintain normal levels of phosphorus and calcium in the blood, necessary for the mineralization of the skeleton , ensuring metabolic functions, including the conduction of excitation along the nerves.
The traditional target organs for calcitriol are the skeleton, gastrointestinal tract, kidneys, and parathyroid gland, but VDRs are also found in the myocardium, muscles, brain, pancreas, gonads, etc., indicating numerous regulatory functions of this VD metabolite. The genomic effects of calcitriol are realized within a period of several hours to several days. Non-genomic effects that develop in the interval from several minutes to several hours include a rapid intestinal increase in calcium absorption (transcaltachia), increased insulin secretion by pancreatic β-cells, opening of Ca and Cl channels in osteoblasts, and increased migration of endothelial cells. The non-genomic effects of calcitriol are thought to be mediated by VDRs present on the apical cell membrane.
The interaction of calcitriol with VDR on PTG cells reduces the expression of PTH mRNA, thereby reducing the synthesis and secretion of PTH, and suppresses the hyperplasia of PTG cells. Against the background of progressive nephropathies, occurring with hypocalcemia and hyperphosphatemia, the expression of transforming growth factor alpha (TGF-α) and its receptor and the epidermal growth factor receptor (EGF) increases on PTG cells, causing hyperplasia of PTG cells and increasing the secretion of PTH. Calcitriol induces the formation of intracellular inhibitors (p21 and p27), which interrupt the signal for activation of TGF-α/EGF (1).
In patients with CKD, all parts of the regulation of phosphorus-calcium metabolism are disrupted, including a decrease in calcitriol production. The main reason for the decrease in the formation of 1,25(OH)2D3 is the destruction of the sites of its formation in the area of the renal proximal tubules, but at the same time, under the influence of hyperphosphatemia, which develops as a result of a decrease in phosphate excretion by the kidneys and an increase in the level of fibroblast growth factor (FGF23) in the blood, the activity of 1α- decreases. hydroxylase, which converts 25OHD to 1.25 (OH)2 D 3. In addition to the kidneys, calcitriol is synthesized by activated macrophages, which is associated with hypercalcemia in sarcoidosis, and in the placenta, however, macrophage production does not compensate for calcitriol deficiency in patients with kidney disease, which impairs calcium absorption in the intestines and permanent hypocalcemia. The latter, along with hyperphosphatemia, is a trigger for the development of secondary hyperparathyroidism (SPTH), the most common form of renal osteodystrophy.
An increase in the concentration of PTH in the blood of patients with CKD is observed when the glomerular filtration rate is ≤ 60 ml/min and increases as nephropathy progresses. Under the influence of PTH secreted in excess, resorption cavities are formed in the bones, filled with disorganized osteoid, the mineralization of which forms disordered bone (woven lone), prone to long-term non-consolidating fractures. With a prolonged course of SHPT, fibrosis of the trabecular bone develops (fibrosive osteitis), and calcium released as a result of bone tissue resorption, when hyperphosphatemia is not tightly controlled, causes calcium phosphate deposits in various organs and tissues, including in the walls of blood vessels, including coronary vessels, and heart valves, exacerbating cardiovascular morbidity and mortality. The most pronounced manifestations of SHPT are observed in patients on renal replacement therapy, however, prevention and treatment of SHPT must begin in the early stages of CKD.
Treatment of SHPT includes controlling hyperphosphatemia (prescription of phosphate-binding gels) and hypocalcemia (calcitriol and other VDR activators), prescribing calcium mimetics according to strict indications, and correcting acidosis, which increases the mobilization of calcium from the skeleton.
The dose of calcitriol, the therapeutic use of which began in 1972 (2), ranges from 0.25 mcg or every other day in patients with early chronic renal failure to 1.5 mcg/day. in patients on RRT. In the latter, the drug can be prescribed daily or at a double dose every other day or 2 times a week, which provides the same reduction in intact PTH (iPTH) as daily dosing, but reduces episodes of hypercalcemia. Intravenous administration of calcitriol is considered even more effective. Meta-analysis of 21 clinical studies on oral and intravenous calcitriol at doses ranging from 2.0 to 7.4 mcg/week. demonstrated faster and more profound suppression of PTH production when administered intravenously (3). When taken orally, the bioavailability of calcitriol does not exceed 50%, and adverse reactions develop more often.
