Quick transition Treatment of laryngopharyngeal reflux
Laryngopharyngeal reflux (LPR) is the reflux of gastric contents (acid and enzymes such as pepsin) into the larynx, leading to hoarseness, a feeling of a lump in the throat, difficulty swallowing, coughing, and a feeling of mucus in the laryngopharynx.
Reflux as a cause of the above symptoms without gastroesophageal reflux disease (GERD) is constantly being questioned. Guidelines issued by specialist societies in the field of laryngology and gastroenterology present different points of view. Both groups acknowledge that interpretation of existing studies is complicated by vague diagnostic criteria for LPR, variable treatment response rates, and large placebo effects in treatments.
There are relatively limited data on the prevalence of LPR: approximately 30% of healthy people may have episodes of reflux on 24-hour pH measurements or show characteristic changes in the larynx.
LPR can directly or indirectly cause laryngeal symptoms. The direct mechanism involves irritation of the mucous membrane of the larynx with caustic substances - refluxates (acid, pepsin). The indirect mechanism involves irritation of the esophagus, leading to laryngeal reflexes and symptoms.
Helicobacter pylori infection may also contribute. The prevalence of H. pylori among patients with LPR is about 44%.
Laryngophangeal reflux and GERD
Although stomach acid is common to both LPR and GERD, many differences exist, making LPR a distinct clinical entity.
- A prerequisite for GERD is heartburn, which is reliably observed only in 40% of patients with LPR.
- Most patients with GERD have evidence of esophagitis on biopsy, while patients with LPR have evidence of esophagitis in only 25% of cases.
- GERD is thought to be a problem of the lower esophageal sphincter and occurs primarily when lying down. In contrast, LPR is seen primarily as a problem of the upper esophageal sphincter, and occurs primarily in an upright position during exercise.
- To form LPR, much less acid exposure is required than with GERD.
There are significant differences between the mucous membrane of the esophagus and larynx.
- The upper limit of normal for acid reflux into the esophagus is considered to be up to 50 episodes per day, while 4 episodes of reflux into the larynx is no longer considered normal.
- In the larynx, unlike the esophagus, which eliminates acid through peristalsis, refluxate persists much longer, causing additional irritation.
- The epithelium of the larynx is thin and poorly adapted to combat caustic chemical damage from the same pepsin and acid.
Symptoms of laryngopharyngeal reflux
- Dysphonia or hoarseness;
- cough;
- feeling of a lump in the throat;
- discomfort and feeling of mucus in the throat;
- dysphagia (impaired swallowing).
Some researchers believe that chronic irritation of the larynx may lead to the development of carcinoma in patients who do not drink alcohol or smoke, although there is no data to support this.
Symptoms characteristic of LPR may also be caused by the following conditions:
- postnasal drip;
- allergic rhinitis;
- vasomotor rhinitis;
- upper respiratory tract infections;
- habitual coughing;
- use of tobacco or alcohol;
- excessive use of voice;
- changes in temperature or climate;
- emotional problems;
- environmental irritants;
- vagal neuropathy.
Methods for correcting neurotic manifestations in children
Neurotic manifestations are one of the most common disorders of the nervous system in children. The share of these disorders is 35–40% of all functional consequences of perinatal hypoxia [1–5]. The wide syndromic range and frequent recurrence of neurotic manifestations require special attention to this cohort of patients not only from neurologists, but also from pediatricians, teachers, and psychologists. In addition, such patients usually require long-term comprehensive medical and psychological support. According to the literature, over 64% of these children have more than 1 episode of exacerbation, about 42% of children have 3 or more episodes of neurotic manifestations [3, 4, 6–8]. Such statistics indicate the insufficient effectiveness of medications used to correct these disorders, which reduce the quality of life not only of the child, but also of his family [5, 6, 9–16]. Of course, dysfunction of the nervous system clinically manifests itself during important periods of a child’s life, such as primary socialization in kindergarten and the beginning of school. At this time, the body undergoes a restructuring to the conditions of the new society, and the functional failure of the nervous system does not allow one to safely pass this period [8, 17–24]. Therefore, the search for new safe and effective therapies is an important task of modern medicine. In this regard, the purpose of our study was a comparative study of the use of several drugs used to correct neurotic and emotional disorders in children.
