- Description of the pathology
- Classification and types
- Causes
- Symptoms
- Complications
- Diagnostics
- Treatment
- Prevention
The pancreas is located behind the stomach, its duct opens into the duodenum. Pancreatitis is a disease caused by an inflammatory process in the tissues of this organ.
Disease history
A separate section of gastroenterology—pancreatology—is devoted to the study of pancreatitis. The first mention of the pancreas is contained in the works of Aristotle, but a detailed study of the pathological processes associated with this organ was not carried out at that time. The study of the physiology of this part of the digestive system is complicated by its specific location in the body. Significant advances in research occurred at the turn of the nineteenth and twentieth centuries.
The first full-fledged studies were carried out by:
- R.Friz (1889);
- H.Chairi (1886);
- I.L. Dolinsky (1894).
The incidence of chronic pancreatitis increases every year. The risk group began to include men 40-55 years old and children 10-14 years old. Research into the pancreas and pathologies associated with its development continues. Experts are inventing not only new methods for studying patients, but also treatment options for the inflammatory process.
Types of chronic pancreatitis
By origin, chronic pancreatitis can be primary or secondary. In the first case, the disease develops against the background of damage to the gland by a specific factor (alcohol, toxins). In the second, the disease is a complication of other pathological processes (for example, disturbances in the functioning of the digestive organs). According to the severity of the course, CP can be mild, moderate or severe. Chronic pancreatitis always develops with periods of remission and exacerbation.
Features of HP of different forms:
The disease is a serious problem, so the slightest suspicion of pancreatitis should be a reason to consult a doctor.
- with a mild course, exacerbations occur once or twice a year (there are no disturbances in the exocrine function of the glands, pain is easily relieved with antispasmodics and analgesics, other signs of CP do not appear);
- with moderate severity, exacerbations become more frequent up to three or four times a year (the exocrine function of the gland is impaired, pain symptoms are more pronounced, the patient may experience a decrease in appetite, weight loss, tests confirm the inflammatory process);
- in severe cases, exacerbations occur on average five or six times a year (the pain syndrome is pronounced, difficult to relieve, body weight decreases to critical levels, diarrhea becomes regular, the clinical picture of the patient’s health is supplemented by most of the symptoms characteristic of CP).
Classification
Additional classification of CP is carried out according to the morphological and clinical picture, as well as clinical manifestations. Determining the specific type of chronic pancreatitis is necessary to prescribe the most effective treatment and make prognoses for the patient.
It is difficult to independently diagnose the form of the disease due to a number of similar symptoms.
Classification:
- according to the morphological picture (obstructive, fibrosclerotic, inflammatory, calcifying);
- according to clinical manifestations (latent, mixed, recurrent, permanent, pseudotumorous);
- according to the functional picture (hypoenzyme, hyperenzyme);
- by the nature of functional deviations (obstructive, hyposecretory, hypersecretory, ductular);
- a separate category includes pancreatic diabetes mellitus (hypoinsulinism, hyperinsulinism).
1) Healthy pancreas. 2) Inflammation of the pancreas.
Causes
The disease occurs under the influence of such factors:
- in 60% of cases, the cause of pancreatitis is alcohol consumption; however, the disease develops only in 5–7% of drinkers, which is due to a genetic predisposition to it;
- cholelithiasis, chronic cholecystitis and other conditions accompanied by stagnation of bile;
- cicatricial deformation of the duodenum, tumor of the papilla of Vater, that is, mechanical obstacles to the release of pancreatic juice into the intestine;
- cystic fibrosis is a genetic disease with a violation of the secretory activity of the glands, accompanied by damage to the respiratory system;
- lipid metabolism disorders, manifested by repeated episodes of acute inflammation;
- autoimmune diseases (primary pancreatic disease, Sjogren's syndrome, primary biliary cirrhosis, sclerosing cholangitis);
- some medications - azathioprine, furosemide, tetracyclines, estrogen preparations, prednisolone, metronidazole and others.
Pancreatitis in children is often associated with pathology of the structure of the biliary tract and pancreas, both congenital and acquired (opisthorchiasis). Often the cause of illness in a child is blunt trauma to the abdomen. Infections play a certain role - herpes, mononucleosis, mumps, salmonellosis.
Causes of the disease
CP is one of the common consequences of gallstone disease and excessive consumption of alcoholic beverages. These factors can disrupt the functioning of the digestive organs in a short period of time (especially in the absence of timely treatment).
