Primary biliary cirrhosis is a destructive and inflammatory liver disease characterized by a chronic course. It is accompanied by damage to the intrahepatic ducts. As such cirrhosis progresses, ductopenia (disappearing bile duct syndrome) and persistent cholestasis (decreased bile flow into the duodenum due to disturbances in its production, excretion and/or excretion) may develop. In the terminal stage of the disease, liver failure is usually observed.
general description
Biliary cirrhosis is
a chronic autoimmune disease that occurs as a result of a violation of the outflow of bile through the intrahepatic and biliary tract (cholestasis) and is characterized by the replacement of parenchymal liver tissue with connective tissue (fibrosis). The prognosis of the disease itself depends on diagnosis and in undiagnosed cases leads to deterioration of development: progressive destruction of the parenchyma with the formation of foci of fibrosis, which results in liver cirrhosis and liver failure.
According to statistics, in economically developed countries, biliary cirrhosis is diagnosed in people aged 30 to 55 years, more often in men. The ratio of incidence among men to women is approximately 3 to 1.
Publications in the media
PRIMARY BILIARY CIRRHOSIS
- chronic non-purulent destructive cholangitis of small and medium-sized intrahepatic bile ducts, leading to their destruction and the development of liver cirrhosis.
Frequency • The disease is observed everywhere, the prevalence varies in different countries (in Europe - from 2 to 24 cases per 100,000 population) • Women make up up to 75–90% of cases • The predominant age is 35–60 years.
Genetic aspects . Occurs as a result of deficiency of dihydrolipoamide acetyltransferase (109720, [EC 2.3.1.12, B]).
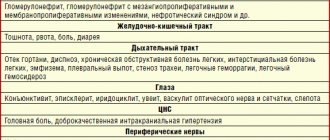
Etiology and pathogenesis are not fully understood • Impaired immunoregulation with loss of immune tolerance to tissues (bile ducts) • High titer of autoantibodies in the blood serum, primarily antimitochondrial autoantibodies • Destruction of small and medium-sized intrahepatic bile ducts leads to the development of cholestasis, regeneration of damaged bile ducts ducts are defective • Toxic components that are usually excreted into bile (bile acids, copper, etc.) are retained in the liver and cause secondary damage to hepatocytes.
Pathomorphology • Destruction of the bile ducts • Lymphomonocytic inflammatory infiltration around the damaged ducts, formation of granulomas • Proliferation of the bile ducts • Fibrosis in the portal zone and beyond • Biliary cirrhosis.
Clinical manifestations • Possible asymptomatic course until the death of the patient • The disease begins with skin itching, usually without jaundice • Jaundice develops 6–24 months after the onset of itching • Pain in the right upper quadrant of the abdomen, which may subsequently disappear • Enlarged liver • Increased fatigue • Skin hyperpigmentation is possible • In the later stages of the disease, osteoporosis, xanthomas, duodenal ulcers, signs of liver cirrhosis and its complications (bleeding from esophageal varices) are observed.
Laboratory tests • Significant increase in the activity of alkaline phosphatase and g-glutamyl transpetidase in the blood serum • Not a constant increase in the concentration of cholesterol in the blood serum, the concentration of direct bilirubin at the onset of the disease does not exceed 35 µmol/l • Increase in the concentration of IgM in the blood serum • Titer of antimitochondrial autoantibodies 1: 40 or more.
Instrumental studies • Liver biopsy • In atypical cases (disease in a man, absence of antimitochondrial autoantibodies, severe abdominal pain, uninformative liver biopsy), the bile ducts are examined using endoscopic or percutaneous cholangiography.
Differential diagnosis • Primary sclerosing cholangitis • Cholestatic variant of sarcoidosis • Autoimmune cholangiopathy • Cholestatic reaction to drugs.
Concomitant diseases • A combination of primary biliary cirrhosis with almost all autoimmune diseases has been described • Often combined with rheumatoid arthritis, scleroderma, CREST syndrome, Sjogren's syndrome, autoimmune thyroiditis, etc. • The risk of developing breast cancer in patients is 4.4 times higher than in the general population.
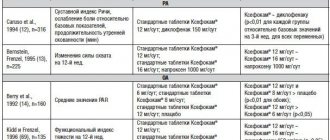
Treatment • Symptomatic treatment of cholestasis (see Primary sclerosing cholangitis) • Taking ursodeoxycholic acid 13–15 mg/kg 2 times a day significantly, although to a small extent, increases the life expectancy of patients and allows delaying liver transplantation • The effectiveness of GCs, cytostatics, colchicine is minimal, and given this, as well as severe side effects, it is not recommended to prescribe these drugs • Since there is a threat of bleeding from varices of the esophagus even before the development of cirrhosis, it is necessary to promptly consider the issue of portacaval shunting, which in patients with primary biliary cirrhosis has positive effect • It is not recommended to remove gallstones if they are not located in the common bile duct, because patients do not tolerate surgery well • Liver transplantation is more successful if it is performed in the early stages of the disease •• Patients should be referred to a transplant center when the serum bilirubin concentration is 150 µmol/l •• Five-year survival rate is 60–70% •• After transplantation, the disease may recur.