Material and methods
We observed 131 patients (72 (54.9%) boys and 59 girls (45.1%)) with neurotic manifestations aged from 3 to 12 years. During the diagnosis, a clinical assessment of the neurological and somatic status, neuroimaging (MRI of the brain), electroencephalography, transcranial Dopplerography of cerebral vessels, assessment of the emotional and psychological state using the Luscher test and the CMAS anxiety scale (for children over 8 years of age - The Children's Form)
of Manifest Anxiety Scale modified by A.M. Prikhozhan 2002) [9, 10, 25, 26]. Biochemical and clinical blood tests were performed. All children were examined by a speech therapist-psychologist, ophthalmologist, and pediatrician. Using a random sampling method, patients were divided into 3 groups: the 1st (44 children) received correction with the drug Phenibut at a dose of 0.25 to 0.5 g/day, the 2nd (44 children) - with the drug Nervohel (“Heel”, Germany), 3rd (43 children) – with the drug Valerianahel (“Heel”). The initial data in each group were taken into account differentially. The drug phenibut (Olainfarm, Latvia) consists of two active substances: aminophenylbutyric acid (a phenylethylamine derivative with a tranquilizing effect) and gamma-aminobutyric acid (GABA) (with a nootropic effect). Excipients include: lactose, potato starch, low molecular weight polyvinylpyrrolidone, calcium stearic. The dose ranged from 0.25 to 0.5 g/day. The homeopathic drug Nervohel (Heel, Germany) consists of 6 components (Table 1), each of which has a specific effect on the body. The drug is used from the age of 3 for the treatment of neurotic disorders of various types. We prescribed to our patients, depending on age, from 1 to 3 tablets/day for 14 days without meals.
The drug Valerianahel (Biologische Heilmittel Heel, Germany), like Nervohel, has a mixed composition (Table 2), which causes a versatile effect not only on the nervous system, but also on the body as a whole. Dose for children from 2 to 6 years old - 5 drops 2-3 times / day, from 6 to 12 years - 10 drops 3 times / day for 2 weeks.
In all groups, children received medications according to age recommendations. The effectiveness was assessed using a control clinical examination, extra- and intracranial Doppler examination of cerebral vessels, EEG, testing using the Luscher and CMAS methods before and after therapy. Statistical processing of the study results was performed using the Statistica 22.0 software package (StatSoft Inc., USA), differences were considered statistically significant at p≤0.05.
Results and discussion
The nosological structure of the pathology in 131 patients was represented by the following functional disorders of the nervous system (Table 3): 39 children (29.8%) had disorders of the emotional sphere, 92 (70.2%) had various types of disorders of a neurotic nature. It should be noted that basically these manifestations debuted at the age of 2.5–3.5 years, when children underwent primary social adaptation (kindergartens, development groups, etc.).
A comprehensive diagnosis of all children with NES and NP showed that the greatest disturbances were observed during transcranial Doppler sonography, which characterizes the blood supply to the brain. All patients demonstrated various changes in blood flow through the great vessels and vertebral artery and into the venous outflow. There was a significant decrease in blood flow in the anterior and middle cerebral artery by 32±3.7 and 28±2.4% (p≤0.05 compared to the norm), impaired venous outflow by 38±4.6% (p≤0. 03), aggravated by loads on average 1.4 times compared to the initial values. All patients had insufficiency of the regulatory function of the autonomic nervous system of a mixed type (68.9%) or with the dominance of sympathicotonia (31.1%) with signs of tension in adaptation processes. In 31% of children, neuroimaging changes were detected in the form of mild residual ventriculomegaly. According to EEG data, 73.5% of patients showed disorganization of the bioelectrical activity of the brain in the form of irregularity of the basic rhythm, dysfunction of the median structures, and in 16.1% of them - paroxysmal activity. According to laboratory data, clinical and biochemical blood tests did not reveal any significant differences from the age norm. According to the Luscher color test, disturbances in the emotional, communicative and volitional spheres were noted. By sequential preferential color selection, the following disorders were verified in the observed patients (Fig. 1): in 32% - changes in emotional balance (although clinical changes were noted in 29.9%), in 27% - impaired motivation, in 43% - communication problems , sleep or falling asleep problems (54%), 81% had phobias and anxiety. When analyzing anxiety (according to the CMAS scale from 8 years old) during testing on 53 points, 3 levels of anxiety were identified: slightly increased (41%), clearly increased (36%) and very high (23%).
