Published in the journal: “EFFECTIVE PHARMACOTHERAPY”; No. 45; 2015; pp. 14-18.
THEM. Korsunskaya1, E.V. Dvoryankova1, K.T. Plieva1, O.O. Melnichenko1, 2, S.V. Panyukova1, 2
1 Center for Theoretical Problems of Physicochemical Pharmacology
2 Moscow Scientific and Practical Center of Dermatovenereology and Cosmetology
The article discusses the pathogenesis of skin itching, possible psycho-emotional problems and somatic triggers of itching. The advantages of second-generation antihistamines, in particular cetirizine, are described: in addition to blocking H1-histamine receptors, the drug inhibits the migration of eosinophils in the area of inflammation and suppresses the skin response to platelet-activating factor. The results of our own studies showing the effectiveness of cetirizine in dermatological diseases are presented. Namely: maximum reduction in itching intensity within 3 hours after use during the first five days of therapy.
The skin makes up about 15% of the total human body weight and is the largest organ. Its most important function is protective.
The condition of the skin has a significant impact on a person’s self-esteem and the formation of interpersonal relationships. Itching is an unpleasant subjective sensation that causes the desire to scratch. This symptom in the vast majority of cases causes discomfort, psycho-emotional stress and exhaustion. In addition, scratching damages the integrity of the skin. It should be noted that, despite the high prevalence of the symptom, it has not been sufficiently studied due to the difficulties of its adequate assessment and the lack of models for research.
Somatic triggers of itching
Generalized itching that occurs without accompanying manifestations on the skin can be due to various reasons - from skin xerosis to endocrinological pathologies or carcinoma. That is why in clinical practice the assessment of this important prognostic symptom should not be neglected.
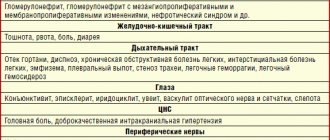
Relatively benign etiological factors include drug allergic reactions, dry skin, scabies and primary dermatological diseases. Most often, itchy skin occurs with dry skin. In older patients it is observed in 10-50% of cases [1]. Generalized itching occurs in 13% of patients with chronic renal failure and in 70-90% of those on hemodialysis [2]. Liver diseases accompanied by cholestasis (primary biliary cirrhosis, cholestasis caused by oral contraceptives, intrahepatic cholestasis during pregnancy, etc.) also often cause skin itching [2].
Hematological diseases that cause itching include polycythemia, iron deficiency anemia, endocrine diseases - thyrotoxicosis and diabetes mellitus [3].
Itching is a common clinical manifestation of AIDS and associated Kaposi's sarcoma and opportunistic infections. Thus, itching with or without skin rashes is observed in 84% of patients with AIDS, and in 35.5% of patients with Kaposi's sarcoma that developed against the background of AIDS. AIDS-associated opportunistic infections are accompanied by itching in 100% of cases [4].
It has been established that itchy skin can occur with malignant diseases. For example, with Hodgkin's lymphoma, itching is observed in 10-25% of patients, characterized by high intensity and limited localization, often on the lower legs. In some cases, this symptom precedes the diagnosis of lymphoma and may indicate a less favorable prognosis of the disease than fever or weight loss [4]. Adenocarcinomas and squamous cell cancer of various organs (stomach, pancreas, lungs, colon, brain, breast, prostate) are accompanied by itching in larger areas of the skin: on the legs, upper torso and extensor surfaces of the upper extremities. In this case, there is a direct relationship between the presence of itching and the activity/recurrence of cancer [4].
Secondary itching of the skin is usually associated with taking medications such as opium derivatives (cocaine, morphine, butorphanol), phenothiazines, tolbutamide, erythromycin, anabolic hormones, estrogens, progestins, testosterone, aspirin, quinidine and other antimalarial drugs, biological products ( monoclonal antibodies), vitamin B. In addition, it is known that itching can be a subclinical manifestation of hypersensitivity to any drug [5].