With cholelithiasis, the infection enters the gland tissue through the lymphatic system, with bile or through the bile ducts. Alcohol is highly toxic to the pancreatic parenchyma.
Other causes of HP:
- cystic fibrosis;
- genetic predisposition;
- peptic ulcer and its complications;
- autoimmune disorders;
- increased level of calcium ions in the blood;
- uncontrolled use of medications;
- consequences of helminthic lesions of the digestive system;
- complications of atherosclerotic diseases;
- intoxication with harmful substances (ammonia, arsenic);
- complications of pancreatitis of unknown etiology.
Description of the pathology
The pancreas has two main functions:
- the production of digestive enzymes, which enter the duodenum through the ducts, where they are activated and participate in the breakdown of proteins and fats;
- secretion of hormones - insulin and glucagon, which are released into the blood and regulate glucose levels.
If the patency of the ducts is disrupted for any reason, the pressure of pancreatic juice in them increases. Damage to gland cells occurs. In acute pancreatitis, the mechanism of “self-digestion” of tissues is triggered. The result of chronic inflammation is a constant deficiency of digestive enzymes, replacement of glandular cells with connective tissue, with a subsequent weakening of not only exocrine function, but also the production of hormones.
Symptoms
The first changes in the functional state of the pancreas develop asymptomatically. Disturbances in the functioning of the digestive system are minor and mildly expressed (mild pain that quickly resolves on their own, changes in stool consistency).
From the moment of the first exacerbation of the inflammatory process, the symptoms intensify and are accompanied by painful attacks. The pain may be constant or intermittent.
Symptoms of HP:
Signs of exacerbation of chronic pancreatitis: paroxysmal pain;- girdle pain;
- pain in the left hypochondrium;
- constant pain in the epigastric zone;
- pain on palpation of the abdomen;
- alternating diarrhea with constipation;
- frequent and debilitating vomiting;
- regular feeling of nausea;
- yellowness of the sclera;
- pallor of the skin.
Diagnosis
When the first signs of reactive pancreatitis appear, a series of clinical and biochemical tests are performed. This type of disease is quite difficult to diagnose. In order to detect reactive pancreatitis, a set of procedures is carried out and some tests are collected, namely:
- General urine analysis;
- X-ray of the abdominal cavity;
- Ultrasound of the abdominal cavity (it will show all the processes that occur in the peritoneum);
- MRI;
- Blood analysis;
- Gastroscopy (will show all existing inflammations and their severity).
With the help of these tests, the doctor will be able to fully familiarize himself with the existing pathology.
Diagnostic examination
A gastroenterologist diagnoses chronic pancreatitis. After the initial examination, the patient is prescribed laboratory and instrumental examination methods. Deviations in test results will indicate the presence of an inflammatory process. Instrumental techniques will allow you to study the general condition of the pancreas and the digestive system as a whole.
In some cases, patients are recommended to undergo additional examination by specialized specialists.
Laboratory diagnostics
The purpose of laboratory diagnostics is to determine the general health of the patient and identify the inflammatory process. The progression of CP is indicated by increased activity of amylase and lipase, trypsin, elastase and excess fat. Some indicators make it possible to determine enzyme insufficiency of the pancreas before conducting an instrumental examination.
Laboratory diagnostic methods:
- general blood and urine analysis;
- blood biochemistry;
- coprogram;
- stool examination;
- radioimmunoassay.
Instrumental diagnostics
Instrumental diagnostics make it possible to accurately determine the nature of the inflammatory process, the extent of its spread and draw up a clinical picture of the disease. In some cases, several procedures (ultrasound, CT) are performed to confirm the diagnosis. If the process of identifying pathology is complicated by additional factors, then the list of necessary procedures expands.
Instrumental diagnostics:
- Ultrasound of the abdominal organs;
- endoscopic ultrasonography;
- CT or MRI of the pancreas;
- X-ray examination;
- tests with stimulants of secretion or enzyme activity;
- retrograde cholangiopancreatography.
Differential diagnosis
The symptoms of chronic pancreatitis may resemble other pathologies. Differential diagnosis of the inflammatory process should be carried out with a perforated ulcer, intestinal obstruction, acute appendicitis and cholecystitis, as well as intestinal vein thrombosis. In some cases, the manifestations of CP resemble myocardial infarction. This pathology should also be excluded when examining the patient.