According to Doppler ultrasound after 2 weeks. after therapy, patients in group 1 receiving phenibut showed positive dynamics in the form of improved venous outflow in 34% and improvement in autonomic support in 36.3%, with a trend toward normalization. No reliable changes in blood flow velocity in the great vessels were obtained. In group 2 (Nervohel), a positive effect was observed in 16 (37.2%) patients in the form of a decrease in functional spasm in the vertebral artery and an improvement in venous outflow, which clinically neutralized tension cephalalgia in children. No significant changes in autonomic regulation were obtained. In group 3 (Valerianahel), an improvement in blood flow velocity in the great vessels was recorded in 19% and normalization of autonomic support in 25.6% of patients. Patients of all groups did not demonstrate significant changes in the EEG, however, on average, 1/3 of patients (36.3% in the 1st, 41% in the 2nd and 30.2% in the 3rd) showed positive changes in the form reducing irritation of cortical-subcortical structures. Positive changes were noted in the reduction of neurotic conditions (Fig. 2, Table 4) and emotional disorders in group 1 (phenibut) in the form of leveling anxiety and phobias in 38.6% of patients, improving sleep in 52.3%. Also, 20.5% of children in this group had improved communication skills, and 38.6% showed a tendency towards normalization of the emotional sphere.
Patients of groups 2 and 3 showed the following results: in 41.9% of children taking Nervohel, anxiety and phobic manifestations decreased, in 25.5% communication skills improved, and in 46.5% their emotional background improved. Among children receiving Valerianahel, anxiety-phobic disorders were leveled out in 34%, sleep disorders in 45.4%, communication skills improved in 18.2%, and emotional background in 23% of patients. The onset of the effect was recorded on days 5–7 of therapy in group 1, from days 4–5 and days 3–4 in groups 2 and 3, respectively. After 2 weeks After therapy, patients showed almost the same results; there was a significant difference between the indicators immediately after treatment and after 2 weeks. after that it was not received. Thus, the effectiveness of homeopathic drugs used to treat neurotic manifestations and emotional disorders is practically no different from the effectiveness of the allopathic drug phenibut (Table 4). Each of the drugs had “its own point of application,” which was most likely due to their composition and mechanism of action. In the correction of sleep disorders, all drugs showed almost identical effectiveness, which made it possible to normalize the process of falling asleep and staying asleep in 44.2–52.3% of children. Nervochel demonstrated the greatest effectiveness in influencing the emotional sphere, as well as in increasing motivation (like phenibut) and communication. Good tolerability of complex homeopathic preparations was also noted - only 2 patients experienced allergic manifestations while taking Nervohel and Valerianachel, which were regarded as a homeopathic “exacerbation”, since they were leveled out independently. In addition to improving the neurological status, 18.6% of patients taking Nervohel and 20.5% taking Valerianachel showed a reduction in dysfunctions in the gastrointestinal tract and urinary system.
Conclusion
Correction of changes of an emotional and neurotic nature requires active and, often, long-term medical intervention. The range of drugs used in the treatment of these disorders is quite wide, but many of them have serious side effects. This fact certainly motivates pediatricians to search for new safe drugs. After the official recognition of homeopathic methods of treatment and permission for their use in traditional medical practice (orders of the Ministry of Health of the Russian Federation No. 115 of July 1, 1991 “On the development of homeopathic methods in medical practice” and No. 335 of November 29, 1995 “On the use of the homeopathy method in practical healthcare"), a huge interest in homeopathy arose in various fields of medicine, especially in pediatrics. A verified clinical, paraclinical and neuropsychological study showed the effectiveness and safety of the use of homeopathic medicines in the treatment of emotional and neurotic disorders in children. Thus, it was found that emotional disturbances are more effectively corrected with Nervohel, and phenibut better eliminates sleep disturbances. When using valerianahel, good results were also observed; it was slightly inferior to the above drugs. It should be noted that Valerianahel helped improve blood flow through the great vessels, which makes it possible to recommend it to children with cerebrovascular distension. In addition to the positive effect on the nervous system, these homeopathic medicines eliminate the manifestations of autonomic dysfunction of the gastrointestinal tract and urinary system. Thus, Nervohel and Valerianahel are effective and safe drugs for the correction of neurotic disorders and changes in the emotional sphere in children, which allows them to be recommended for widespread use in practical healthcare.
Diagnostics
There is considerable controversy regarding the appropriate way to diagnose LPR.
Most patients are diagnosed clinically, based on symptoms associated with LPR.