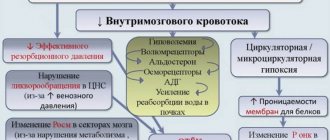
Since itching is observed not only in dermatological pathologies, it is advisable to conduct a thorough examination of the patient (Fig. 1) and treat patients taking into account the identified pathology.
Rice. 1. Algorithm for diagnosing skin itching
Diagnostics
Anamnesis
- Localization : focal or generalized.
- Onset : acute onset is the least characteristic of systemic diseases.
- Duration.
- Nature/character : severe, constant itching, worsening in the evening - scabies;
- “burning” itching – perpetiform dermatitis;
- “tingling” – polycythemia.
Physical examination
- Careful examination of the skin: primary lesions;
- excoriation of the skin in various areas (pediculosis, scabies);
- inflammatory papules on the legs with a small vesicle in the center (flea bites);
- “butterfly” sign in the upper central part of the back (hepatobiliary pathology);
- uremic chills.
Laboratory research
Complete blood count with leukoformula, urea, creatinine, liver tests (markers of cholestasis - alkaline phosphatase, gamma-glutamyl transpeptidase (GGT), determination of bilirubin), thyroxine (T-4) and thyroid-stimulating hormone (TSH), blood glucose.
Mechanisms of development and relief of itching
Hypotheses about the mechanisms of development of itching have been formulated based on studies of the pathophysiology of pain, since pain and itching share common molecular and neurophysiological mechanisms.
The sensation of both itching and pain results from the activation of a network of free nerve endings in the dermal-epidermal zone. The triggering mechanism is the influence of internal or external thermal, mechanical, chemical stimuli or electrical stimulation. Cutaneous nerve irritation can be mediated by several biological agents, including histamine, vasoactive peptides, enkephalins, substance P, and prostaglandins.
It is believed that other, non-anatomical factors, such as psycho-emotional stress, individual subjective perception, the presence and intensity of other sensations and/or distractions, have a significant impact on the degree of sensitivity of itching in different areas of the skin.
The nerve impulse that causes the sensation of itching, which arose under the influence of any of the listed factors, is transmitted through the same neural connection as pain impulses: from peripheral nerve endings to the dorsal horns of the spinal cord, through the anterior commissure, along the spinothalamic tract to the contralateral laminar nucleus of the thalamus. It is hypothesized that the thalamocortical tertiary neuron tract acts as a “relay” for impulse transmission through the integration of the thalamic reticular activating system in several brain regions. In response, there is a desire to scratch the skin, which is formed in the corticothalamic center and is realized in the form of a spinal reflex. After scratching, skin itching occurs again after 15-25 minutes. However, in some cases, especially in patients with chronic dermatoses, the itching sensation after scratching does not stop, which leads to excoriation.
Despite the fact that many etiological and pathogenetic factors contributing to the occurrence of itching are currently known, their study continues and new mechanisms of its development are being discovered.
The mechanism by which itching is relieved by scratching has not been reliably established. It is possible that during scratching, sensory impulses are generated that interrupt the neural arc responsible for the occurrence of sensation.
In addition to scratching, vibration, injections into the itchy area, exposure to heat, cold, and ultraviolet radiation help reduce itching [3].
Pharmacotherapy of hay fever consists of the use of pharmacological agents aimed at eliminating the main symptoms of rhinitis, conjunctivitis, and bronchial asthma. In pharmacotherapy of AR, in turn, the following groups of drugs are used: antihistamines (inverse agonists of H1 receptors), glucocorticosteroids, mast cell membrane stabilizers (cromones), vasoconstrictors (decongestants), less often - anticholinergics, antileukotriene drugs, monoclonal anti-IgE antibodies (Table 2).