Calcitriol increases the absorption of calcium in the small intestine and therefore its administration is combined with additional calcium intake (500-1000 mg/day), which is especially important for patients with predialysis chronic renal failure who are on a diet limited in protein and, accordingly, calcium. Along with calcium, calcitriol increases the absorption of phosphate in the gastrointestinal tract, which is especially rich in meat, fish, and dairy products. An increase in blood phosphorus levels stimulates PTH production and induces metastatic calcification. Therefore, correction of hyperphosphatemia is an essential element in the prevention and treatment of SHPT.
In addition to the traditional target organs that regulate phosphorus-calcium metabolism, VD, or more precisely calcitriol, which historically has long been considered an antirachitic factor, interacts with specific receptors and controls many biological processes in the body.
D-hormone affects the cardiovascular, renin-angiotensin, muscular, hematopoietic systems, processes of differentiation, proliferation and apoptosis, due to which vitamin D is successfully used to treat psoriasis, various malignant tumors, autoimmune diseases, etc. D-hormone suppresses the production of type I collagen in the myocardium, the accumulations of which are primarily susceptible to calcification (4), inhibits the formation of calcification factors - matrix Gla-protein and Runx2/Gbfal (5) and increases the expression of calcification inhibitors - MBP2, β-catenin, interleukin-6. By suppressing the formation and secretion of PTH, calcitriol mitigates the negative effects of PTH on the cardiovascular system, endothelial dysfunction, LVH, the development of myocardial fibrosis (6), and proliferation of smooth muscle cells (7). In VDR knockout mice, the renin-angiotensin system (RAS) is hyperactive, causing LVH, while in animals treated with D hormone, these changes are absent, as well as increased production of atrial natriuretic peptide (ANP) by cardiomyocytes treated with endothelin-1 ( 8). Treatment with calcitriol reduces LVH in both animals with spontaneous hypertension and in patients on program hemodialysis (9).
In the general population, vitamin D deficiency is combined with cardiovascular pathology (10), and the use of vitamin D modifies such risk factors as insulin resistance, metabolic syndrome, obesity, and susceptibility to thrombosis (11). Vitamin D supply in the population is associated with lower blood pressure (BP) (12).
VDRs are found on B and T lymphocytes and VD deficiency is accompanied by a decrease in T-cell immunity (reduction in the number of natural T killer cells, production of γ-interferon, IL-2) (13), while replenishment of VD deficiency normalizes the immune response (14).
Calcitriol blocks exacerbations of recurrent encephalomyelitis in animals, which is a model of multiple sclerosis, and prevents and even cures autoimmune type I diabetes in rats, preventing the destruction of pancreatic islet cells. Calcitriol has been noted to have a beneficial effect on the course of lupus nephritis, inflammatory bowel disease, rheumatoid arthritis (15) and transplant rejection (16).
In patients with terminal uremia, various infections occur many times more often than in the population, being the second main cause (after cardiovascular complications) of deaths. In addition to complications associated with vascular access, dialysis patients are susceptible to respiratory infections. Cathelicidins are a family of antimicrobial peptides that are part of the innate immune system and are active against gram-positive and gram-negative microbes, viruses and fungi. Only one of these peptides (hCAP 18-cathelicidin autimicrolal peptide), designated LL-37 after its active fragment, has been found in humans (17). The human gene encoding hCAP18 is transcriptionally regulated by VDR and is enhanced by calcitriol administration in vitro
production of hCAP18 in many organs and tissues. Hemodialysis patients with low circulating hCAP18 levels have an increased risk of infectious complications (18).
VDRs are expressed on skeletal muscle cells in animals and humans, and in VDR knockout mice, along with changes in the structure (shortening) of muscle fibers, hypocalcemia, hyperphosphatemia, and increased production of pathologically altered muscle proteins (myf5, myogenin, myosin light chain isoforms) are observed. . In older adults, the number of muscle VDRs progressively decreases, but calcitriol may be able to slow age-related muscle changes (24).