During laryngoscopy (examination of the larynx), swelling and hyperemia (redness) of varying degrees are noted. However, the relatively weak correlation between symptoms and endoscopic findings argues against the use of endoscopic diagnostic methods.
The Reflux Symptom Score and Reflux Symptom Index are well suited for both diagnosis and monitoring response to therapy.
Daily Ph-metry with a dual sensor probe, despite its excellent sensitivity and specificity, is questioned, since the results of this diagnostic method often do not correlate with the severity of symptoms.
Another diagnostic option may be empirical PPI therapy.
Treatment of laryngopharyngeal reflux
Lifestyle changes and diet are the main approach in the treatment of LPR and GERD. The role of drug therapy is more controversial. It is unknown whether asymptomatic patients with incidentally detected signs of LPR require treatment. There are theoretical concerns that LPR may increase the risk of malignancy, but this has not yet been proven. In any case, patients with asymptomatic LPR are advised to follow a diet.
Patients are advised to quit smoking, alcohol, and avoid foods and drinks containing caffeine, chocolate, and mint. Prohibited foods also include most fruits (especially citrus fruits), tomatoes, jams and jellies, barbecue sauces and most salad dressings, and spicy foods. Small meals are recommended.
You should avoid exercise for at least two hours after eating, and refrain from eating or drinking three hours before bedtime.
Drug therapy usually includes proton pump inhibitors (PPIs), H2 blockers, and antacids. A PPI is recommended for six months for most patients with LPR. This figure is based on the results of endoscopic studies (this is the time needed to reduce laryngeal edema), as well as the high percentage of relapse in the case of a three-month course of therapy. Discontinuation of therapy should be carried out gradually.
If therapy with PPIs and H2 blockers is unsuccessful, treatment with tricyclic antidepressants, gabapentin and pregabalin should be considered, since one of the possible mechanisms for the development of reflux is increased sensitivity of the larynx.
New in the diagnosis and treatment of AIT
Murzaeva Irina Yurievna
Endocrinologist, Preventive Medicine Doctor
December 5, 2016
Endocrinology is an ultra-modern science!! It appeared only in the 20th century. Approaches to the diagnosis and treatment of many endocrine diseases are constantly changing as new research appears on the causes of this or that pathology, people continue to study the hormonal-endocrine, and not only, secrets of their body 
In the upcoming blog topics I will present:
- new approach in the treatment of AIT
- a new look at the treatment of obesity and an updated menu
- a new look at the problem of treating type 2 diabetes mellitus and the progression of complications. The theory is based on the division of type 2 diabetes mellitus into subgroups based on the presence of an autoimmune reaction to insulin, which will make it possible to predict various options for the course of type 2 diabetes mellitus and the occurrence of complications.
But today we are talking about a mysterious autoimmune thyroiditis. Currently, there is a general increase in autoimmune diseases. But it is autoimmune diseases of the thyroid gland that stand apart from other immune pathologies. Of all thyroid pathologies, AIT accounts for 20-50% of cases. Women over 60 years of age are more often affected, especially residents of megacities.
In the clinical picture of AIT, one can distinguish complaints that increase depending on age. With them, people, as a rule, go to see a doctor: Young people with AIT typically complain of hair loss, weight gain, constipation (constipation), brittle nails, dry skin.
In middle age, complaints about symptoms of arthrosis and osteochondrosis, depression, and arterial hypertension predominate.
over 50 years, neurological and cardiovascular complaints predominate.
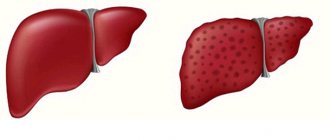
AIT (autoimmune thyroiditis) is a slow-type immuno-inflammatory process , expressed by autoaggression of immune cells to the own cells of the thyroid gland in the form of a destructive process and infiltration of gland tissue with inflammatory cells: neutrophils, macrophages, etc. with the production of antibodies to thyroglobulin and microsomal protein structures of the thyroid glands. Antibodies themselves are not capable of destroying thyroid cells and follicles. Inflammation - destruction (tissue destruction) is caused by immune cells.