Pathophysiology
Signals for pain and itching caused by skin causes are transmitted along the same pathways, but the afferent C-fibers differ functionally: one part of the nerve fibers is stimulated by histamine, the other by other substances that cause itching (for example, serotonin). There is evidence of similarities between neuropathic pain, itch and cough. Their common property is peripheral and central sensitization of the afferent nervous system. This explains the effectiveness of antiepileptic drugs and antidepressants for such a variety of conditions, as well as the ineffectiveness or low effectiveness of H1 blockers for some types of itch.
Mechanisms and mediators involved in the formation of the sensation of itching:
- amines (histamine, serotonin, acetylcholine);
- proteases and kinins (tryptase, chymase, kallikrein, bradykini, etc.);
- neuropeptides (substance P, neurotensin, etc.);
- cytokines (prostaglandin E reduces the threshold for susceptibility to itching);
- opioid receptors (metenkephalin, leuenkephalin, β-endorphin), naloxone reduces itching, opiates relieve pain but increase itching.
Treatment
Therapeutic treatment methods should be aimed primarily at eliminating pathogenetic factors.
Patients are shown sedatives (especially with intense chronic itching), emollients (to reduce dry skin, which is both a cause and a consequence of itching), topical distraction agents (cold lotions, menthol-containing products, etc.), antihistamines, which In the vast majority of cases, they are first-line drugs.
There are two generations of antihistamines: sedative (Suprastin, Tavegil, Diazolin, Diphenhydramine, Fenkarol, Fenistil) and non-sedating/weak sedative (cetirizine, levocetirizine, loratadine, desloratadine, fexofenadine, ebastine, rupatadine).
It is important to note that, despite the need to take sedatives, it is better not to use first-generation antihistamines (which have a sedative effect in addition to antihistamines). Firstly, sleep when using them is unphysiological (the drugs inhibit the REM sleep phase). Secondly, the multiple side effects characteristic of this group of drugs limit their use in a large group of patients with concomitant diseases. Therefore, it is better to use tranquilizers as sedatives, and when choosing antihistamines, preference should be given to second-generation blockers.
Cetirizine occupies a special place among them.
Useful tips
Systemic treatment is often not necessary if the skin condition improves.
If your skin becomes dry, stop using soap; bathing in warm rather than hot water, lubricating the skin after bathing and at night, applying a damp cloth for 15–20 minutes, then applying cream or ointment.
For damp skin - protective cream (zinc paste), drying dressings with Burov's liquid (aluminum acetate 8%, diluted 1:10–1:20).
Local anti-itch remedies
Zinc oxide has anti-inflammatory, antiseptic and antipruritic effects, and is used in concentrations of 10–50% in creams, liniments, lotions, ointments and pastes that are effective in the treatment of localized forms of itching.
Menthol, when applied to the skin and mucous membranes, dilates blood vessels, causing a feeling of coldness and then numbness, significantly reducing itching. It is used in powders, ointments, and lotions in concentrations of 1–10%.
Camphor , when applied to the skin, produces a warm sensation followed by mild anesthesia, which reduces itching. It is used in the form of liniments, lotions and ointments in concentrations of 2–20%.
Important
It should be remembered that products with menthol and camphor cannot be used simultaneously on one area of the skin.
Calamine , a lotion containing zinc carbonate (calamine), zinc oxide and a small amount of phenol, is widely used in the treatment of itching and atopic dermatitis.
Cetirizine
Cetirizine inhibits the histamine-mediated early phase of the allergic reaction, prevents various physiological and pathophysiological effects of histamine, such as dilation and increased capillary permeability (development of edema, urticaria, redness), stimulation of sensory nerve endings (itching, pain) and contraction of smooth muscles of the respiratory and gastrointestinal tract. intestinal tract.
In the late stage of an allergic reaction, cetirizine not only inhibits the release of histamine, but also the migration of eosinophils and other cells, thereby attenuating the late allergic reaction. Reduces the expression of adhesion molecules, such as intercellular adhesion molecule-1 (ICAM-1) and vascular cellular adhesion molecule-1 (VCAM-1), which are markers allergic inflammation.