Calcitriol and other metabolites of vitamin D, due to their effect on the activity of the RAS, can enhance the erythropoietic response to rhERP, and, by reducing proteinuria, slow down the progression of chronic renal failure. Treatment of rats with subtotal nephrectomy with calcitriol slowed down the development of glomerulosclerosis (20).
Many of the effects of calcitriol are reproduced by its predecessor metabolite 25(OH)D, which is also a substrate for lα-hydroxylase, and other metabolites. The activity of 25OHD3 is 1000 times less than 1,25(OH)2D3, but it has effects similar to calcitriol, since its concentration in serum is 1000 times higher (30 μg/l), compensating to a certain extent for the low affinity of 25(OH)D3 to VDR.
The level of 25(OH)D3 in the blood is considered an indicator of vitamin D reserves in the body. In elderly healthy people, the level of 25(OH)D33 is not only in elderly people prone to developing vitamin D deficiency, but also in patients on chronic hemodialysis (21). In the latter, low values of 25(OH)D3 are often combined with radiological and morphological signs of osteomalacia, regardless of the level of calcitriol, while in adynamic skeletal disease high values of 25(OH)D3 are found (22).
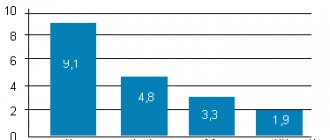
In the general population, provision of VD is associated with a decrease in overall and cardiovascular mortality (23). A similar pattern is observed in patients with CKD. A number of studies conducted in recent years have shown that the survival rate of patients with stage III-V CKD who received calcitriol is higher
,
and overall mortality and mortality from cardiovascular complications is lower than in patients not treated with VD metabolites (24, 25), and small doses of the drug virtually eliminate the risks of deterioration in renal function and transfer of patients to RRT.
A well-known historical cohort study (26) showed that the 2-year survival rate of 37,173 hemodialysis patients treated with injectable forms of VD metabolites was 26% higher than that of 13,864 patients not treated with VD metabolites. According to M. Naves-Diaz et al. (27), with oral administration of VD metabolites, the mortality of patients on chronic hemodialysis (n = 7203) from cardiovascular and infectious complications and tumor diseases was significantly lower than in 8801 patients who did not receive metabolites, and the greatest effect was achieved when prescribing metabolites in small doses. Small doses of drugs have less effect on serum calcium and phosphorus levels. According to G. Block et al. (28) and S. Ganesh (29), both high and low serum levels of these minerals increase the morbidity and mortality of hemodialysis patients. The beneficial effect on the survival of patients on hemodialysis of paricalcitol and doxecalciferol is even higher than that of calcitriol, however, judgments about the improvement in the survival of patients with chronic renal failure when treated with VD metabolites are not shared by all authors (30).
Currently, the main indication for calcitriol is high PTH levels in patients on RRT and with predialysis chronic renal failure. At the same time, the presence of VDR in most body tissues and the ability of VD and its metabolites (calcidiol and calcitriol) to influence many biological processes (inflammation, cell differentiation, cytokine production, etc.) indicate the organoprotective properties of D-hormone, including nephroprotection .
This phenomenon is based on the ability of VD to inhibit RAS activity, prevent glomerular hypertrophy in rats with subtotal nephrectomy, and reduce albuminuria and mesangial cell proliferation. In experimental animals, calcitriol administration preserved podocytes (31). In humans, calcitriol reduces proteinuria and protein excretion-related mesangial inflammation, and modulates the immune response (32). At the same time, there is a decrease in the production of tumor necrosis factor-α and other cytokines. In mice with lupus nephritis, calcitriol administration reduced the titer of anti-DNA antibodies. Other VD metabolites, in particular paricalcitol, have similar antiproteinuric and immunomodulatory effects (33).
In renal transplant recipients, the immunosuppressive effects of calcitriol, commonly prescribed for osteoporosis, are less clear and most studies are retrospective in nature (34).
Calcitriol under the brand name Rocaltrol is supplied by the Swiss company in capsules of 0.25 mcg for oral administration. The drug is on the DLO list and patients in need receive it free of charge. Currently, several more VD metabolites or, as they prefer to be called, VDR activators, Paricalcitol and Doxecalciferol, are registered in Russia, the effectiveness of which in a number of aspects exceeds the effectiveness of Rocaltrol, but they are not included in the DLO lists.