There are many theories about the reasons for the appearance of AIT. Here are the main ones:
- viral, this is a provocation of the inflammatory process by Coxsackie and herpes viruses (type 6, etc.);
- genetic theory of the prerequisites for immune diseases (as well as bronchial asthma, rheumatoid arthritis, etc.);
- increased consumption of iodine in the form of medications provokes and enhances the activity of the autoimmune process in the thyroid gland. Academician of the Russian Academy of Natural Sciences Veldanova M.V. in his monograph “Lessons of Thyroidology” (a basic textbook for endocrinologists on the thyroid gland) explains the mechanisms of development of this process;
- frequent and uncontrolled use of antiviral drugs - interferon, cycloferon, amixin, monoclonal antibodies and others, contributes to the development or exacerbation of existing autoimmune diseases, including autoimmune thyroiditis. What does the leading thyroidologist in our country M.I. Balabolkin point out? in his monograph “Fundamental and Clinical Thyroidology”.
But, relatively recently, a new theory of the development of AIT has emerged.
The KNOW-HOW of the theory of 2014 (Professor, MD Rustambekova S.A.) is that one of the reasons for the development of AIT is the theory of dispolymicr(macro)elementosis.
Dyspolymicr(macro)elementosis is a violation of the homeostatic balance of the macro-microelement supply of the body, which also provokes and initiates immune inflammation, oxidative stress and other pathological processes that damage the thyroid tissue.
This theory is also confirmed by the fact that the clinical manifestations (symptoms) of autoimmune thyroiditis are not characteristic of true inflammation, which occurs when an infection enters the gland. The theory of dysmicroelemnotosis is now popular in obstetrics
(hypomagnesemia, hypocalcemia), in cardiology for a long time, for arrhythmia, rhythm disturbances.
Let me explain: for normal functioning, our body has a certain set of micro (macro) elements: macroelements are potassium, calcium, magnesium, etc. Microelements: selenium, zinc, iodine, iron, etc. If we recall our school-student knowledge, these micro (macro) elements are present in all cells of the body - they participate in all metabolic processes and are part of many enzymes in the body, including those involved in the formation of thyroid hormones and immune cells. An excess or deficiency of some micro (macro) elements is deadly, for example, hyperkalemia (excess potassium, due to renal failure, causes life-threatening arrhythmias). Other micro(macro)elementoses are not so dangerous, but they disrupt the functioning of many organs, in our case the thyroid gland. As a result of many years of research, Moscow scientists came to the conclusion that the thyroid gland needs not only the popularized iodine, but also selenium, zinc, magnesium, and other equally important trace elements. And the emissions released into the atmosphere as a result of the work of industrial enterprises, transport, and for other reasons greatly interfere with the functioning of the thyroid gland: cadmium and lead! The environmental situation in the city or region where a person lives, as it turns out, directly affects the development of AIT, due to an excess of toxic elements: lead, cadmium, aluminum, mercury, etc. in the air, water, soil. That is why AIT is now called an environmentally dependent disease. Cadmium, for example, is a direct antagonist of beneficial selenium and zinc. Therefore, to develop the correct treatment tactics for AIT, it is necessary to donate the micro(macro)element composition of blood or hair, which must include: iodine, calcium, iron, phosphorus, potassium, magnesium, selenium, zinc, copper, manganese, cadmium, lead and mercury. Based on this analysis, it is decided how to correctly adjust the existing changes. This is an individualized approach to patient treatment. If there is a dysfunction of the gland: hypo- or hyperthyroidism, they are subject to adjustment with standard medications taken for this purpose - Thyrozol (Mercazolil) or L-thyroxine (Eutirox).
In a monographic study of dysmicroelementosis, prof. Rustambekova S.A. It is shown in clinical examples that correction of macro(micro)elemental dysfunction of the body leads to:
- to a decrease in the titer of antibodies to TPO and TG
- reducing the inflammatory process
- disappearance of nodes, or rather, pseudonodes against the background of AIT
- faster normalization of TSH and free T4 levels
- disappearance of symptoms characteristic of hypothyroidism, which is not always compensated even by taking L-thyroxine
- faster reduction of puffiness - swelling of the face, dry skin, weakness and other symptoms.
But for sufficient effectiveness, the course of treatment with micro-macroelements should not be less than 3 months.
The most effective drugs are:
- selenium preparations (doses in the first months of treatment of at least 200 mcg), - magnesium preparations (possible without B6, if you are allergic to B vitamins), - zinc preparations,
- Iodine preparations! very strictly according to need! and etc.
And this approach justifies itself, and in some cases, I think, it can help long-term remission of AIT (without hormonal treatment) or cure in its initial stages of the disease.
The material was prepared on the basis of the monograph by S. Rustambekova. Microelementoses in diseases of the thyroid gland, 2014. From Lap Lambert AP Germany.