Complications and their treatment • Osteoporosis • Varicose veins of the esophagus develop in a third of patients on average after 5.6 years, half subsequently experience bleeding • Other complications of liver cirrhosis • Infectious complications (sepsis).
Course and prognosis • The course is unpredictable • Life expectancy with asymptomatic course is about 10 years, with symptoms - about 7 years • Adverse prognostic factors in the presence of clinical manifestations - old age, hepatosplenomegaly, ascites, constant increase in bilirubin concentration more than 100 µmol/l ( life expectancy is no more than 2 years), the concentration of albumin in the blood serum is less than 30 g/l.
SECONDARY BILIARY CIRRHOSIS develops with long-term disruption of the outflow of bile (cholestasis) due to a pathological process in any area from the hepatocyte to the common bile duct.
Etiology • Mechanical obstruction of the bile ducts (usually extrahepatic) •• Stones of the common bile duct •• Cancer of the pancreas and papilla of Vater •• Benign strictures of the ducts •• Infections of the bile ducts •• Cholangiocarcinoma growing into the main intrahepatic ducts • Drug-induced hepatitis, cholestatic variant of the viral , alcoholic hepatitis • Taking oral contraceptives • Bile duct atresia • Sepsis • Byler family disease • Lymphogranulomatosis • Benign recurrent cholestasis • Amyloidosis
Pathomorphology • The liver is enlarged, green in color • Proliferation of the bile ducts • Ruptures of the interlobular bile ducts with the formation of “bile lakes” • Accumulation of copper in hepatocytes (in a non-toxic form) • Fibrosis is first periportal, then septa are formed and nodular regeneration of hepatocytes develops (biliary cirrhosis of the liver) .
Clinical picture • Skin itching • Jaundice • Malabsorption in the intestines, steatorrhea • Hypovitaminosis A, E, D, K • The liver is enlarged, hardened, painless • Splenomegaly at the stage of cirrhosis • Osteodystrophy (osteoporosis and osteomalacia) •• Bone pain •• Fractures with minimal trauma • Xanthomas, xanthelasmas, skin pigmentation • Feces are discolored, urine is dark.
Laboratory tests • Increased serum concentrations of direct bilirubin, alkaline phosphatase, cholesterol (not constant), lipoproteins • Direct bilirubin in the urine.
Instrumental studies • Ultrasound can detect dilation of the extrahepatic bile ducts, in this case, endoscopic retrograde or percutaneous transhepatic cholangiography is then performed; if there are no ductal lesions, a liver biopsy is necessary • If the extrahepatic ducts are not dilated on ultrasound, a liver biopsy is performed; If biopsy reveals changes in large ducts, cholangiography must be performed.
Treatment is aimed at eliminating the cause of cholestasis • Symptomatic treatment of cholestasis (see Primary sclerosing cholangitis) • Indications for surgical intervention (removal of stones, tumors, drainage of the biliary tract, anastomosis) are determined by the cause of obstruction and the patient’s condition.
Synonyms • Hypertrophic cirrhosis Ano • Cholangiolytic cirrhosis
ICD-10 • K74.3 Primary biliary cirrhosis • K74.4 Secondary biliary cirrhosis •• K74.5 Biliary cirrhosis, unspecified
Causes:
Due to their occurrence, there are 2 types of biliary cirrhosis:
- Primary biliary cirrhosis of the liver
- Secondary biliary cirrhosis of the liver
Primary biliary cirrhosis - the mechanism of occurrence is that autoimmune inflammation occurs in the liver tissue itself. Antibodies are produced against liver cells (hepatocytes) and they are perceived by the human body as foreign. The process itself is joined by a protective system, in the form of lymphocytes, macrophages, mast cells, which produce biologically active substances and antibodies. All of them together destroy hepatocytes, cause disturbances in blood supply, metabolism and bile stagnation, leading to general destruction of the architectonics (structure) of the liver.
- Genetic predisposition
- People suffering from autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, thyrotoxicosis, scleroderma, polyarteritis nodosa, sarcoidosis
- It is known from scientific sources that about 15% of cases of the disease are caused by an infectious substrate such as the herpes virus, rubella, Epstein-Barr
Secondary biliary cirrhosis of the liver occurs due to blockage or narrowing of the lumen of the intrahepatic bile ducts.