Symptoms
The clinical picture appears within 2-3 hours after exposure to the provoking factor. Symptoms of this disease include such manifestations as:
- Pain that gets worse when eating. But it is not as strong as with other pancreatic diseases;
- The pain may be accompanied by vomiting. In the vomit, you can notice impurities of bile or mucus. It is mainly localized in the upper abdomen with transition to the hypochondrium.
- The person shows signs of intoxication, blood pressure drops, and body temperature rises.
- Children have approximately the same symptoms. But in addition to the symptoms described, the baby may also experience stool upset. The baby's stool turns yellow and mucus appears. Sometimes he is constipated. In addition, his urine becomes dark and his skin takes on a yellowish tint. An infant may suddenly begin to cry.
Complication of the disease
Complications of CP are divided into early and systemic. Pancreatitis provokes a violation of the outflow of bile, which can result in obstructive jaundice. Even in the early stages of development, the inflammatory process can cause internal bleeding, infectious complications, abscesses, damage to the biliary tract or phlegmon of the retroperitoneal tissue. These conditions are life-threatening and, in the absence of adequate treatment, pose a threat to life.
Disease progression
CP is a progressive disease. The inflammatory process disrupts the intrasecretory and exocrine functions of the pancreas. The course of the disease has a long-term relapsing nature. In severe cases, a change in the cellular structure of the gland occurs and its functional failure develops.
It is not recommended to self-medicate, because the sooner you visit a specialist, the sooner a serious problem with the pancreas can be identified. Systemic complications:
- encephalopathy;
- functional failure of the lungs, liver and kidneys;
- diabetes;
- malignant formations;
- esophageal bleeding;
- critical loss of body weight;
- death.
Complications
Pancreatitis may be accompanied by the following complications:
- stagnation of bile with the appearance of pain in the right hypochondrium, nausea, bitterness in the mouth, formation of gallstones;
- infectious diseases - purulent inflammation of the bile ducts, peritonitis, sepsis;
- the formation of large cavities in the pancreatic tissue;
- bleeding caused by damage to the esophagus, gastric or duodenal ulcer;
- thrombosis of the veins of the liver and spleen;
- pleurisy - accumulation of fluid in the cavity around the lungs, ascites - effusion in the abdominal cavity;
- compression or narrowing of the lumen of the duodenum, deterioration of its patency;
- hypoglycemic crisis - a condition caused by a lack of glucagon, manifested by severe weakness, muscle tremors, sweating, palpitations, impaired consciousness;
- pancreas cancer.
Treatment
The goal of therapy for chronic pancreatitis is to relieve pain symptoms, maximize the period of remission, and improve the functional parameters of the pancreas. In the absence of effectiveness of conservative and drug treatment, the only way to alleviate the patient’s condition may be surgical intervention. The scale of the operation depends on the stage of development of the inflammatory process and the degree of damage to the digestive system.
Treatment regimen
The treatment regimen for chronic pancreatitis is drawn up individually. Mandatory stages of therapy are taking medications and diet therapy. If treatment occurs using surgical techniques, then the patient’s tendency to recovery will depend on proper rehabilitation.
Rehabilitation therapy is not inferior in importance to basic medical methods.
Approximate treatment plan:
- diet therapy (table No. 5b);
- symptomatic therapy;
- detoxification procedures;
- relief of the inflammatory process;
- restoration of digestive function;
- replacement of pancreatic enzymes;
- surgical intervention (if indicated);
- maintenance and rehabilitation therapy;
- prevention of complications of the inflammatory process;
- regular examination by a gastroenterologist.
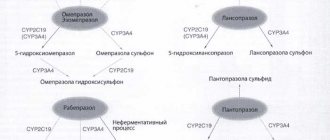
Drug treatment
Medicines for the treatment of CP are selected taking into account the individual clinical picture of the patient’s health status. Some of the drugs are recommended for long-term course use. The drug therapy schedule should not be violated. If treatment for CP is stopped earlier than recommended, the period of remission may be shortened.
Examples of medicines:
- enzyme-containing drugs (Pancreatin, Creon);
- analgesics for pain relief (Papaverine, No-Shpa);
- antacids (Maalox, Almagel);
- proton pump inhibitors (Rabeprazole);
- drugs from the group of prokinetics (Cerucal, Motilium);
- anti-inflammatory drugs (Diclofenac);
- drugs to reduce gland secretion (Sandostatin);
- antisecretory drugs (Omeprazole).
Surgery
For patients with CP, surgical treatment is prescribed in rare cases. The main methods of treating pathology of this type are medication and diet therapy. The need for surgery arises when there is no tendency to recovery or serious complications occur. In some cases, emergency surgical procedures are performed to save the patient's life.