In addition, unlike other drugs used for skin manifestations of allergies, cetirizine not only blocks H1-histamine receptors, but also suppresses the skin response to platelet-activating factor [6, 7]. This is confirmed by the results of numerous clinical comparative studies: the ability to accumulate in the skin allows the drug to relieve itching and hyperemia more effectively than drugs such as ebastine, epinastine, terfenadine, fexofenadine and loratadine [8-10].
Cetirizine has a low volume of distribution compared to other antihistamines - 0.5 l/kg. This provides higher concentrations of the substance in the extracellular space, where H1-histamine receptors are located. This ensures their full employment and the highest antihistamine effect [11]. Another feature of the drug is its high ability to penetrate the skin. 24 hours after taking a single dose of cetirizine, the concentration in the skin is equal to or even slightly higher than the concentration in the blood. The advantage of cetirizine is its steroid-sparing effect: with the simultaneous administration of cetirizine and inhaled glucocorticosteroids in patients with bronchial asthma, the dose of the latter can be reduced or not increased, despite contact with the allergen.
Among cetirizines, Cetrin occupies a special place. In the study by E.E. Nekrasova et al. in patients with chronic urticaria, Cetrin showed the highest effectiveness among other generic cetirizine and the best results in terms of pharmacoeconomics [12].
Care Tips
- Prevention of scratching: short-filed nails, lightly rubbing itchy areas.
- After washing, dry your skin carefully using wet movements, use a soft towel or a hair dryer on a cold setting.
- Avoid long hot baths. Try a bath with sodium bicarbonate (baking soda) or medicated oils.
- Use loose clothing and loose bedding/blankets.
- Avoid overheating and sweating, especially during night sleep.
- Increase the humidity in the bedroom so that your skin loses less moisture.
- Wear cotton gloves at night to prevent scratching.
- Avoid damaging the skin with alcohol-containing rubbing, woolen clothing, and excessive hygiene procedures.
- Cleanse your skin gently using moisturizers.
- Use cooling, soft compresses.
- You can use an anesthetic mixture: aftershave cream with menthol 50 ml, Diphenhydramine 1% 3–5 ml, Lidocaine 2% 1–2 ml, Novocaine 0.5% 5–10 ml. Mix and serve chilled.
- Use relaxation and positive visualization techniques.
Application experience
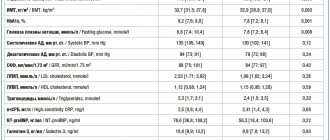
Under our supervision there were 75 patients aged from 18 to 76 years (34 men and 41 women) with diagnoses of “atopic dermatitis”, “allergic dermatitis”, “chronic eczema in the acute stage”, “lichen planus”, “toxidermia” ( Fig. 2).
Rice. 2. Distribution of patients by nosology
All patients received topical and systemic therapy, including the antihistamine Cetrin (cetirizine) at a dose of 10 mg once a day at night. The duration of therapy is from 14 to 21 days, depending on the diagnosis. Patients assessed the effectiveness of itching relief using a point system: 0 points - no itching, 1 point - mild itching (present, but not bothersome), 2 points - moderate (bothering, but does not interfere with daily activity and/or sleep), 3 points - severe /intense itching (disturbs and interferes with daily activity and/or sleep).
The maximum reduction in itching intensity was observed within 3 hours of taking the drug in the first five days (Fig. 3).
Rice. 3. Average subjective assessment of the intensity of itching after using the drug
Subsequently, a decrease in itching or its absence was noted by the 10th day of therapy, with a simultaneous decrease in the clinical manifestations of the disease (Fig. 4).
Rice. 4. Dynamics of clinical manifestations
The results obtained demonstrate the high effectiveness of Cetrin (cetirizine) in the treatment of chronic and acute dermatoses. Cetrin (cetirizine) has a pronounced antipruritic effect, and also reduces other clinical manifestations of allergic dermatoses (infiltration, erythema). In addition, the drug can also be used for somatic diseases as symptomatic therapy.