- Developmental anomalies (congenital or acquired) of the bile ducts and gallbladder
- Cholelithiasis
- Narrowing or blockage of the biliary tract after surgery on the abdominal organs, benign tumors
- External compression of the biliary tract by an inflamed pancreas or tumor
Complications
Intrahepatic cholestasis in primary biliary cirrhosis can cause a lack of bile in the intestine, which can be accompanied by steatorrhea (an increase in the amount of fatty components in the stool), the development of a deficiency of fat-soluble vitamins, impaired bone mineralization and, as a consequence, the occurrence of osteoporosis. As liver disease progresses, patients gradually lose weight and usually develop symptoms such as blurred vision, bone pain, bleeding gums, and possible pathological fractures.
Symptoms of biliary cirrhosis of the liver
Main nonspecific symptoms:
- Weakness
- Headache
- Dizziness
- Decreased appetite
- Impaired memory and attention
- Weight loss
- Apathy
- Sleep disturbance at night and drowsiness during the day
Symptoms of hepatocellular failure:
- Vomiting of intestinal contents
- Intense pain in the right hypochondrium
- Bloating
- Alternating diarrhea and constipation
- Jaundice (yellowing of the skin and mucous membranes)
- Itchy skin
- Darkening of urine
- Stool discoloration
- The appearance under the skin of the eyelids, ears and phalanges of the fingers of yellow tuberous inclusions (xanthemas)
- Enlarged liver and spleen
Symptoms of portal hypertension:
- “Jellyfish head” is a symptom that combines the presence of an enlarged abdomen and the presence of a pronounced venous network on the skin of the anterior abdominal wall
- Vomiting “coffee grounds” is a symptom that indicates bleeding from the veins of the esophagus or stomach
- “Tar” stool is a symptom indicating bleeding from the small intestine
- Dark red blood released from the rectum during defecation is a symptom indicating the presence of bleeding from hemorrhoidal veins located in the rectum
- Palmar erythema - redness of the palms
- The appearance of telangiectasias on the skin - spider veins
Diagnostics
NEARMEDIC clinics perform thorough diagnostics. The disease is detected in the early stages, when the disease can be brought under control, tissue can be restored, and progression can be interrupted. The initial appointment is carried out by an experienced gastroenterologist. The doctor establishes the clinical picture.
What tests are taken:
- general blood test (detects an increased content of leukocytes, a decrease in hemoglobin, platelets);
- biochemical blood test shows alkaline phosphatase, increased levels of bilirubin, ALT, AST, decreased albumin, high levels of potassium, urea, sodium, creatinine.
Hardware diagnostics and treatment
In NEARMEDIC clinics, modern ultrasound examination devices allow you to assess the condition of the organ: check the enlargement (accurately determine the size), see changes in the size of the spleen, evaluate the shape of the internal organs.
A computed tomography scan is performed to carefully examine the condition of the ducts, vessels, and tissues for damage. If a disease is suspected, Doppler measurements are performed to evaluate the blood vessels, and the doctor also recommends an MRI.
The most informative method is a biopsy: it best shows changes and the extent of organ damage. They will allow you to choose the most effective treatment method. Often, a diet, avoidance of harmful foods and drinks, and taking medications are sufficient for this.
Choose the clinic correctly so as not to pay too much for your health.
Review of drugs
Drug therapy only stops pathological processes in the digestive gland and does not lead to recovery. With the help of hepatoprotectors, antibiotics, diuretics and other medications, it is possible to reduce the severity of symptoms and thereby alleviate the patient’s condition. Biliary cirrhosis can be treated with the following drugs:
- cytostatics (“Aminosol”, “Decapeptyl”) - antitumor medications that prevent the formation of malignant tumors;
- choleretic drugs (“Nicodin”, “Hologon”) - increase the concentration of acids in bile and stimulate its production in the digestive gland;
antioxidants (“Essentiale”, “Complivit Selenium”) - neutralize harmful substances and free radicals in the body;- hepatoprotectors (“Heptral”, “Karsil”) - protect hepatocytes from the negative effects of toxins, antibodies and other substances;
- diuretics (“Spironol”, “Aldactone”) - promote the excretion of salts and toxic substances in the urine;
- anti-inflammatory drugs (“Essliver Forte”, “Kuprenil”) - reduce inflammation in the parenchyma, thereby slowing down the process of death of hepatocytes.
Irrational use of diuretics can lead to impaired renal function and the development of encephalopathy.
Treatment of cirrhosis
Treatment of cirrhosis involves:
- Treatment of the underlying disease that led to the development of cirrhosis;
- Specific therapy for complications, including medications: for example, the prescription of diuretics for ascites, the prescription of antibiotics for spontaneous bacterial peritonitis, etc.
- Surgical treatment of ascites and bleeding from dilated veins of the esophagus and stomach1
Important components are diet, exclusion of harmful effects on the liver, such as alcohol, hepatotoxic drugs, treatment of concomitant chronic diseases.4 If the measures taken are ineffective, organ transplantation is indicated1.