Surgical procedure options:
- sanitation and opening of purulent foci (phlegmon, abscesses);
- sphincterotomy (for sphincter blockage);
- pancrectomy (the operation can be complete or partial);
- removal of the gallbladder (if indicated);
- removal of stones from the pancreatic ducts;
- partial gastrectomy;
- creation of circumferential bile outflows (to relieve the load on the pancreatic ducts).
Diet
Diet therapy is one of the main methods of treating CP. If you allow errors in nutrition at any stage of treatment of the inflammatory process, then the tendency to recovery will be significantly reduced. In addition, taking prohibited foods will provoke an attack of pancreatitis. Fried, spicy, salty, fatty foods, marinades, some vegetables (radish, radish), mushrooms, sour fruits and alcoholic drinks should be excluded from the diet.
Vegetables that are strictly prohibited for pancreatitis.
Allowed to include in the diet:
- lean meats and poultry;
- boiled pureed vegetables;
- steam omelettes;
- vegetarian soups;
- pasta;
- porridge with water or milk;
- fruits with low acidity levels;
- low-fat dairy products;
- low-fat fish (boiled).
When preparing dishes, it is recommended to give preference to the methods of steaming, boiling or stewing. Meals are taken up to six times a day (in small portions). It is important to avoid overeating and starvation. As an addition to diet therapy, you can use medicinal mineral waters (alkaline types of Essentuki, Borjomi).
Sample menu
| Breakfast | Steam omelette, tea or dried fruit compote, oatmeal with blueberries |
| Lunch | Banana (or fruit salad), glass of low-fat yogurt |
| Dinner | Vegetarian soup, boiled turkey with carrots, reduced fat cheese, apple juice |
| Afternoon snack | Baked apple, low-fat cottage cheese |
| Dinner | Rice with lean fish, boiled carrots, whole grain bun, dried fruit compote or tea |
| Before bedtime | Three wheat-oat bread, a glass of skim milk |
How to help yourself during an attack of pancreatitis?
If the diagnosis of chronic pancreatitis is confirmed and the patient is able to independently determine the attack, then several recommendations can be used to alleviate the condition. At the first manifestation of CP or too severe pain symptoms, only a qualified specialist can provide proper assistance (you should consult a doctor or call an ambulance).
Algorithm of actions:
- elimination of pain (Paracetamol);
- relief of spasm (Drotaverine, No-Shpa);
- decreased acidity of gastric juice (Omeprazole, Maalox, Phosphalugel);
- decreased pancreatic secretion (Creon, Mezim);
- hunger, cold and rest (you cannot eat food during the day, you can apply a cold compress to the painful area, any stress on the body is excluded).
Consequences
Without adequate treatment, the disease can cause irreversible changes in tissues. Ignoring the disease, lack of diet and treatment can lead to complications such as pancreatic necrosis. This process cannot be stopped. In addition, conditions such as:
- Formation of ulcers;
- Internal bleeding;
- Formation of fistulas in the digestive organs;
- Death of stomach and pancreas tissue;
- Pancreatic shock.
Prevention
Primary prevention of CP includes standard rules of a balanced diet, a healthy lifestyle and giving up bad habits. If the disease is detected, then after the course of therapy it is necessary to follow all the doctor’s recommendations. Errors in nutrition, excessive physical activity, alcohol and other negative factors will shorten the period of remission and increase the intensity of symptoms of attacks.
Prevention measures:
- quitting smoking and alcohol abuse;
- compliance with the drinking regime (at least one and a half to two liters of water per day);
- limiting the amount of fatty, fried, salty foods in the diet (spicy foods, marinades, spices and seasonings);
- compliance with the rules of a healthy diet (sufficient content of healthy elements and vitamins in the menu);
- balanced diet with the exception of overeating.
Forecast
In CP, the mortality rate reaches 50%. In most cases, the cause of death in patients is complications of the inflammatory process. The development of the disease can be asymptomatic for a long time, but the progression of the pathology does not stop without adequate therapy. In case of CP, the patient should be regularly examined by a gastroenterologist (at least once every six months).
Timely therapy provides:
- persistent and long-term remissions;
- slowing down the inflammatory process;
- reduction of pain symptoms during exacerbation attacks.
Video on the topic: Chronic pancreatitis. What are the symptoms? How to treat? What can and cannot be eaten?