Bibliography:
- Duncan WC, Fenske NA Cutaneous signs of internal disease in the elderly // Geriatrics. 1990. Vol. 45. No. 8. P. 24-30.
- Masmoudi A., Hajjaji Darouiche M., Ben Salah H. et al. Cutaneous abnormalities in patients with end stage renal failure on chronic hemodialysis. A study of 458 patients // J. Dermatol. Case Rep. 2014. Vol. 8. No. 4. P. 86-94.
- Abel EA, Farber EM Malignant cutaneous tumors // Scientific American Medicine / eds. E. Rubenstein, D. D. Federman. Section XII. New York: Scientific American, Inc., 1992. P. 1-20.
- Dangel RB Pruritus and cancer // Oncol. Nurs. Forum. 1986. Vol. 13. No. 1. P. 17-21.
- Bernhard JD Clinical aspects of pruritus // Dermatology in General Medicine / eds. T.B. Fitzpatrick, A.Z. Eisen, K. Wolff et al. 3rd ed. Chapter 7. New York: McGraw-Hill, 1987. P. 78-90.
- Smirnova G.I. Antihistamines in the treatment of allergic diseases in children. M., 2004.
- Gushchin I.S. Cetirizine is a standard H1-antihistamine // Mistetstvo Likuvannya. 2009. No. 5. P. 60-70.
- Belsito D. Second-generation antihistamines for the treatment of chronic idiopathic urticaria // J. Drugs Dermatol. 2010. Vol. 9. No. 5. P. 503-512.
- Grant J., Riethuisen J., Moulaert B., DeVos C. A double-blind, randomized, single-dose, crossover comparison of levocetirizine with ebastine, fexofenadine, loratadine, mizolastine, and placebo: suppression of histamine-induced wheal-and -flare response during 24 hours in healthy male subjects // Ann. Allergy Asthma Immunol. 2002. Vol. 88. No. 2. P. 190-197.
- Kavosh E., Khan D. Second-generation H1-antihistamines in chronic urticaria: an evidence-based review // Am. J. Clin. Dermatol. 2011. Vol. 12. No. 6. P. 361-376.
- Volosovets A.P., Krivopustov S.P., Pavlik E.V. The role of allergic inflammation in everyday medical practice. Optimization of antiallergic therapy // Medical literature (Kyiv). 2010. No. 1. P. 70-75.
- Nekrasova E.E., Ponomareva A.V., Fedoskova T.G. Rational pharmacotherapy of chronic urticaria // Russian Allergological Journal. 2013. No. 6. P. 69-74.
Possible causes of itchy body skin: which doctor to consult
Itchy skin is an unpleasant sensation accompanied by the need for mechanical irritation of the skin, that is, it causes a constant desire to scratch the disturbing area. The types of skin itching depend on the reasons that provoked it. Itching is a symptom of various diseases, disorders and conditions. It can be the result of infection, inflammation, allergies, insect bites, or occur during the normal wound healing process. Itching significantly affects the general condition and quality of life of patients. It causes insomnia and, in severe cases, leads to depression.
The skin on your hands is very dry, flaky and itchy
Other possible causes of itchy body skin:
- Scabies. The disease is caused by female scabies mites. An infected person is bothered by intense skin itching, which intensifies after a hot shower, in the evening and at night.
- Head and pubic lice.
- Insect bites: bees, wasps, mosquitoes, fleas, bedbugs.
The skin of the hands is very dry, flaky and itchy - a condition characteristic of a fungal infection, and can also signal a metabolic disorder or result from contact with aggressive environments. A dermatologist must make an accurate diagnosis and prescribe treatment.
Why does the skin on my legs itch and redness appear? Symptoms may indicate either a skin or allergic disease, or an endocrine or autoimmune pathology.
Itching may be a symptom of infection:
- Chickenpox or other viral infection.
- A fungal infection (athlete's foot) that causes itching between the toes.
- Ringworm.
- Vaginal candidiasis, causing itching of the genitals and surrounding skin (inner thigh).